The impact of nutrition on the caries process is known in the dental field, but dental professionals need to continue to convey the importance of this relationship to patients. Working as partners with patients, dental professionals can aid in the prevention of dental caries and help maintain patients' overall health by offering nutritional counseling and behavior modification techniques. The incidence of caries in the United States could decrease significantly as dental professionals implement the advances available for early caries detection, recommend anticaries treatments, and offer nutritional analysis and counseling.
This course is designed for dental professionals involved in the prevention and treatment of caries.
The purpose of this course is to equip all members of the dental team with the skills needed to implement the advances available for early caries detection, recommend anticaries treatments, and offer nutritional analysis and counseling.
Upon completion of this course, you should be able to:
- Describe the caries process and methods for its detection.
- List the oral care habits recommended by the American Dental Association.
- Identify the dietary choices of patients and the factors that influence the diets of patients.
- Recognize populations at increased risk for caries and describe caries prevention products and procedures for this population.
- Explain the use of personalized patient care and nutritional counseling to decrease incidence of caries.
Mark J. Szarejko, DDS, FAGD, received his dental degree from the State University of New York at Buffalo in 1985. He received fellowship from the Academy of General Dentistry in 1994.
Contributing faculty, Mark J. Szarejko, DDS, FAGD, has disclosed no relevant financial relationship with any product manufacturer or service provider mentioned.
Sarah Campbell
The Director of Development and Academic Affairs has disclosed no relevant financial relationship with any product manufacturer or service provider mentioned.
The purpose of NetCE is to provide challenging curricula to assist healthcare professionals to raise their levels of expertise while fulfilling their continuing education requirements, thereby improving the quality of healthcare.
Our contributing faculty members have taken care to ensure that the information and recommendations are accurate and compatible with the standards generally accepted at the time of publication. The publisher disclaims any liability, loss or damage incurred as a consequence, directly or indirectly, of the use and application of any of the contents. Participants are cautioned about the potential risk of using limited knowledge when integrating new techniques into practice.
It is the policy of NetCE not to accept commercial support. Furthermore, commercial interests are prohibited from distributing or providing access to this activity to learners.
Supported browsers for Windows include Microsoft Internet Explorer 9.0 and up, Mozilla Firefox 3.0 and up, Opera 9.0 and up, and Google Chrome. Supported browsers for Macintosh include Safari, Mozilla Firefox 3.0 and up, Opera 9.0 and up, and Google Chrome. Other operating systems and browsers that include complete implementations of ECMAScript edition 3 and CSS 2.0 may work, but are not supported. Supported browsers must utilize the TLS encryption protocol v1.1 or v1.2 in order to connect to pages that require a secured HTTPS connection. TLS v1.0 is not supported.
The role of implicit biases on healthcare outcomes has become a concern, as there is some evidence that implicit biases contribute to health disparities, professionals' attitudes toward and interactions with patients, quality of care, diagnoses, and treatment decisions. This may produce differences in help-seeking, diagnoses, and ultimately treatments and interventions. Implicit biases may also unwittingly produce professional behaviors, attitudes, and interactions that reduce patients' trust and comfort with their provider, leading to earlier termination of visits and/or reduced adherence and follow-up. Disadvantaged groups are marginalized in the healthcare system and vulnerable on multiple levels; health professionals' implicit biases can further exacerbate these existing disadvantages.
Interventions or strategies designed to reduce implicit bias may be categorized as change-based or control-based. Change-based interventions focus on reducing or changing cognitive associations underlying implicit biases. These interventions might include challenging stereotypes. Conversely, control-based interventions involve reducing the effects of the implicit bias on the individual's behaviors. These strategies include increasing awareness of biased thoughts and responses. The two types of interventions are not mutually exclusive and may be used synergistically.
#54680: Caries-Prone Patients: Prevention, Assessment, and Intervention
Dental caries is a preventable disease that affects a majority of the population. According to the 2011–2016 National Health and Nutritional Examination Survey, approximately 90% of adults 20 to 64 years of age had at least one decayed tooth [1]. Data collected between 2017 and 2020 indicate that among children and adolescents 2 to 19 years of age, 46.0% had one or more carious lesions in their primary or permanent teeth [2]. These statistics show the increase in caries incidence over time, making it important for dental professionals to develop strategies for determining caries risk and counseling patients to reduce risk and a future of dental caries.
The impact of nutrition on the caries process is known in the dental field, but dental professionals need to continue to convey the importance of this relationship to patients. Working as partners with patients, dental professionals can aid in the prevention of dental caries and help maintain patients' overall health by offering nutritional counseling and behavior modification techniques. The incidence of caries in the United States could decrease significantly as dental professionals implement the advances available for early caries detection, recommend anticaries treatments, and offer nutritional analysis and counseling. This basic-level course is intended to equip all members of the dental team with the skills needed to realize this over-riding goal.
Dental caries is a multifactorial disease. It is also preventable. In order for caries disease to occur, a number of factors must be present, including caries-causing microorganisms, a susceptible tooth surface, fermentable carbohydrates, and time. Dental professionals have the obligation to inform adult patients and parents of young patients that they possess the power to prevent and reverse this disease process. In this section, the factors that affect caries development will be addressed.
Untreated dental caries among deciduous ("baby/milk") teeth is the most prevalent childhood ailment, affecting 514 million children globally. Overall, dental caries affects 97% of the global population at some point in their lives [3,4]. The accepted theory of caries formation is related to the acids produced by oral bacteria removing tooth surface minerals, eventually causing a cavitation. Streptococcus mutans (S. mutans), S. sobrinus, Bifidobacterium species, and Lactobacillus micro-organisms have all been found to aid in caries progression [5,6]. These same bacteria are associated with root caries, as are the micro-organisms Actinomyces viscosus and A. naeslundii, which are notably present in active lesions [7].
Infants are not born with pathogenic oral bacteria but can acquire them from the skin or vaginal area during delivery or from family members with whom they are in close contact [8]. It has been determined that these bacteria can be transmitted between individuals through kissing, sharing eating utensils or cups, and other interactions. Studies have demonstrated that the mouth of the neonate is colonized by bacteria that resemble those from the oral cavity of the mother [9]. Women of childbearing age, parents, and caregivers of young children should be educated about the potential to transmit the bacteria contributing to dental caries.
All erupted teeth have the potential to develop caries lesions. However, teeth with optimal fluoride content are more resistant to caries lesion development than are teeth lacking in fluoride, as fluoride has an essential role in protecting enamel from demineralization [10]. Patients with recession (exposed root surfaces) are at increased risk for dental caries because roots do not have enamel, the extremely hard and most caries-resistant material surrounding the crown of the tooth.
A diet high in sugar, including fermentable carbohydrates, increases the likelihood of developing dental caries. Included are foods that are innately sugary (e.g., juices), those with sugar added (e.g., soda and candy), and starchy foods that break down into sugars in the mouth (e.g., breads and crackers).
When fermentable carbohydrates are introduced into the mouth, the sugars begin to be broken down to acid by oral bacteria. This acid lowers the pH of the saliva and oral plaque biofilm and may increase the rate of demineralization of tooth surfaces. Tooth enamel begins to demineralize at a pH of 5.5, and root surface demineralization occurs at an even milder pH of 6.2 [11]. Once the pH dips into these ranges, the outer layer of the tooth loses minerals. This causes a loss in surface hardness and increases the possibility of caries lesion progression.
Time is a contributing factor in the caries process because the probability of caries increases as the frequency of acid formation from fermentable carbohydrate–rich food sources increases [6]. Simply stated, the more often fermentable carbohydrates are ingested, the more often salivary pH will decrease, and the greater the likelihood that teeth will experience demineralization. The extent of demineralization depends on the length of time the acidic biofilm is in contact with the tooth surface and the frequency of this contact. Caries lesions are the result of repeated or extended periods of demineralization.
Caries lesions are detected a number of ways [3,12,13,14]:
Visual examination is employed for diagnosing large pit and fissure, root surface, and facial and lingual smooth surface caries lesions.
Inspection with a blunt explorer or probe over the surfaces of teeth is the tactile method of detecting caries lesions. This exploration is especially effective around margins of existing restorations.
