This course will be applicable to healthcare professionals who use the computer in their daily work or who encounter patients with carpal tunnel syndrome. An evaluation of available treatments for a diagnosis of computer-related injury will be provided. According to the Bureau of Labor and Occupational Safety and Health Association, certain professions are at risk for overuse injuries of the hand, fingers, and wrist. Identifying these occupations and other risk factors will be reviewed. Numerous research studies regarding the importance of ergonomics will be cited, and checklists to analyze computer workstations will be provided. This will include identification of available alternative devices and training methods to reduce the incidence of carpal tunnel syndrome. Finally, office safety programs and computer-related work claims will be reviewed in order to reduce these types of injuries.
This course is designed for physicians, nurses, occupational therapists, physical therapists, and any healthcare professionals who may encounter patients with carpal tunnel syndrome or who use the computer everyday.
The purpose of this course is to provide healthcare professionals with awareness of how to diagnose carpal tunnel syndrome, based on specific signs and symptoms and appropriate diagnostic tests, and of interventions available to treat and/or prevent the condition.
Upon completion of this course, you should be able to:
- Define carpal tunnel syndrome, and identify the causes and contributing factors.
- Identify conditions that may mimic carpal tunnel syndrome.
- Describe the methods and tools currently used to diagnose carpal tunnel syndrome.
- Discuss the recommended treatment options for carpal tunnel syndrome.
- Discuss potential prevention strategies for patients who may be at risk for developing carpal tunnel syndrome, including consider- ations for non-English-proficient patients.
Charlene H. Grafton, RN, BS, MS, CCM, is licensed in two states as a Registered Nurse and was nationally certified as a Case Manager. She has worked as a Qualified Rehabilitation Provider and an Independent Nurse Case Manager. She was selected as Who's Who by American Colleges and Universities, American Nursing and also by the International Tennis Federation. Also, she is a Veteran of the Army Nurse Corps, First Lieutenant. Ms. Grafton has demonstrated her natural leadership style through volunteer work and participation on various Boards of Directors, such as the Jaycee Jaynes, Nevada Community Enrichment Program, Southern Nevada Continuity of Care Association, Florida's Governor's Council on Fitness and Sports, Nevada Tennis Association, National Senior Women's Tennis Association, Health Insight (Medicare and Medicaid) and the Executive Women's Golf League. In addition, she has presented papers and shown her teaching abilities by speaking at local, state, regional, national and international forums on a variety of subjects, including teaching techniques, lateral dominance, fitness and case management. As a writer, she has published two books about dominance and researched in areas of coordination, laterality, and sidedness from gifted to learning disabilities/problems and functional independence. Her work has also appeared in trade magazines.
Contributing faculty, Charlene H. Grafton, RN, BS, MS, CCM, has disclosed no relevant financial relationship with any product manufacturer or service provider mentioned.
John M. Leonard, MD
Mary Franks, MSN, APRN, FNP-C
The division planners have disclosed no relevant financial relationship with any product manufacturer or service provider mentioned.
Sarah Campbell
The Director of Development and Academic Affairs has disclosed no relevant financial relationship with any product manufacturer or service provider mentioned.
The purpose of NetCE is to provide challenging curricula to assist healthcare professionals to raise their levels of expertise while fulfilling their continuing education requirements, thereby improving the quality of healthcare.
Our contributing faculty members have taken care to ensure that the information and recommendations are accurate and compatible with the standards generally accepted at the time of publication. The publisher disclaims any liability, loss or damage incurred as a consequence, directly or indirectly, of the use and application of any of the contents. Participants are cautioned about the potential risk of using limited knowledge when integrating new techniques into practice.
It is the policy of NetCE not to accept commercial support. Furthermore, commercial interests are prohibited from distributing or providing access to this activity to learners.
Supported browsers for Windows include Microsoft Internet Explorer 9.0 and up, Mozilla Firefox 3.0 and up, Opera 9.0 and up, and Google Chrome. Supported browsers for Macintosh include Safari, Mozilla Firefox 3.0 and up, Opera 9.0 and up, and Google Chrome. Other operating systems and browsers that include complete implementations of ECMAScript edition 3 and CSS 2.0 may work, but are not supported. Supported browsers must utilize the TLS encryption protocol v1.1 or v1.2 in order to connect to pages that require a secured HTTPS connection. TLS v1.0 is not supported.
The role of implicit biases on healthcare outcomes has become a concern, as there is some evidence that implicit biases contribute to health disparities, professionals' attitudes toward and interactions with patients, quality of care, diagnoses, and treatment decisions. This may produce differences in help-seeking, diagnoses, and ultimately treatments and interventions. Implicit biases may also unwittingly produce professional behaviors, attitudes, and interactions that reduce patients' trust and comfort with their provider, leading to earlier termination of visits and/or reduced adherence and follow-up. Disadvantaged groups are marginalized in the healthcare system and vulnerable on multiple levels; health professionals' implicit biases can further exacerbate these existing disadvantages.
