When a patient is experiencing a stroke, time is of the essence. For every minute that passes, the brain loses critical blood flow and proper oxygenation. Frequently, the verbiage is "time lost is brain lost." This course will outline the NIH Stroke Scale and why its use is significant. Learners will be able to identify components of the Scale, perform the Scale with proper scoring, and educate colleagues regarding the Scale.
This course is designed for physicians, physician assistants, and nurses involved in the assessment and care of patients with suspected stroke.
The purpose of this course is to provide clinicians with a clear understanding of the National Institute of Health (NIH) Stroke Scale, including proper administration and consistent scoring, with the ultimate goal of improving patient outcomes.
Upon completion of this course, you should be able to:
- Define the NIH Stroke Scale and why it is used.
- Identify the articles of the stroke scale.
- Identify proper scoring of the NIH Stroke Scale.
- Educate colleagues on the NIH Stroke Scale.
Mary Franks, MSN, APRN, FNP-C, is a board-certified Family Nurse Practitioner and NetCE Nurse Planner. She works as a Nurse Division Planner for NetCE and a per diem nurse practitioner in urgent care in Central Illinois. Mary graduated with her Associate’s degree in nursing from Carl Sandburg College, her BSN from OSF Saint Francis Medical Center College of Nursing in 2013, and her MSN with a focus on nursing education from Chamberlain University in 2017. She received a second master's degree in nursing as a Family Nurse Practitioner from Chamberlain University in 2019. She is an adjunct faculty member for a local university in Central Illinois in the MSN FNP program. Her previous nursing experience includes emergency/trauma nursing, critical care nursing, surgery, pediatrics, and urgent care. As a nurse practitioner, she has practiced as a primary care provider for long-term care facilities and school-based health services. She enjoys caring for minor illnesses and injuries, prevention of disease processes, health, and wellness. In her spare time, she stays busy with her two children and husband, coaching baseball, staying active with her own personal fitness journey, and cooking. She is a member of the American Association of Nurse Practitioners and the Illinois Society of Advanced Practice Nursing, for which she is a member of the bylaws committee.
Contributing faculty, Mary Franks, MSN, APRN, FNP-C, has disclosed no relevant financial relationship with any product manufacturer or service provider mentioned.
John M. Leonard, MD
Sharon Cannon, RN, EdD, ANEF
The division planners have disclosed no relevant financial relationship with any product manufacturer or service provider mentioned.
Sarah Campbell
The Director of Development and Academic Affairs has disclosed no relevant financial relationship with any product manufacturer or service provider mentioned.
The purpose of NetCE is to provide challenging curricula to assist healthcare professionals to raise their levels of expertise while fulfilling their continuing education requirements, thereby improving the quality of healthcare.
Our contributing faculty members have taken care to ensure that the information and recommendations are accurate and compatible with the standards generally accepted at the time of publication. The publisher disclaims any liability, loss or damage incurred as a consequence, directly or indirectly, of the use and application of any of the contents. Participants are cautioned about the potential risk of using limited knowledge when integrating new techniques into practice.
It is the policy of NetCE not to accept commercial support. Furthermore, commercial interests are prohibited from distributing or providing access to this activity to learners.
Supported browsers for Windows include Microsoft Internet Explorer 9.0 and up, Mozilla Firefox 3.0 and up, Opera 9.0 and up, and Google Chrome. Supported browsers for Macintosh include Safari, Mozilla Firefox 3.0 and up, Opera 9.0 and up, and Google Chrome. Other operating systems and browsers that include complete implementations of ECMAScript edition 3 and CSS 2.0 may work, but are not supported. Supported browsers must utilize the TLS encryption protocol v1.1 or v1.2 in order to connect to pages that require a secured HTTPS connection. TLS v1.0 is not supported.