Using the air/water syringe to visualize teeth wet and dry is helpful. Demineralized surfaces will look dull, chalky, and irregular when dry.
Radiographs can be used to identify interproximal caries before they can be detected visually or tactilely, allowing for diagnosis when they are small or incipient.
Transillumination is the technique of shining light through the teeth with a dental light and mirror or with fiber-optic equipment. Various lasers for caries detection are available from dental equipment manufacturers. These methods allow tooth examination without risking cavitation of decalcified tooth surfaces, as may occur with the use of dental instruments.
Employing a combination of these methods increases the probability of finding carious lesions in early stages when restorative treatment can be minimal or may even be avoided. A thorough dental examination helps the dental professional to determine a patient's caries risk level because any caries activity, including the presence of white spots or demineralization, automatically places a patient at high risk for caries development [15].
The role of plaque biofilm in the caries process necessitates the teaching and frequent reviewing of proper oral hygiene with patients. It is possible to distinguish patients who are at increased risk for dental caries by recognizing patients with poor oral care habits.
To prevent tooth decay, the American Dental Association recommends the following oral hygiene behaviors [16]:
Brush teeth twice a day.
Brush for two to three minutes.
Use a fluoride toothpaste that is ADA-accepted.
Replace the toothbrush every three to four months, or more frequently if bristles are fraying.
Floss or use an interdental cleaner daily to remove bacteria between teeth and under the gum line.
Limit snacking and eat a balanced diet.
Develop a customized at-home oral hygiene regimen that includes the use of prescription-strength fluoride gels or toothpastes.
Establish a dental recall schedule that reflects the patient's ability to maintain ideal oral hygiene.
Since the average patient brushes for less than one minute and few adults floss daily, it is important to review the ADA guidelines with patients at dental visits. To increase patient acceptance and understanding of oral hygiene instructions, it is advantageous for the dental professional to give patients the opportunity to demonstrate oral hygiene techniques. This allows the patient to receive feedback and gain confidence.
Power toothbrushes may be advisable for some patients because they are better than manual toothbrushes at reducing dental plaque levels and can be an exceptional oral hygiene tool for orthodontic patients and those with limited manual dexterity [16]. Timers may also be recommended to ensure that patients are brushing for a full two to three minutes.
In order to decrease caries through nutritional counseling, the dental professional must understand the most common caries-promoting behaviors and diet choices among the population. Poor nutrition can promote the development of carious lesions and can also have an adverse effect upon the structural integrity of the gingival tissues, the oral mucosa, and the periodontium [17].
Snacking is a common habit in the United States, with 90% of U.S. adults reporting one or more snacks per day—which accounts for approximately 22% of their daily energy intake [18]. Snacking promotes caries for a number of reasons. First, patients do not often brush or floss after eating snacks, leaving food debris and dental plaque biofilm in the mouth for extended periods. Second, most snack foods either have elevated sugar content or—like potato chips and crackers—are high in fermentable carbohydrates, allowing for acid formation from oral bacteria. Third, snacks are usually eaten throughout the day, permitting oral bacteria to produce acid and lower the salivary and plaque biofilm pH multiple times in a relatively short period.
Snacking habits have changed over the years, making it important for dental professionals to stay abreast of healthy options and nutritional evaluation techniques. Over a span of 35 years—between 1977 and 2012—there was a significant increase in per capita energy intake from snacking. The snack foods and beverages consumed were typically sugar-sweetened beverages, desserts, sweets, and salty snacks, the consistent consumption of which is not ideal for oral or systemic health [18]. The consumption of such snacks between meals or at a time that is typically not conducive to tooth brushing leads to a cumulative effect of an increased potential for the development of carious lesions. It is estimated that in the United States, approximately 22% of the daily caloric intake is from snacks that are sweet, salty, or desserts despite dietary guidelines that these items should comprise a limited portion of the daily caloric intake [18]. Even patients trying to eat healthfully may fall prey to ingesting excessive sugar because many snack foods marketed as "low-fat" have increased sugar per serving to improve taste once the fat is removed.
The average American consumes approximately 20 teaspoons of sugar every day via ingredients in foods and beverages such as fructose, dextrose, and high-fructose corn syrup [19]. The amount of sugar in the typical American diet not only promotes caries but also underlies the increase in obesity, heart disease, and diabetes in the general population. The American Heart Association recommends that men consume no more than 9 teaspoons (36 grams or 150 calories) of added sugar per day and that women consume no more than 6 teaspoons (25 grams or 100 calories per day) of added sugar per day [20].
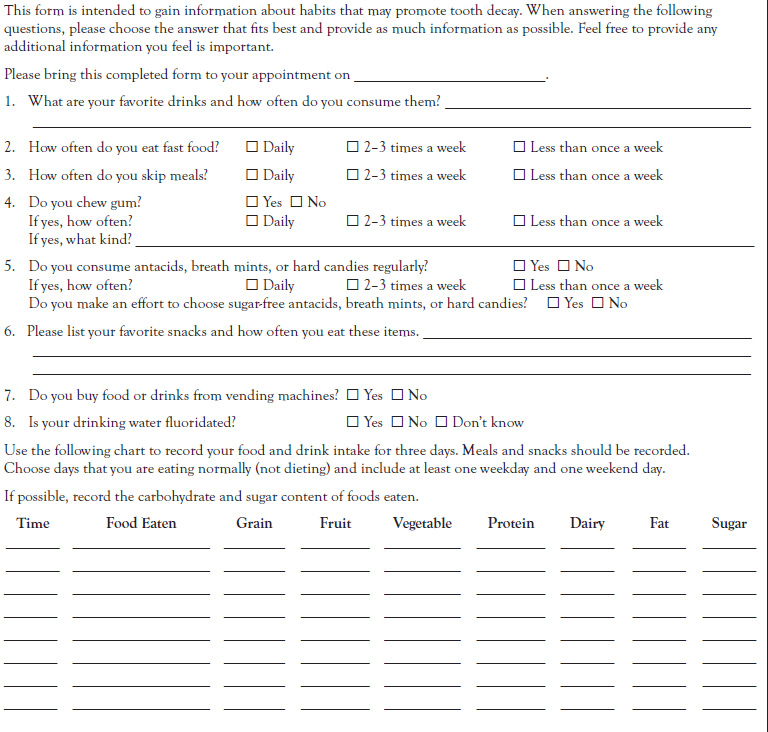
The Nutritional Questionnaire and Food Log shown in Table 1 is an example of a dietary questionnaire that clinicians can use to gather nutritional information that is pertinent to oral health. A food log can help the dental professional guide patients to modify snacking habits and include fewer fermentable carbohydrates and sugars. Some dental providers ask their patients each question, and the questions can be customized depending on previous knowledge. Other dental providers send questionnaires home with patients and assess them at a subsequent appointment.
The technique used would depend on the caries risk of the individual and the suspicion that diet plays a role. See the Resources section for websites that contain valuable information and interactive programs to help patients improve their diets.
To decrease caries risk, dental professionals should encourage patients to make changes in the composition and frequency of snacks—moving toward more healthy choices. Even minor changes, such as limiting snacks to a period of 10 to 15 minutes once a day and brushing teeth or chewing sugar-free gum after snacks, may decrease this common habit's negative effects on patients' teeth.
The American population's consumption of fast food has been growing steadily for many years. Data from the National Health and Nutrition Examination Survey of 2017–2018 indicated that on an average day, 36.5% of American adults consume fast food, which accounted for 13.8% of their daily calories [21]. Children and adolescents vary in their daily caloric intake from fast food consumption. Each day, approximately 36.3% of children and adolescents consume fast food, with 11.4% of children and adolescents obtaining more than 45% of their daily caloric intake from fast food; 13.8% obtaining 25% to 40% of their caloric intake from fast food; and 11.1% obtaining less than 25% of their caloric intake from fast food [22]. Clearly, millions of Americans consume fast food on a regular basis, and this is associated with a high caloric intake and poor diet quality. Patients who eat fast food meals or snacks laden with carbohydrates are at increased risk for caries due to the high amounts of sugar and fermentable carbohydrates present in fast food items [23]. Being armed with knowledge of the statistical relationships between fast food and caries may help the dental professional counsel patients on making healthier fast food choices.