Interventions or strategies designed to reduce implicit bias may be categorized as change-based or control-based. Change-based interventions focus on reducing or changing cognitive associations underlying implicit biases. These interventions might include challenging stereotypes. Conversely, control-based interventions involve reducing the effects of the implicit bias on the individual's behaviors. These strategies include increasing awareness of biased thoughts and responses. The two types of interventions are not mutually exclusive and may be used synergistically.
#91954: Carpal Tunnel Syndrome
While carpal tunnel syndrome is possibly the most common nerve disorder diagnosed today, it is not a new condition born of the information technology age [1]. Compression of the median nerve of the hand was first reported in 1854 by Sir James Paget. In 1880, James Putnam reported on a series of patients who were experiencing pain and paresthesia in the median nerve of the hand. In 1913, Pierre Marie and Charles Foix offered a description of the pathology of median nerve compression, and in 1933, Sir James Learmonth reported the first release treatment for median nerve compression [2].
Determining the causes of carpal tunnel syndrome remains an area of ongoing research, discussion, and disagreement among healthcare professionals. Historically, some have concluded that carpal tunnel syndrome is purely an occupational disorder with clear-cut associations to repetitive manual movements or work tasks. Others have concluded that the causes of carpal tunnel syndrome are unknown, unproven, or based on multiple factors.
Despite the ongoing disagreement about its causes, the U.S. Department of Labor Bureau of Labor Statistics reports that carpal tunnel syndrome exacts a significant toll each year on the health and productivity of the U.S. workforce. The rate of reported cases, while declining in recent years, accounts for the second highest number of days away from work among all work-related musculoskeletal disorders [12,13,14]. Approximately 5,650 cases of occupational injury or illness resulting from carpal tunnel syndrome and involving time away from work (median: 28 days) are reported each year, resulting in lost wages, increased healthcare costs in local communities, and added costs to state workers' compensation programs.
The purpose of this course is to provide information about the causes of carpal tunnel syndrome and to review current methods of diagnosis and treatment and recommended prevention strategies. It begins by defining carpal tunnel syndrome, which includes a discussion of common symptoms, causes and contributing factors, and conditions that mimic carpal tunnel syndrome. Current diagnostic methods and tools are reviewed, and current treatment options and recommended prevention strategies are discussed. The course concludes with a simulated case study that describes the course of treatment for a patient who presents with chronic symptoms of carpal tunnel syndrome.
Carpal tunnel syndrome is generally associated with such umbrella terms as repetitive stress injuries, work-related upper extremity disorders, musculoskeletal disorders, entrapment neuropathies, and cumulative trauma disorders [16,18]. Specifically, carpal tunnel syndrome is a painful disorder of the wrist and hand that occurs when the median nerve (which runs from the hand to the forearm) becomes compressed [1,19].
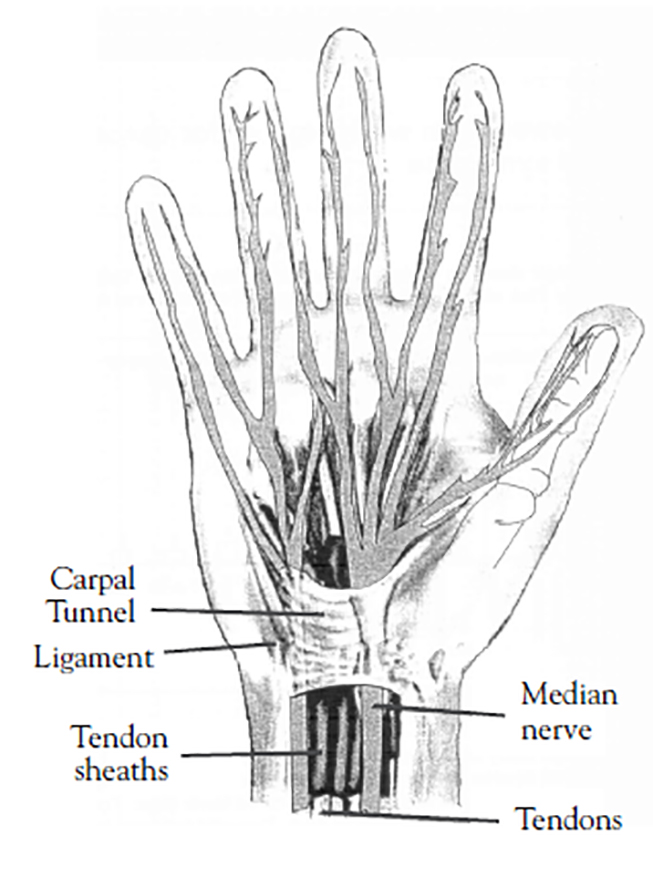
The carpal tunnel is a narrow passageway on the palm side of the wrist. Surrounded by bones and ligaments, the carpal tunnel houses and protects the tendons of the hand and the median nerve, which controls sensations to the thumb and fingers (Figure 1). When the median nerve becomes pinched or compressed (due to swelling or irritation in adjacent tissues or tendons), the result can be pain, numbness, hand weakness, and in extreme cases, loss of hand function. Cases of bilateral carpal tunnel syndrome have been reported, but typically only one hand is affected [1,20,21]. Carpal tunnel syndrome is rare in children; it usually occurs only in adults [9].