The role of implicit biases on healthcare outcomes has become a concern, as there is some evidence that implicit biases contribute to health disparities, professionals' attitudes toward and interactions with patients, quality of care, diagnoses, and treatment decisions. This may produce differences in help-seeking, diagnoses, and ultimately treatments and interventions. Implicit biases may also unwittingly produce professional behaviors, attitudes, and interactions that reduce patients' trust and comfort with their provider, leading to earlier termination of visits and/or reduced adherence and follow-up. Disadvantaged groups are marginalized in the healthcare system and vulnerable on multiple levels; health professionals' implicit biases can further exacerbate these existing disadvantages.
Interventions or strategies designed to reduce implicit bias may be categorized as change-based or control-based. Change-based interventions focus on reducing or changing cognitive associations underlying implicit biases. These interventions might include challenging stereotypes. Conversely, control-based interventions involve reducing the effects of the implicit bias on the individual's behaviors. These strategies include increasing awareness of biased thoughts and responses. The two types of interventions are not mutually exclusive and may be used synergistically.
#90380: The NIH Stroke Scale
Approximately 795,000 strokes occur in the United States each year. An average, an individual has a stroke every 40 seconds in the United States, and every 3 minutes and 14 seconds, an individual dies as a result of stroke [1].
A stroke occurs when the blood supply is blocked to the brain, either by a physical blockage (such as plaque in an artery loosening and completely blocking the artery) or a vessel rupture causing hemorrhage within the brain. When this blockage occurs, damage to the brain occurs, leading to potential long-term disability or death [2].
When a patient is experiencing a stroke, time is of the essence. For every minute that passes, the brain loses critical blood flow and proper oxygenation. Frequently, the verbiage is "time lost is brain lost" [2]. This course will outline the NIH Stroke Scale and why its use is significant. Learners will be able to identify articles within the NIH Stroke Scale, perform the NIH Stroke Scale with proper scoring, and educate colleagues on the NIH Stroke Scale.
Stroke scales have evolved since the late 1980s. The first widely used scales included the Cincinnati Prehospital Stroke Severity Scale (CP-SSS), the Canadian Neurological Scale (CNS), the Edinburgh-2 Coma Scale, and the Oxbury Initial Severity Scale (OISS). With all of these, the greater the score, the larger infarct present. The NIH Stroke Scale (NIHSS) has evolved for the initial plan, which appeared in a naloxone trial for acute stroke [3].
The current NIHSS consists of 11 components, a decrease from the original 15. An even further modified form including only eight components was developed for quick assessments in emergency settings. For standard purposes, the 11-component NIHSS is the ideal tool [3,4]. The NIHSS was most recently updated in June 2016 [5].
As mentioned, the NIH stroke scale consists of 11 components [4,5]:
Level of consciousness (LOC)
LOC Instructions
LOC Questions
LOC Commands
Best gaze
Visual
Facial palsy
Motor arm
Motor leg
Limb ataxia
Sensory
Best language
Dysarthria
Extinction and inattention (formerly neglect)
Each component is paired with specific instructions, and scoring is based assessment of each section.
To obtain most accurate scoring with the NIHSS, the items should be assessed in the order listed. The patient's performance or response to each component should be fully recorded, and no items should be changed or rescored as the assessment progresses. The score is a reflection of how the patient performs the task or test, not how the provider perceives the patient performing each test. Ideally, the patient should not be coached during the exam [4,5].