In addition, there is a correlation between eating fast food on a regular basis and developing insulin resistance, which is a risk factor for type 2 diabetes [24]. To guide patients with diabetes and the general public toward healthier fast food options, the practitioner can refer patients to the American Diabetes Association website (http://www.diabetes.org), their physician, or a nutritionist for guidance specific to the patient's health condition, keeping in mind that as a dental professional, oral health should remain a focus.
Within the United States, the median annual per capita consumption of sugar-sweetened beverages (SSB) in 2021 was 37.1 gallons, with the annual per capita consumption of SSB the lowest in Hawaii (23.5 gallons) and the highest in Missouri (51.8 gallons) [25]. Most people are unaware of the sugar content of their favorite sugar-sweetened beverage or soda, and they are not aware of the daily recommended maximum amount of sugar. The World Health Organization has recommended that for children the maximum daily consumption of sugar is 3 teaspoons. A 20-ounce bottle of soda contains about 16 teaspoons of sugar, while a 12-ounce can contains about 10 teaspoons of sugar [26]. Many nutritional experts and health organizations believe that soda and SSB in general are a major contributing factor to the escalation of childhood and adult obesity [27]. The consumption of soda doubles the risk of the development of carious lesions in children and increases the potential for the development of carious lesions in adults [26].
The patient education pamphlet "Sip All Day, Get Decay!" produced by the Minnesota Dental Association (available at http://www.sipallday.org) states that the average 12-ounce can of soda has 10 teaspoons of sugar and a pH just over 3. The low pH of soft drinks results from the ingredient phosphoric acid. Sodas also contain carbonic acid, and many contain citric acid. Therefore, even diet sodas are detrimental to oral health due to their acidic pH levels.
Patients who sip soda throughout the day cause their oral pH to plunge due to the acidity of the soda and the acid formed from oral bacteria metabolizing the sugars with this extended exposure a source of an increased risk for the development of dental caries [28].
Sports drinks and fruit juices also tend to be acidic and contain high amounts of sugar [29,30]. The use of these products should be limited. Milk and water remain the best drink options for healthy teeth. The development of flavored, unsweetened water gives patients another drink option that is not detrimental to their teeth.
It is important for dental professionals to study the factors influencing patients' diet choices to understand the motivations behind them and to offer healthy alternatives. Factors influencing diet include food availability, family structure, convenience, parental influence, habit, cost, and media [31,32].
As the number of Americans who are eating meals prepared outside of the home continues to increase, food availability and convenience have become factors that greatly influence food choices. The majority of foods that are considered "convenient" are high in sugar, refined or fermentable carbohydrates, and fat [17,18]. These foods are therefore unhealthy choices for oral and systemic health. Examples of convenience foods include hamburgers, chips, vending machine snacks, and candy bars.
The prevalence of vending machines gives people access to many low-nutrient, energy-dense snacks on a daily basis [33,34]. The Smart Snacks school nutrition standards became effective at the beginning of the 2014–2015 school year and established limits on the amount of fat, sugar, sodium, and calories in foods that are sold in vending machines within school settings [35]. The Smart Snacks school nutrition standards have specific nutritional requirements for food items sold in vending machines, student stores, and snack bars [36]. However, simply not having these options available is not the complete answer. Hungry teens need to understand the benefits of high-nutrient snack options and learn to seek them out.
Within the United States, vending machines are present in 43% of elementary schools, 74% of middle schools, and 98% of high schools [37]. Though Congress has mandated a reduction of foods and snacks in schools that are correlated with obesity and dental caries, schools continue to struggle with replacing these items with more nutritional, low-fat options as do hospitals and workplaces [38]. Many schools gain some revenue from vending machine sales, which adds to the complexity of changing food items. Schools, food vendors, and families continue to struggle with balancing nutrition, funding, and adolescents' food preferences. Vending machines are found in many places besides schools, and the low nutritional quality of vending machine foods is generally consistent throughout the different locations [38]. Increasing the nutritional value of foods available through vending machines would have a positive impact on various groups. Dental professionals should educate patients about the healthiest and least caries-promoting vended items, such as sunflower seeds, nuts, crackers with cheese, and sugar-free gum.
Many fast food chains have added more nutritious options to their menus in an effort to appeal to health-conscious consumers. Dental professionals can promote patients' oral health by educating them about the impact of common convenience foods on the caries process and guiding them toward more healthful choices.
Parental influence also plays a role in diet choices, especially those of children and adolescents [39]. Because parents generally purchase the foods available for snacking and family meals, they have a high level of control over what foods are eaten by their children.
Children tend to emulate their parents' food choices [39,40]. Parents' food choices and nutritional guidance can be driven by habits, myths, misinformation, weight control efforts or problems, availability, and their own nutritional knowledge [17,41]. Other factors that influence dietary choices include cultural preferences, parenting styles, and family dynamics [17]. Dental professionals should guide parents to not buy sodas and low-nutrient foods in an effort to discourage the formation of habits such as snacking and soda consumption that can contribute to caries. Parents may need to be guided to make healthy, affordable choices for themselves and their families. Also, parents can limit snacking by not allowing children to eat while watching television or playing video games. Educating parents about their influence and guiding them toward healthy food choices can benefit the entire family.
Eating habits start early and may be difficult to change, especially as time solidifies these behaviors [39,42]. Habits such as eating at the table, having a healthy breakfast, and eating fruits and vegetables can and should start in childhood; however, it is never too late to start these beneficial habits [40,43]. Through discussing habits with patients, dental professionals can encourage behaviors that will promote oral health and identify caries-promoting practices that need to be altered.
The cost of food is a factor that influences dietary choices for many people. Foods with low nutritional value are often more affordable and more easily accessible than foods with high nutritional value. Fresh fruits, vegetables, and lean proteins are more costly per serving than alternatives that are higher in sugar and fermentable carbohydrates [44]. In addition, there is an inverse relationship between calories and cost per serving: Nutritionally deficient foods such as those with high sugar, fermentable carbohydrate, and fat content are among the most affordable dietary choices [45].
When recommending diet modifications to patients, dental professionals need to consider food costs for many reasons. Studies show that persons of low socioeconomic status tend to live in neighborhoods known as food deserts, where good quality, nutritional foods are scarce and transportation and the time needed to get to nutritional food sources factor into the cost of food [46]. Due to the higher costs associated with healthier foods, people with low incomes incur the highest risks of diet-related conditions [47].
Media have an impact on diet in two ways. Children ages 8 to 18 spend approximately 7.5 hours every day with media, including television, the Internet, music, magazines, cell phones, and tablets. Marketing of foods and snacks to children tends to be geared toward low-nutrition foods and beverages [48]. Media influence diet choices, especially those of children, by the sheer number of food-related advertisements found on television, in print, and on cell phones and tablets—which can evade parental monitoring [48].
By realizing the factors that affect patients' diets, dental professionals are more likely to recommend diet changes to which patients will be willing to adhere. Also, dental professionals can educate patients about these factors to facilitate self-assessment of dietary influences.
Certain populations are at increased risk for caries formation due to diet, habits, lack of adequate oral hygiene, and other factors. These populations can especially benefit from nutritional counseling and caries prevention applications and procedures.
Because all teeth, once erupted, are susceptible to dental caries, even very young children are vulnerable. Early childhood caries (ECC) is defined as the presence of one or more decayed, missing (due to caries), or filled tooth surfaces in the primary dentition of a preschool-age child [49]. This condition is seen throughout the general population but is more common in the poor and near-poor preschool children. In the United States, it is estimated that between 3% and 6% of children have early childhood caries [50]. The National Institute of Dental and Craniofacial Research (NIDCR) has indicated that between the years of 2011–2016 that 23% of children between the ages of 2 and 5 years had carious lesions in their primary teeth and that children from lower-income families were twice as likely to have decay in their primary teeth compared to children from higher-income families [51]. Among children ages 6 to 11 years, 17% had decay in their permanent teeth [51].
To prevent ECC development, the American Academy of Pediatric Dentistry (AAPD) recommends that children have their first dental appointment soon after their first tooth erupts and no later than their first birthday [49]. Educating the child's primary caregiver about oral hygiene care for the child and proper use of bottles is one of the main objectives of this appointment. Sodas, juices, and other sugared drinks should not be given to children, or they should be given very sparingly, and they should never be dispensed through a bottle. Children using bottles should not be allowed to go to sleep with them unless the bottle contains water. The AAPD also advises eliminating the use of a baby bottle by age 12 months and avoiding foods and drinks that contain sugar for children under 2 years of age [49].
Parents and primary caregivers need to be reminded about the eruption pattern of teeth and the fact that children have new teeth exposed to the oral environment from age 6 months to approximately age 12 years. The enamel of primary teeth is thinner and less organized compared to the enamel of permanent teeth, so the former is more susceptible to demineralization and the formation of carious lesions compared to the latter [50]. Therefore, soda, sugar, and fermentable carbohydrate exposure is more detrimental in youth than in adults.
The incidence of caries continues to rise as children grow into teenagers. According to the NIDCR, approximately 57% of adolescents between ages 12 and 19 have had carious lesions in their permanent teeth [52]. Adolescence is a time of increased caries risk because teenagers consume diets that are higher in fermentable carbohydrates and sugars, and they often practice poor oral hygiene.
Research shows that this age group responds to health behavior change requests through motivational interviewing (MI) techniques, rather than the traditional dissemination of information and dispensing of advice [53]. Motivational interviewing, a collaborative, goal-oriented form of communicating behavior change, has been shown to positively affect adolescents' change in diet, exercise, and compliance with medications. MI techniques that will help professionals better communicate oral healthcare principles with this age group and the mechanisms by which MI works to instill behavioral changes in adolescents is an area of continued research [54]. Among high school students between 2019–2021, approximately 16.5% of boys and 12.7% of girls had consumed one or more sugar-sweetened soda beverages each day [55,88]. Soda is included with other sugary products and those made with solid fats in the category of empty calories. Empty calories account for 30.2% to 34.4% of 9- to 13-year-olds' daily caloric intake and 30.5% to 35.5% of that of 14- to 18-year-olds [56]. Utilizing the principles of MI, the dental professional can work with each teenager to find easily accessible and tasty alternatives to sugar-laden foods. The Resources section contains links to websites that can be shared with young patients and their parents.
Many adolescents have braces or other orthodontic appliances that complicate oral hygiene. The combination of susceptible tooth surfaces, a high-sugar diet, and poor oral hygiene is the perfect recipe for caries formation.
To decrease caries risk in the adolescent population, medical and dental professionals should inform teenagers about the impact of diet choices on teeth and educate them about healthy eating. Minor changes such as limiting soda consumption to mealtimes and brushing after meals can have a large impact on caries development. In addition, the use of fluoride and sealants is extremely beneficial in preventing caries in the adolescent population.
Adolescents are forming habits that will be a foundation for their adult life. Healthy eating, limiting snacks and sugars, and good oral hygiene will be invaluable practices that will help protect their teeth from caries.
Older adults are at increased risk for caries as a result of gingival recession, reduced saliva flow, inadequate oral hygiene, physical and sensory limitations, and cognitive limitations [57]. In the United States alone, the elderly population (i.e., those age 65 and older) will grow to 20% (72 million) by 2030 [57,58]. Aging baby boomers who have retained more of their teeth and have undergone more complex dental procedures will have a greater exposure to dental caries and periodontal concerns, as well as greater expectations of their dental care providers [57,59]. Many studies have found root surface caries to be most prevalent in the elderly population [60].
Ideal oral hygiene may be difficult to achieve, as manual dexterity often becomes limited in elderly patients. The presence of partial dentures also complicates oral hygiene, as food and plaque frequently accumulate where the dentures rest against the natural tooth structure. Educating elderly patients who wear partial dentures, and their caregivers when applicable, concerning proper oral hygiene is essential to protect the teeth adjacent to partials from caries. Practices such as cleaning the mouth after meals with fluoridated toothpastes and rinses, removing partials when performing oral hygiene, removing partial dentures before going to bed, paying attention to dietary intake, and using prescription-strength fluoride gels or toothpastes should be encouraged in these patients [59,61].
Elderly patients also consume an elevated amount of fermentable carbohydrates and sugars, further increasing their caries risk. Missing teeth, poorly fitting prosthetics, and tooth mobility due to periodontal disease may make eating fresh fruits, vegetables, and high-fiber foods difficult. To replace these items in their diet, elderly patients are more likely to consume breads, cakes, pies, and food replacement drinks, as these substances are easy to prepare and eat [59]. In addition, elderly patients may suck on hard candies and eat sugary snacks throughout the day to combat the symptoms of xerostomia.
Special considerations need to be taken into account when recommending dietary changes to elderly patients. Food cost, level of difficulty of preparation, and ease of mastication are factors that must be taken into account when advising dietary changes. Replacing candies with a sugar-free variety, limiting snacks, and adding calcium-rich foods such as cheese to their diet are a few of the measures that older adults can take to reduce caries risk. The use of power toothbrushes and fluoride may also be helpful in reducing caries incidence in this population.
Xerostomia is the subjective description of dry mouth, which can be caused by any number of events [62]. Dry mouth can be a transient reduction or loss of saliva as a result of salivary gland dysfunction. It places patients at a higher risk for caries because saliva contains buffers to neutralize acids in the mouth. Adequate saliva is important for several reasons. The presence of calcium and phosphate in the saliva aids in the remineralization of tooth surfaces [63]. Saliva also helps to naturally cleanse teeth, protects the oral mucosa from mechanical injury, facilitates chewing and swallowing, and inhibits bacterial growth [64,65].
Saliva production can decrease with age [59,66]. Moreover, some medications are commonly associated with xerostomia. More than 500 medications have reduced saliva as a side effect [62,67]. The main medication classes associated with xerostomia include antidepressants, antihypertensives, antihistamines, antipsychotics, sedatives, anorexiants, antiparkinsonism agents, opioids, muscle relaxants, and diuretics [65]. Head and neck radiation therapy and the autoimmune disease Sjögren syndrome are other common causes of salivary gland dysfunction that results in dry mouth [62,68].
Remedies for reducing the effects of xerostomia vary, and recommendations should be patient specific. Depending on a patient's age and cognitive ability, dental professionals should encourage them to chew sugar-free gum, use sugar-free candies, or sip water to reduce the exposure to sugars. The use of over-the-counter saliva substitutes for oral lubrication also helps to increase patients' comfort. Prescription medications designed to stimulate saliva flow may also be recommended for patients who have undergone radiation treatment and for those with Sjögren syndrome. However, efficacy, side effects, and compliance must be weighed against the benefits of using these medications [67,69]. Patients experiencing xerostomia need to demonstrate excellent oral hygiene and may benefit from fluoride and other caries prevention treatments such as the application of in-office fluoride varnish or in-office fluoride treatments [70].
Fluoride has been used for more than 80 years to prevent dental caries [70]. Demineralization and remineralization are natural processes, as minerals are lost and returned to the tooth surface during the day [71]. Fluoride strengthens enamel, making it more resistant to the acids that promote demineralization and facilitate the development of carious lesions. It also enhances the remineralization of impaired tooth surfaces [72]. Erupted teeth accrue the most benefit from fluoride when its salivary concentration is incorporated into the biofilm that adheres to the teeth [72]. Although it is a bit controversial, water fluoridation is one method of achieving these conditions [70,72]. Approximately 72.7 of U.S. communities have fluoridated water as of 2020 [55]. Bottled water does not contain enough fluoride to prevent dental caries, so patients who drink only bottled water must be educated about the benefits of the topical fluoride found in toothpaste, oral rinses, and prescription-strength fluoride supplements [70,73]. Parents of young children should be aware that multiple forms of fluoride ingestion can lead to fluorosis, that is, detectable changes in the tooth surface that can discolor the tooth but that do not adversely affect tooth strength [72].
Fluoridated water, toothpastes, and mouth rinses are advisable for the general population and especially for caries-prone patients because the use of a fluoride mouth rinse in conjunction with the use of a fluoridated toothpaste enhances enamel fluoridation and remineralization [72]. The use of prescription-strength fluoride toothpaste (1.1% neutral sodium fluoride) may be advantageous to and is usually well tolerated by patients consuming caries-promoting foods, orthodontic patients, patients with xerostomia, and those demonstrating substandard oral hygiene [72].