LOC Instructions
Level of consciousness is assessed by observation. If the patient has a barrier to clear communication (e.g., an endotracheal tube, language barrier, orotracheal damage), the provider administering the exam should choose a response [4,5]. This item is scored as follows [4,5]:
0 : Alert; keenly responsive
1: Not alert, but arousable by minor stimulation to obey, answer, or respond
2: Not alert; requires repeated stimulation to attend, or is obtunded and requires strong or painful stimulation to make movements (not stereotyped)
3: Responds only with reflex motor or autonomic effects, or totally unresponsive, flaccid, and areflexic
LOC Questions
In this test, the provider asks the patient the current month along with his or her current age. Patients who are aphasic (a language disorder caused by a stroke) or stuporous (needing frequent stimuli to maintain arousal) automatically score a 2 [7,8]. Patients who are intubated or otherwise unable to verbally communicate due to orotracheal trauma, dysarthria from any cause, language mismatch, or any other problem not secondary to aphasia are automatically given a 1 for a score. The provider performing the exam should not coax the patient with any verbal or nonverbal cues [4,5]. This item is scored as follows [4,5]:
0: Answers both questions correctly
1 = Answers one question correctly
2 = Answers neither question correctly
LOC Commands
In testing LOC commands, the patient is asked to open and close their eyes. The patient will also be asked to grip and release the nonparetic (non-paralyzed) hand [8]. If the hands are not able to be used, another one-step test may be substituted. The patient can receive credit for the test if the attempt is made but cannot be completed due to weakness. If the patient does not respond to the command request, the provider may demonstrate to the patient, and the response is recorded as following none, one, or two commands [4,5]. This item is scored as follows [4,5]:
0: Performs both tasks correctly
1: Performs one task correctly
2: Performs neither task correctly
For this assessment, only horizontal gaze is tested and consists of voluntary and reflexive eye movements. If the patient has a conjugate deviation that can be overcome with voluntary or reflexive eye movements, the score will be recorded as a 1. If there is observed paralysis of cranial nerves III, IV, or VI, the score is also 1. In patients with ocular trauma, bandages, pre-existing blindness, or other disorders of visual acuity, testing with reflexive movements is recommended. Testing can be completed on all aphasic patients. This item is scored as follows [4,5]:
0: Normal
1: Partial gaze palsy; gaze is abnormal in one or both eyes, but forced deviation or total gaze paresis is not present
2: Forced deviation, or total gaze paresis is not overcome by the oculocephalic maneuver
Visual fields are tested by confrontation, using finger counting or visual threat, whichever is most appropriate for the patient. In this particular test, encouragement of the patient is allowed. For those with unilateral blindness or enucleation, the item is scored according to the remaining visual fields. A score of 1 is indicative of clear asymmetry. If the patient is found to have blindness from any cause, a score of 3 is given. If there is blindness, double simultaneous stimulation is performed. If extinction exists, the score is a 1, and the result is used to answer item 11. This item is scored as follows [4,5]:
0: No visual loss
1: Partial hemianopia
2: Complete hemianopia
3: Bilateral hemianopia (blindness, including cortical blindness)
When checking facial palsy, the patient will be asked to show their teeth, raise their eyebrows, and close their eyes. If the patient is minimally responsive and grimaces to noxious stimuli, the symmetry response is scored. If the patient has physical barriers obscuring the face, such as orotracheal tubes or facial trauma, an attempt should be made to remove or address these barriers prior to assessing facial palsy. This item is scored as follows [4,5]:
0: Normal, symmetrical movements
1: Minor paralysis (e.g., flattened nasolabial fold, asymmetry on smiling)
2: Partial paralysis (total or near-total paralysis of lower face)
3: Complete paralysis of one or both sides (absence of facial movement in the upper and lower face)
When assessing function of the arms in patients with suspected stroke, the arms are extended with palm side down. If the patient is sitting, the arms are held at 90 degrees; if lying down, the arms are extended at 45 degrees. A pronator drift is scored greater than a 0 if an arm falls before 10 seconds on either side. Ideally, the arms are tested in turn, starting with the nonparetic side. A score of untestable (UN) should be made only if there is an amputation or joint fusion contributing to loss of function. The testing provider should also clearly document the reason for the UN score. This item is scored as follows [4,5]:
0: No drift; limb holds 90 (or 45) degrees for full 10 seconds
1: Drift; limb holds 90 (or 45) degrees, but drifts down before full 10 seconds without hitting the bed or other support
2: Some effort against gravity; limb cannot get to or maintain (if cued) 90 (or 45) degrees, drifts down to bed, but has some effort against gravity
3: No effort against gravity; limb falls
4: No movement
Untestable (UN): Amputation or joint fusion (provide further explanation)
The legs are tested in the supine position, with a leg lifted and held at 30 degrees. A drift is scored if the leg starts to fall before five seconds. As with the arms, each leg is tested in turn, beginning with the nonparetic leg. UN can also be applied with motor leg test scoring, with clear documentation of why this score was chosen. This item is scored as follows [4,5]:
0: No drift; leg holds 30-degree position for full five seconds
1: Drift; leg falls by the end of the five-second period but does not hit the bed
2: Some effort against gravity; leg falls to bed by five seconds but has some effort against gravity
3: No effort against gravity; leg falls to bed immediately
4: No movement
Untestable (UN): Amputation or joint fusion (provide further explanation)
Limb ataxia testing is used to identify a unilateral cerebellar lesion. Finger-nose-finger testing and heel-shin testing is used and assessed on both sides; the patient's eyes should remain open. Ataxia is scored only if it is present and out of proportion to weakness. A score of 0 is given if the patient cannot understand or is paralyzed. UN is used in cases of amputation or joint fusion. If the patient is blind, he or she should perform the test of finger to nose with the arm extended as the starting point. This item is scored as follows [4,5]:
0: Absent
1: Present in one limb
2: Present in two limbs
Untestable (UN): Amputation or joint fusion (provide further explanation)
For the sensory dimension, the patient's sensation or grimace to pinprick or withdrawal from noxious stimulus in the obtunded or aphasic patient is assessed. Only sensory loss attributed to stroke is scored as abnormal, and the examiner should test as many body areas (e.g., arms [not hands], legs, trunk, face) as needed to accurately evaluation potential hemisensory loss. A score of 2 should only be given when a severe or total loss of sensation can be clearly demonstrated. Therefore, stuporous and aphasic patients will probably score 1 or 0. Patients with brainstem stroke who have bilateral loss of sensation are scored 2, as are patients who are quadriplegic or are in a coma. This item is scored as follows [4; 5]:
0: Normal; no sensory loss
1: Mild-to-moderate sensory loss. Patient feels pinprick is less sharp or is dull on the affected side, or there is a loss of superficial pain with pinprick, but patient is aware of being touched.
2: Severe to total sensory loss. Patient is not aware of being touched in the face, arm, and leg.