In-office fluoride treatments may help patients reduce dental caries. Treatments come in a variety of forms, including foams, gels, rinses, and varnishes. The application of 5% sodium fluoride varnish twice a year on the primary and permanent teeth of children ages 6 months through 15 years is beneficial in preventing caries in this age group as well as for the permanent teeth of adult patients [10,70]. The use of in-office professionally applied fluoride gel or foam at 3- to 12-month intervals provides the most preventive benefit for those do not consume fluoridated water and/or whose at-home oral hygiene is substandard [74].
Xylitol, a sugar alcohol (polyol), is a sugar substitute that helps to prevent dental caries because oral bacteria are unable to break it down to an acid [49,75]. Xylitol also inhibits plaque formation, especially that of mutans streptococci, and has been shown to contribute to remineralization [76,77].
Nutritionally, xylitol has fewer calories than sugar—2.4 calories per gram versus approximately 4.0 calories per gram of sugar [76]. It is also safe for diabetic patients to consume, making it a wise choice for replacing sugar in patients' diets for reasons beyond caries control because xylitol lowers the insulin response compared to foods sweetened with sorbitol or ordinary sugar [78]. Replacing sugar with xylitol has been shown to cause a statistically significant reduction in S. mutans, which is the primary cariogenic bacterial species [79].
New studies are seeking to determine the efficacy and optimal dosage of erythritol, another polyol, for caries prevention. The efficacy of polyols to prevent caries when used to sweeten gum, candy, and food may be confounded by the presence of natural and added fluoride in the diets of the study participants. Some studies have revealed that the combination of xylitol and fluoride can reduce the biofilm in which the cariogenic bacteria reside [80].
Dosage recommendations for xylitol as an anticaries agent include several small exposures during the day, with a plateau effect for the reduction of the cariogenic bacterium S. mutans noted between 6.88 grams per day and 10.32 grams per day [76]. This can be accomplished by using toothpastes, gums, and mints that contain xylitol and using xylitol as a sugar replacement to sweeten foods and drinks. Xylitol can also be used in place of sugar in baking, but patients should be cautioned that consuming large quantities of xylitol may cause gastrointestinal upset.
The pits and fissures of teeth can be especially caries prone, and applying sealants here is a component of a comprehensive approach to caries management [4]. Pits and fissures in the occlusal, buccal, and lingual surfaces retain food particles and plaque, thus complicating oral hygiene efforts. Consequently, these surfaces are the predominant areas of dental caries. Pit and fissure sealants have been employed to prevent pit and fissure dental caries since the 1960s and remain an excellent method of reducing risk for dental caries. A 2016 systematic review suggests that well-placed occlusal sealants protect the pits and fissures from caries development better than fluoride varnish application does [4]. The review in no way recommends forgoing fluoride application to protect occlusal surfaces from caries. Rather, it states that the available evidence supports the use of both preventive measures where appropriate. Clinicians need to use a combination of assessment and diagnostic tools to determine the best treatment plan for preventing decay and preserving tooth structure in individual patients.
In order to identify pits and fissures that are suitable for the application of preventive sealants or other minimally invasive procedures, dental examinations should include the clinical evaluation of tooth surfaces visually and with the use of a blunt explorer; laser detecting device; compressed air; and the newest addition to caries classification, the International Caries Detection and Assessment System [81]. The ICDAS system is an evidence-based process for identifying and classifying dental caries lesions using visual cues [82]. This method of classifying carious lesions allows clinicians to apply appropriate evidence-based preventive and minimally invasive treatment methods to affected tooth surfaces. Using a scale of 0 (sound) to 6 (extremely decayed) to classify each pit and fissure, clinicians can safely determine the best practice for treating the surface, which can include no treatment, fluoride application, sealants, or restorative procedures [82].
Dental caries is a multifactorial disease. Counseling a patient who is at risk for caries requires the clinician to consider the various factors that can put patients at risk for, or protect them from, dental caries. In addition to caries-promoting diets and belonging to one or more of the high-risk populations discussed previously, the following are factors that can increase an individual's caries risk [15,28,83]:
Poor oral hygiene
Family history of poor dental health
Prolonged bottle- or breastfeeding
High bacterial titers of S. mutans
Intermittent dental care
Mental or physical disabilities that limit oral hygiene ability
Numerous multisurface restorations
Restorations with open or overhanging margins
Orthodontic appliances
Enamel defects and genetic tooth abnormalities
Radiation or chemotherapy treatments
Eating disorders
Alcohol and drug abuse
Smoking and vaping
Determining a patient's caries risk level, and therefore the relative importance of nutritional counseling and other interventions, requires consideration of these factors and communication with the patient and/or patient's parent. Some of these factors can be identified during the dental examination, such as recession, multisurface restorations, and enamel defects. Other factors, such as personal and family dental history, are elusive and require an open dialogue with the patient and/or patient's parent [84].
There are several caries risk assessment tools available [4,84]. Practitioners need to find a tool that allows them to evaluate the variety of factors associated with caries risk as they begin to discuss how diet and nutrition affect the patient's risk for caries. Caries risk assessments categorize patients into one of three categories. A patient at low caries risk exhibits no caries risk factors and a dental history of no incipient or active caries lesions in the past three years. Patients at moderate risk for caries include those that had either one or two incipient or active caries lesions in the past three years or no caries history in the past three years but at least one caries risk factor. High caries risk is the determination given to patients who have developed three or more caries lesions (incipient or active) in the past three years, have low fluoride contact, present with multiple caries risk factors, or have severe xerostomia [85].
Separate caries risk assessment forms for patients ages 0 to 6 years and for patients older than 6 years can be found on the ADA website at http://www.ada.org/en/member-center/oral-health-topics/caries. Use of these forms will facilitate and standardize the dental team's caries risk assessment. In addition, the use of risk assessment forms can help uncover the role of poor nutrition as a risk factor and allow the topic of nutrition to be more effectively woven into the risk reduction discussion.
All patients stand to benefit from nutritional counseling. Once a caries risk level has been established, all patients should be counseled on how their diet affects their teeth, their caries risk, and their general oral health. Personalized oral hygiene instructions should be established for each patient. Those patients identified as being at moderate to high risk for caries may need to have nutritional counseling and preventive measures not just discussed but also incorporated into their treatment plans.
Dental caries is a preventable disease. However, a high incidence of caries in early childhood is the single strongest predictor of the development of carious lesions into adolescence and adulthood [86]. For patients at low to low-moderate risk for dental caries, nutritional counseling may be performed at the dental cleaning, or recare, appointment. Questions regarding diet, such as those listed later in this section, may be asked on the medical history form or directly of the patient by the dental professional. For these patients, the goal of nutritional counseling is education designed to maintain their low caries risk level.
Patients with a moderate- to high-risk level of caries may benefit from a separate nutritional counseling appointment. The appointment length is individualized based on the patient's dental knowledge, dietary habits, and motivation level. During this appointment, the dental professional and patient have an opportunity to evaluate the patient's current diet, discuss preventive treatments, and set goals to improve the diet and reduce caries incidence.
To gain information concerning dietary habits, the dental professional may have patients complete a diet questionnaire and food log [87]. An example of a dietary questionnaire and food log was previously shown in Table 1. Alternatively, the dental professional may choose to interview patients concerning dietary habits, using questions such as:
What are your favorite snacks?
On a typical school or workday, what do you eat for lunch?
What is your favorite soft drink or fruit juice, and how often do you drink it?
How long does it take you to finish a can of soda or a glass of juice?
How often do you brush your teeth? How often do you floss?
Follow-up to the nutritional counseling appointment should take place in order to encourage the patient's goals and reinforce habit changes. This follow-up may consist of a phone call to check in with the patient, or it may be a short appointment a few weeks after the counseling appointment. The patient's progress can be reevaluated at subsequent dental appointments.
Establishing and routinely reassessing a patient's caries risk level allows the dental professional to provide proactive care and recommend preventive measures to minimize the patient's risk of dental decay.
Occasionally, a patient may benefit from a referral to a dietician, nutritionist, or primary care physician. This is especially true if a condition such as acid reflux, an eating disorder, or chemical dependency is suspected or confirmed.
The dental professional should be practical when recommending changes to a patient's diet. Asking patients to forfeit their favorite foods in exchange for increased brushing and flossing will rarely improve patient compliance. It is important to note, however, that relatively minor changes in nutrition and habits can lower a patient's caries risk. By evaluating each patient's individual incentives and motivation level, dental professionals can help patients set goals that are realistic and achievable.
Some examples of these goals are:
Limiting soda drinks to mealtimes
Exchanging sugared gum or candies for sugar-free or xylitol-sweetened varieties
Replacing soda with flavored water
Including sweet foods with meals, when the sugar content will be diluted
Making a conscious effort to eat a fruit or vegetable with every meal, as fruits and vegetables act as natural oral cleansers
Brushing with a xylitol-containing toothpaste and chewing xylitol gum twice a day
As patients set and achieve goals, additional changes can be recommended to further decrease caries risk. Nutritional counseling, like other behavioral modification interventions, is a dynamic process that is emphasized depending on need.
Savannah is a 4-year-old girl coming to your office for the first time. She is wearing a pretty dress and sparkly shoes, and she has a pink bow tying her long black hair up in a ponytail. She is obviously frightened. As you escort Savannah and her mother to the treatment room, the only thing Savannah says is that she does not want silver teeth. Savannah has an unremarkable medical history, takes no medications, is current with her vaccinations, and has no allergies. When you ask Savannah if any of her teeth hurt, she quietly nods. Upon being asked whether Savannah has been to the dentist, her mother explains that Savannah lived with her aunt for several months and during that time had been taken to her aunt's dentist. Her aunt's dentist had recommended stainless-steel crowns for Savannah's carious teeth #E and #F, but the aunt did not want to have the crowns placed without Savannah's mother's permission. Savannah is covered by insurance, but the insurance pays only for stainless-steel crowns, and Savannah's mother admits to having been unable to afford the tooth-colored crowns until now.
Establishing a caries risk level for this child should be easy, as her mother admits that she has active carious lesions. What is her caries risk level? One look at Savannah's cute smile reveals severe caries on teeth #E and #F. At this point, you complete the caries risk assessment form, determining the child's fluoride exposure level, oral hygiene routine, and snacking habits. Savannah's mother works full time and has two children, Savannah and her 3-year-old sister, Lillian. Savannah's mother admits that the girls don't brush their teeth regularly, as they commonly fall asleep in front of the television and are carried to bed. A typical breakfast consists of sweetened cereal, milk, and a juice box. They eat lunch at the babysitter's, and their mother tries to make them sit down to have dinner each night. The girls like to eat candy after dinner, frequently not eating all their dinner in order to save room for the candy.
Treating Savannah's oral conditions will be a long process. Because her caries risk is high, each appointment should include a short nutritional counseling session, which can be added to the treatment plan. If Savannah were your patient, what would be your plan for preventing new carious lesions? What would you consider to be a manageable step 1 for this child?
Treatment Plan
Savannah has ECC, with several carious lesions in each quadrant needing extensive restorative intervention. Her mother does not want her sedated, so the restorations will require no fewer than five appointments.
Vision for Preventing New Carious Lesions
Restore all existing cavitated lesions, promote remineralization of the noncavitated lesions, develop excellent oral self-care habits, and perform preventive dental hygiene care every four to six months until no new caries activity has been observed for a period of three years. In other words, the goal is to reduce Savannah's caries risk to low. It is imperative to break the chain of the four elements required for caries activity: Caries-causing micro-organisms, a susceptible tooth surface, fermentable carbohydrates, and time.
What Would You Consider to be a Manageable Step 1?
Initial examination should include simple nutritional counseling and thorough oral hygiene instruction that includes both the mother and child. Poor oral hygiene and eating habits are difficult to change. A good first step may be to give the family the goal of brushing their teeth after each meal. Discuss the bacteria and food that remain on teeth after eating and how they need to be removed after each meal. Comparing this process to the habit of washing hands before each meal to remove bacteria and dirt may help the child make the connection. Have Savannah's mother complete the Nutritional Questionnaire and Food Log and bring it to the next nutritional counseling session.
Mr. Ribeiro, a 68-year-old male, arrives for his dental hygiene recare appointment. He is a pleasant, retired gentleman. He appears happy, healthy, and quiet, as usual. His medical history is unchanged from his last visit six months ago. He has high blood pressure and prostate malfunction. He takes losartan, finasteride, and terazosin. He has no dental complaints. During your oral health and caries risk assessment, you detect very little plaque biofilm, no bleeding on probing, stable periodontal health, adequate saliva flow, a broken cusp on tooth #31, and what appears to be a recurrent carious lesion under the crown on tooth #8. As you complete your caries risk assessment, your first inquiry goes as follows:
Q: How often do you brush?
A: Three times a day.
Q: How do you clean in between your teeth?
A: I use that flosser thing three times a day.
Q: Do you snack?
A: Not very often.
Q: What do you drink when you're thirsty?
A: Water.
Dental professionals commonly see this scenario. The patient knows all the right answers, and you can't dispute his oral health routine, as his periodontal condition is excellent. However, he does have recurrent decay on tooth #8.
What follow-up questions might you choose to ask to fill in the blanks about the role his nutritional intake may play in this case?
Recalling the four factors necessary for the caries disease progression—susceptible tooth, diet, time, and bacteria—you need to be a bit of a detective. Mr. Ribeiro's history of dental care also includes several crowns and a recent restoration. This tells you that his teeth are susceptible. He maintains a clean mouth, or so he says, so you must consider that he removes the oral bacteria from his teeth regularly. Diet may be the culprit.
A good way to begin with a patient who knows all the right answers and does not want to be lectured might be to go through your caries risk assessment out loud. Begin by telling him why you are asking these questions. Tooth decay is preventable, and you want to help him prevent the need for more costly crowns and fillings in the future. Ask him to tell you what he has eaten in the past 24 hours. Share with him that even though he brushes three times a day, the bacteria and acids on his teeth will eventually begin to demineralize his teeth. Often, letting that fact form a picture in a patient's head can spur questions or even solutions for reducing the risk. Change is most likely to happen when the patient is a partner in the change.
Many patients take oral health for granted and will benefit from learning that caries is a preventable disease, and their dietary choices can either promote the progression of disease or aid in preventing caries development. Addressing nutritional choices during dental visits can positively affect patients and can help them make healthier choices for their entire family. Dental professionals as a community have the ability to educate hundreds of thousands of people. Taking the time to discuss nutrition with patients will pay the dividend of having healthier patients who truly value their teeth and overall health. As patients come to understand the relationship between oral health and systemic health, the impact of their dietary choices on both will become evident.
| Academy of Nutrition and Dietetics |
| 1-800-877-1600 |
| http://www.eatright.org |
| American Dental Association: Diet and Dental Health |
| http://www.mouthhealthy.org/en/az-topics/d/diet-and-dental-health |
| American Dental Association: Diet and Nutrition |
| http://www.ada.org/en/advocacy/advocacy-issues/diet-and-nutrition |
| Centers for Disease Control and Prevention |
| CDC Healthy Schools: School Nutrition |
| https://www.cdc.gov/healthyschools/nutrition/schoolnutrition.htm |
| Minnesota Dental Association: Sip All Day, Get Decay! |
| http://www.sipallday.org |
| National Association of Nutrition Professionals |
| 1-800-342-8037 |
| http://www.nanp.org |
| National Heart, Lung, and Blood Institute |
| We Can! Parent Tips: Making Healthier Food Choices |
| http://www.nhlbi.nih.gov/health/public/heart/obesity/wecan/downloads/tip_choices.pdf |
| U.S. Department of Health and Human Services |
| Dietary Guidelines Advisory Report |
| http://health.gov/dietaryguidelines/2015 |
| U.S. Department of Agriculture |
| ChooseMyPlate |
| http://www.choosemyplate.gov |
1. National Institute of Dental and Craniofacial Research. Dental Caries (Tooth Decay) in Adults (Ages 20 to 64 Years). Available at https://www.nidcr.nih.gov/research/data-statistics/dental-caries/adults. Last accessed October 15, 2024.