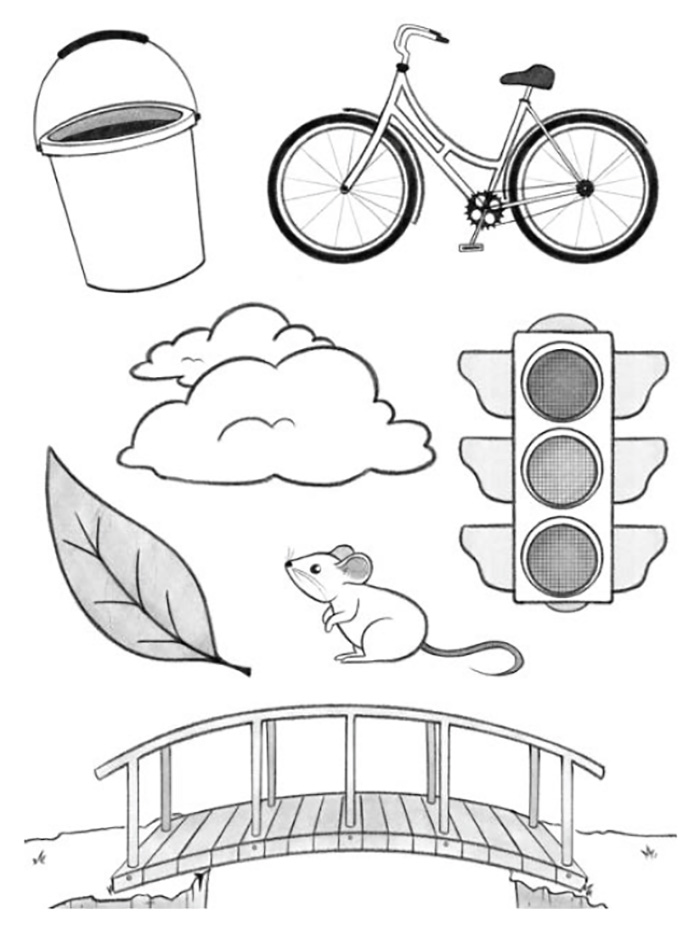
Assessment of language differs slightly from the other dimensions. The patient is asked to describe what is happening in the images from the NIH Stroke Scale manual (Figures 1 and 2) and to read from the list of words and sentences provided in the manual. The ability of the patient to perform the test is assessed based on the responses to these prompts as well as to all the commands in the preceding general neurological exam. If visual loss hinders the tests, the patient is asked to identify objects placed in the hand and to repeat and produce speech. Intubated patients should be asked to write, if able. Patients who scored a 3 on item 1a (i.e., responds only with reflex motor or autonomic effects, or totally unresponsive, flaccid, and areflexic) will automatically be scored with a 3 for this item as well. The examiner must choose a score for the patient with stupor or limited cooperation. A score of 3 should be used only if the patient is mute and does not follow one-step commands. This item is scored as follows [4,5]:
0: No aphasia; normal
1: Mild-to-moderate aphasia; some obvious loss of fluency or facility of comprehension, without significant limitation on ideas expressed or form of expression. Reduction of speech and/or comprehension, however, makes the conversation about provided materials difficult or impossible. For example, in a conversation about provided materials, the examiner can identify picture or naming card content from the patient's response.
2: Severe aphasia; all communication is through fragmentary expression; great need for inference, questioning, and guessing by the listener. The range of information that can be exchanged is limited; the listener carries the burden of communication. The examiner cannot identify the materials provided from the patient's response.
3: Mute, global aphasia; no usable speech or auditory comprehension
For this dimension, the patient will be asked to read and repeat the words from the NIH Stroke Scale manual. If the patient is thought to have no deficits, an adequate speech sample must be obtained. If severe aphasia is identified, the clarity of articulation of the patient's spontaneous speech can be rated. The patient who is intubated or has other physical barriers to producing speech (e.g., trauma) should have a recorded score as UN, again with a clear explanation for this choice. If possible, the patient should not be made aware they are being tested. This item is scored as follows [4,5]:
0: Normal
1: Mild-to-moderate dysarthria; patient slurs at least some words and, at worst, can be understood with some difficulty
2: Severe dysarthria; patient's speech is so slurred as to be unintelligible in the absence of or out of proportion to any dysphasia, or is mute/anarthric
Untestable (UN): Intubated or other physical barrier (provide further explanation)
Adequate information to discover extinction and inattention may be acquired during the assessment of all of the prior dimensions. If the patient has severe visual loss preventing visual double simultaneous stimulation and cutaneous stimuli are normal, the score is recorded as normal (0). If the patient has aphasia but does appear to attend to both sides, the score is also normal. The presence of visual-spatial neglect or anosognosia may also be taken as evidence of abnormality. There is not an option to score UN for this item. This item is scored as follows [4,5]:
0: No abnormality
1: Visual, tactile, auditory, spatial, or personal inattention, or extinction to bilateral simultaneous stimulation in one of the sensory modalities
2: Profound hemi-inattention or extinction to more than one modality; does not recognize own hand or orients to only one side of space
A copy of the current NIH Stroke Scale may be accessed online at https://www.ninds.nih.gov/sites/default/files/2024-05/KnowStroke_NIHStrokeScale_May2024_508c.pdf.