2. National Center for Health Statistics. Oral and Dental Health. Available at https://www.cdc.gov/nchs/fastats/dental.htm. Last accessed October 15, 2024.
3. Abdelaziz M. Detection, diagnosis, and monitoring of early caries: the future of individualized dental care. Diagnostics. 2023;13:3649.
4. American Dental Association. Caries Risk Assessment and Management. Available at https://www.ada.org/resources/ada-library/oral-health-topics/caries-risk-assessment-and-management. Last accessed October 15, 2024.
5. Zhang JS, Chue C-H, Yu OY. Oral microbiome and dental caries development. Dentistry Journal. 2022;10:184.
6. Zhu Y, Wang Y, Zhang S, et al. Association of polymicrobial interventions with dental caries development and prevention. Frontiers in Microbiology. 2023;14:1162380.
7. Takenaka S, Edanami N, Komatsu Y, et al. Periodontal pathogens inhabit root caries lesions extending beyond the gingival margin: a next-generation sequencing analysis. Microorganisms. 2021;9:2349.
8. Guo H, Li J, Yao H, et al. The dynamic communities or oral microbiome in neonates. Frontiers in Microbiology. 2022;13:1052525.
9. Nardi GM, Grassi R, Ndokaj A, et al. Maternal and neonatal oral microbiome developmental patterns and correlated factors: a systematic review. Does the apple fall close to the tree? International Journal of Environmental Research and Public Health. 2021;18:5569.
10. Veiga N, Figueiredo R, Correia P, et al. Methods of primary clinical prevention of dental caries in the adult patient: an integrative review. Healthcare. 2023;11:1635.
11. Amaechi BT, Phillips TS, Evans V, et al. The potential of hydroxyapatite toothpaste to prevent root caries: a pH-cycling study. Clinical, Cosmetic and Investigational Dentistry. 2021;2021(13):315-324.
12. Foros P, Oikonnomou E, Kolesti D, Rahiotis C. Detection methods for early caries diagnosis: a systematic review and meta-analysis. Caries Research. 2021;55(4):247-259.
13. Saffan ADA. Current approaches to diagnosis of early proximal carious lesion: a literature review. Cureus. 2023;15(8):e43489.
14. Ghodasra R, Brizuela M. Dental caries diagnostic testing. StatPearls. Treasure Island, FL: StatPearls; 2023.
15. Caries Care International. 1st D: Determine Caries Risk. Available at https://cariescareinternational.com/1st-d-determine-caries-risk. Last accessed October 15, 2024.
16. American Dental Association. Home Oral Care. Available at https://www.ada.org/resources/ada-library/oral-health-topics/home-care. Last accessed October 15, 2024.
17. Dimopoulou M, Antoniadou M, Amargianitakis M, et al. Nutritional factors associated with dental caries across the lifespan: a review. Applied Sciences. 2023;13:13254.
18. Enriquez JP, Gollub E. Snacking consumption among adults in the United States: a scoping review. Nutrients. 2023;15:1596.
19. John Hopkins Medicine. Obesity, Sugar and Heart Health. Available at https://www.hopkinsmedicine.org/healt/wellness-and-prevention/obesity-sugar-and-heart-health. Last accessed October 15, 2024.
20. American Heart Association. How Much Sugar is Too Much? Available at https://www.heart.org/en/healthy-living/healthy-eating/eat-smart/sugar/how-much-sugar-is-too-much. Last accessed October 15, 2024.
21. Dunn C, Gao KJ, Soto MJ, Bleich SN. Disparities in fast-food consumption in the U.S. by race and ethnicity, National Health and Nutrition Examination Survey 2017–2018. American Journal of Preventive Medicine. 2021;61(4):e197-e201.
22. Fryar CD, Carroll MD, Ahluwalia N, Ogden CL. Fast food intake among children and adolescents in the United States, 2015–2018. National Center for Health Statistics. 2020;375:1-7.
23. American Dental Association. Nutrition and Oral Health. Available at https://www/ada/org/resources/ada-library/oral-health-topics/nutrition-and-oral-health. Last accessed October 15, 2024.
24. Cleveland Clinic. Living with Type 2 Diabetes. Available at https://my.clevelandclinic.org/health/diseases/21501-type-2-diabetes. Last accessed October 15, 2024.
25. Andreyeva T. Large state variation in sugar-sweetened beverage purchases: what we learn from the beverage industry data. Current Developments in Nutrition. 2021;5(12):nzab128.
26. Center for Science in the Public Interest. Sugary Drinks. Available at https://www.cspinet.org/advocacy/nutrition/sugary-drinks. Last accessed October 15, 2024.
27. Calcaterra V, Cena H, Magenes VC, et al. Sugar-sweetened beverages and metabolic risk in children and adolescents with obesity: a narrative review. Nutrients. 2023;15:702.
28. Mayo Clinic. Cavities and Tooth Decay. Available at https://www.mayoclinic.org/diseases-conditions/cavities/symptoms-causes/syc-20352892. Last accessed October 15, 2024.
29. Munoz-Urtubia N, Vega-Munoz A, Estrada-Munoz C, et al. Healthy behavior and sports drinks: a systematic review. Nutrients. 2023;5:2915.
30. Rosdy NMMNM, Amin NASM, Roslan N. Erosive potential and sugar content of popular beverages: a double whammy for dentition. International Journal of Dentistry. 2023;2023:9924186.
31. Ogundijo DA, Tas AA, Onarinde BA. Age, an important sociodemographic determinant of factors influencing consumers' food choices and purchasing habits: an English university setting. Front Nutr. 2022;9:858593.
32. U.S. Department of Agriculture. Diet Quality and Nutrition. Available at https://www.ers.usda.gov/topics/food-choices-health/diet-quality-nutrition/background. Last accessed October 15, 2024.
33. Mengarelli CA, Kirchoff C, Palacios C. College students' perception of snacks sold in vending machines in the U.S.: a mixed-methods study. Frontiers in Nutrition. 2021;8:742121.
34. Whatnall MC, Patterson AJ, Hutchesson MJ. Effectiveness of nutrition intervention in vending machines to encourage the purchase and consumption of healthier food and drinks in the university setting: a systematic review. Nutrients. 2020;12:876.
35. Centers for Disease Control and Prevention. Smart Snacks and School Vending Machines. Available at https://www.cdc.gov/healthyschoold/nutrition/smartsnacks.htm. Last accessed October 15, 2024.
36. U.S. Department of Agriculture. A Guide to Smart Snacks in School. Available at https://fns-prod.azureedge.us/sites/default/files/resource-files/smartsnacks.pdf. Last accessed October 15, 2024.
37. Benson M. Vending Machines in Schools: Favorable and Profitable. Available at https://www.vendinglocator.com/blog/vending-machines-in-schools-both-favorable-and-profitable. Last accessed October 15, 2024.
38. Griffiths ML, Powell E, Usher L, et al. The health benefits and cost-effectiveness of complete healthy vending. PLoS ONE. 2020;15(9).
39. Mahmood L, Flores-Barrantes P, Moreno LA, et al. The influence of parental dietary behaviors and practices on children's eating habits. Nutrients. 2021;13:1138.
40. Devitt M. Parents Encouraged to Improve Children's Diet, Activity Levels. Available at https://www.aafp.org/news/health-of-the-public/parents-children-food-choices.html. Last accessed October 15, 2024.
41. Dimitratos SM, Swartz JR, Laugero KD. Pathways of parental influence on adolescent diet and obesity: a psychological stress-focused perspective. Nutrition Reviews. 2022;80(7):1800-1810.
42. Centers for Disease Control and Prevention. Improve Your Eating Habits. Available at https://www.cdc.gov/healthyweight/losing_weight/eating_habits.html. Last accessed October 15, 2024.
43. Przybylowicz KE, Danielewicz A. Eating habits and disease risk factors. Nutrients. 2022;14:3143.
44. Mackenbach JD, Ibouanga EL, van der Veen MH, et al. Relation between the food environment and oral health-systematic review. European Journal of Public Health. 2022;32(4):606-616.
45. Sexton C. The High Cost of Healthy Foods Linked to Malnutrition Across the Globe. Available at https://www.earth.com.news-cost-healthy-foods-malnutrition. Last accessed October 15, 2024.
46. Ney J. Food Deserts and Inequality. Available at https://www.socialpolicylab.org/post/grow-your-blog-community. Last accessed October 15, 2024.
47. Daniel C. Is healthy eating too expensive? How low-income parents evaluate the cost of food. Social Science and Medicine. 2020;248:112823.
48. Sina E, Boakye D, Christianson L, Ahrens W, Hebestreit A. Social media and children's and adolescents' diets: a systematic review of the underlying social and physiological mechanisms. American Society of Nutrition. 2022;13(3):913-937.
49. American Academy of Pediatric Dentistry. Policy on Early Childhood Caries (ECC): Consequences and Preventive Strategies. Available at https://www.aapd.org/globalassets/media/policies_guidelines/p_eccconsequences.pdf. Last accessed October 15, 2024.
50. Tungare S, Paranjpe AG. Early childhood caries. StatPearls. Treasure Island, FL: StatPearls Publishing; 2024.
51. National Institute of Dental and Craniofacial Research. Dental Caries (Tooth Decay) in Children Ages 2-11 Years. Available at https://www.nidcr.nih.gov/research/data-statistics/dental-caries/children. Last accessed October 15, 2024.
52. National Institute of Dental and Craniofacial Research. Dental Caries (Tooth Decay) in Adolescents (Ages 12 to 19 Years). Available at https://www.nidcr.nih.gov/research/data-statistics/dental-caries/adolescents. Last accessed October 15, 2024.
53. Wulandari ER, Lindayani L, Herdiman H. The effect of motivational interviewing on adolescent behaviors: a literature review. KnowledgeE KNE Publishing. 2022;995-1003.
54. Mutschler C, Naccarato E, Rouse J, et al. Realist-informed review of motivational interviewing for adolescent health behaviors. Systematic Reviews. 2018;7:109.
55. Centers for Disease Control and Prevention. Water Fluoridation Data and Statistics. Available at https://www.cdc.gov/fluoridation/statistics/index.htm. Last accessed October 15, 2024.
56. Wambogo E, Reedy J, Shams-White M, et al. Sources of energy, empty calories, added sugars, and solid fats among children and adolescents 2–28 years in the United States. Current Developments in Nutrition. 2020;4(Suppl 2):296.
57. American Dental Association. Aging and Dental Health. Available at https://www.ada.org/resources/ada-library/oral-health-topics/aging-and-dental-health. Last accessed October 15, 2024.
58. Vespa J, Medina L, Armstrong DM, U.S. Census Bureau. Demographic turning points for the United States: Population projections for 2020 to 2060. Available at https://www.census.gov/content/dam/Census/library/publications/2020/demo/p25-1144.pdf. Last accessed October 15, 2024.
59. Janto M, Iurcov R, Daina CM. Oral health among elderly, impact on life quality, access of elderly patients to oral health services and methods to improve oral health: a narrative review. Journal of Personalized Medicine. 2022;12:372.
60. Zhang J, Lo ECM. Epidemiology of dental root caries: a review of risk factors. Frontiers of Oral and Maxillofacial Medicine. 2020;2:5.
61. The American Dental Association. The Caregiver's Guide to Dental Health. Available at https://www.mouthhealthy.org/life-stages/adults/caregivers-guide-adults-over-60. Last accessed October 15, 2024.
62. National Institute of Dental and Craniofacial Research. Dry Mouth. Available at https://www.nidcr.nih.gov/health-info/dry-mouth. Last accessed October 15, 2024.
63. Farooq I, Bugshan A. The role of salivary contents and modern technologies in the remineralization of dental enamel: a narrative review. F1000 Research. 2021;9:171.
64. American Dental Association. Saliva. Available at https://www.mouthhealthy.org/all-topics-a-z/saliva. Last accessed October 15, 2024.
65. Talha B, Swarnkar SA. Xerostomia. StatPearls. Treasure Island, FL: StatePearls Publishing; 2024.
66. Toan NK, Ahn S-G. Aging-related metabolic dysfunction in the salivary gland: a review of the literature. International Journal of Molecular Sciences. 2021;22:5835.
67. Wynn RL, Meiller TF, Crossley HL. Drug Information Handbook for Dentistry. 28th ed. New York, NY: Wolters Kluwer Clinical Drug Information, Inc.; 2022.
68. Crouch B. Living with Sjogren's: One RDH's Advice to Dental Professionals and Dry Mouth Sufferers. Available at https://dentistryiq.com/dental-hygiene/article/14182372/sjogrens-syndrome-advice-from-a-registered-dental-hygienist. Last accessed October 15, 2024.
69. Kapourani A, Kontogiannopoulos KN, Barmpalexis P. A review on the role pilocarpine on the management of xerostomia and the importance of the topical administration systems development. Pharmaceuticals. 2022;15(6):762.
70. Wallace A. Fluoride: What's New, What's Not, and What Do Dental Patients Need to Know. Available at https://www.dentistryiq.com/dental-hygiene/articvle/14305769/fluoride-whats-new-whats-not-and-what-do-dental-patients-meed-to-know. Last accessed October 15, 2024.
71. Ellington D. Managing Enamel Demineralization. Available at https://dimensionsofdentalhygiene.com/article/managing-enamel-demineralization. Last accessed October 15, 2024.
72. Nassar Y, Brizuela M. The role of fluoride on caries prevention. StatPearls. Treasure Island, FL: StatePearls Publishing; 2023.
73. Centers for Disease Control and Prevention. Bottled Water. Available at https://www.cdc.gov/fluoridation/faqs/bottled_water.htm. Last accessed October 15, 2024.
74. American Dental Association. Fluoride: Topical and Systemic Supplements. Available at https://www.ada.org/resources/ada-library/oral-health-topics/fluoride-topical-and-systemic-supplements. Last accessed October 15, 2024.
75. Turkistani J. The modes of dental caries prevention with xylitol. Online Journal of Dentistry and Oral Health. 2020;3(1).
76. Bisla I. Review on role of xylitol in remineralization of dental caries. International Journal of Dental and Medical Sciences Research. 2021;3(2):51-64.
77. Wu Y-F, Salamanca E, Chen I-W. Xylitol-containing chewing gum reduces cariogenic and periodontopathic bacteria in dental plaque-microbiome investigation. Frontiers in Nutrition. 2022;9:882636.
78. Watts M. Xylitol. Available at https://www.diabetics.co.uk/sweetners/xylitol.html. Last accessed October 15, 2024.
79. American Dental Association. Chewing Gum. Available at https://www.ada.org/resources/ada-library/oral-health-topics/chewing-gum. Last accessed October 15, 2024.
80. Zen I, Delbem ACB, Martins TP, et al. Evaluation of solutions containing fluoride, sodium trimetaphosphate, xylitol and erythritol, alone or in different associations, on dual-species biofilms. International Journal of Molecular Sciences. 2023;24:12910.
81. Howell N. A Refresher to Caries Risk Management Strategies. Available at https://www.todaysrdh.com/a-refresher-to-caries-risk-management-strategies. Last accessed October 15, 2024.
82. Al Dhubayb S, Sultan MA, Sudairi SA. Ability of dentists and students to detect caries by using the International Caries Detection and Assessment System. Clinical, Cosmetic and Invetsigational Dentistry. 2021;13:379-387.
83. McDonald Z. 8 Surprising Things that Put You At Risk for Cavities. Available at https://www.health.com/surprising-things-that-put-you-at-risk-for-cavities-7488060. Last accessed October 15, 2024.
84. Pocket Dentistry. Evidence-Based Dentistry Caries Risk Assessment and Disease Management. Available at https://pocketdentistry.com/evidence-based-dentistry-caries-risk-assessment-and-disease-management. Last accessed October 15, 2024.
85. Featherstone JDB, Crystal YO, Alston PA. Comparison of four caries risk assessment methods. Frontiers in Oral Health. 2021;2:656558.
86. National Institute of Dental and Craniofacial Research. Oral health across the lifespan: adolescents. In: Oral Health in America: Advances and Challenges. Bethesda, MD: National Institute of Dental and Craniofacial Research; 2021.
Mention of commercial products does not indicate endorsement.