All providers who might use or evaluate results of the NIH Stroke Scale, including nurses, nurse practitioners, physician assistants, and physicians, should have clear education regarding the appropriate use in order to ensure consistent and accurate scoring. Unfortunately, one study demonstrated that one in three patients had a difference of two points or greater when scored by a registered nurse compared with a neurologist. The greatest scoring inconsistencies were among patients with documented aphasia. Researchers from this study concluded that NIH Stroke Scale training requirements may be contributory to the scoring differences [9]. It is imperative that those administering the Scale perform it in the same manner using the same scoring technique. Consistency in scoring translates to accuracy of the patient assessment and can provide guidance for further testing, imaging, and treatment as indicated [9].
Training on administration of the NIH Stroke Scale is not mandatory for physicians; however, nurses who work in the emergency department, intensive care unit, or neurological unit are required to take training and to be certified through the NIH annually. This requirement is for facilities that are considered primary stroke centers (PSC) certified by The Joint Commission [9].
Early diagnosis and appropriate immediate treatment are key to the recovery of neurologic function and survival after stroke, making it imperative for both healthcare professionals and the general public to recognize the symptoms of stroke and stroke-like symptoms. Clinicians and all staff involved in the care of patients with suspected stroke should be skilled in identifying and documenting possible stroke-related symptoms. Efforts to educate the public about the importance of seeking medical care for stroke-related symptoms and about the warning signs of stroke are also essential.
The NIH Stoke Scale is a resourceful tool to determine the extent to which patients are affected by a neurological event or stroke, and it can be administered in only a matter of minutes. Minimizing between-clinician differences in scoring is also essential. While the Scale has evolved over the years, standardized use can help to guide the course of treatment and follow-up to ensure optimal patient outcomes.
1. Centers for Disease Control and Prevention. Stroke Facts. Available at https://www.cdc.gov/stroke/data-research/facts-stats/?CDC_AAref_Val=https://www.cdc.gov/stroke/facts.htm.Last accessed October 15, 2024.
2. Centers for Disease Control and Prevention. About Stroke. Available at https://www.cdc.gov/stroke/about/?CDC_AAref_Val=https://www.cdc.gov/stroke/about.htm. Last accessed October 15, 2024.
3. Lyden P. Using the National Institutes of Health Stroke Scale: a cautionary tale. Stroke. 2017;48(2):513-519.
4. National Institute of Neurological Disorders and Stroke. NIH Stroke Scale. Available at https://www.ninds.nih.gov/health-information/stroke/assess-and-treat/nih-stroke-scale Last accessed October 17, 2024.
5. National Institute of Neurological Disorders and Stroke. NIH Stroke Scale. Available at https://www.ninds.nih.gov/sites/default/files/2024-05/KnowStroke_NIHStrokeScale_May2024_508c.pdf. Last accessed October 15, 2024.
6. Johns Hopkins Medicine. Aphasia. Available at https://www.hopkinsmedicine.org/health/conditions-and-diseases/aphasia. Last accessed October 15, 2024.
7. Tindall SC. Level of consciousness. In: Walker HK, Hall WD, Hurst JW (eds). Clinical Methods: The History, Physical, and Laboratory Examinations. 3rd ed. Boston, MA: Butterworths; 1990.
8. Merriam-Webster. Paretic. Available at https://www.merriam-webster.com/medical/paretic. Last accessed October 15, 2024.
1. Powers WJ, Rabinstein AA, Ackerson T, et al. Guidelines for the early management of patients with acute ischemic stroke: 2019 update to the 2018 guidelines for the early management of acute ischemic stroke: a guideline for healthcare professionals from the American Heart Association/American Stroke Association. Stroke. 2019;50(12):e344-e418. Available at https://www.ahajournals.org/doi/10.1161/STR.0000000000000211. Last accessed October 21, 2024.
Mention of commercial products does not indicate endorsement.