The symptoms of carpal tunnel syndrome typically appear gradually and may include [9,20]:
Numbness, burning, or tingling in the fingers and palm of the hand
Pain in the wrist, palm, or forearm, especially during use
Decreased grip strength
Weakness in the thumb
Sensation of swollen fingers, whether or not swelling is apparent
Difficulty distinguishing between hot and cold
Symptoms may cause waking during the night with the urge to "shake out" the hand or wrist. Symptoms may occur with activities that require prolonged grasping and/or flexing of the wrist (e.g., driving, holding a book). Left untreated, carpal tunnel syndrome can progress to persistent numbness and permanent loss of hand function. In severe and chronic cases, irreversible muscle damage or atrophy may occur [1,9,23]. Complete sensory loss in the hand has also been reported.
Researchers have identified a variety of factors that may cause or contribute to the development of carpal tunnel syndrome. These factors include the presence of other health conditions, engagement in an occupation or activity that involves repetitive use of the hand, and the presence of a range of personal/physical factors that may indicate a predisposition to carpal tunnel syndrome [1,3,9,13,19,20,26,28,30]. There is general agreement that carpal tunnel syndrome is multifactorial and that the exact cause is unknown [31]. Also, the role of individual contributing factors in the development and prognosis of carpal tunnel syndrome is uncertain. In some instances, no cause can be identified [9]. However, the pathophysiology seems to involve alterations of fluid balance (e.g., fluid retention), hormonal changes, and accompanying peripheral tissue edema, which may be precipitated by a variety of disorders and bodily changes [47].
Several health conditions are associated with the presence of carpal tunnel syndrome and may be contributing factors in its development. The most commonly noted co-occurring health conditions are noninflammatory synovial fibrosis, metabolic syndrome, diabetes, thyroid disorders, rheumatoid arthritis, pregnancy, and menopause.
Noninflammatory synovial fibrosis is the most common pathologic finding in patients with idiopathic carpal tunnel syndrome [32,33]. This finding supports the belief that chronic or repetitive injury to the median nerve, resulting in tissue swelling, compression of the nerve, or injury to the outside layers of the nerve, is a primary factor in the development of carpal tunnel syndrome [9,19,32,34,35,36]. Studies of patients with idiopathic carpal tunnel syndrome have revealed alterations in the material properties of the synovial tissue, irregular patterns of tendon movement, and an absence of the normal interconnections between tissue layers that surround the median nerve [32,36,37]. The long-term effect of these altered properties is unknown.
Metabolic disorders have a well-documented association with carpal tunnel syndrome [1,19,28,39,40,41]. This is particularly true of disorders that directly affect the nerves of the body by increasing their susceptibility to compression [9]. Metabolic syndrome, which is characterized by abdominal obesity, hypertension, hyperlipidemia, and insulin resistance, is frequently associated with the presence of carpal tunnel syndrome [1,19,28,39]. The incidence of metabolic syndrome has been found to be higher in patients with carpal tunnel syndrome. Also, in patients with metabolic syndrome, the symptoms may be more severe [39].
Diabetes has been linked with several debilitating musculoskeletal disorders of the hand, including carpal tunnel syndrome [20,40]. The incidence of carpal tunnel syndrome is higher in individuals with diabetes than in those without. Some studies have found that presence of the syndrome appears to be related more to the duration of the diabetes than to the patient's gender or age [40,41]. A 2014 case-controlled retrospective analysis of nearly 1,600 patient records found that type 2 diabetes was not an independent risk factor for carpal tunnel syndrome, despite the increased prevalence of diabetes in the carpal tunnel group [4]. In this analysis, the prevalence of carpal tunnel syndrome was not influenced by duration of diabetes, glycemic control, or microvascular complications.
Studies conducted to determine the prevalence of musculoskeletal problems with respect to thyroid function have indicated that musculoskeletal disorders, including carpal tunnel syndrome, frequently accompany thyroid conditions; however, a 2014 meta-analysis found evidence of publication bias and poor control in many studies investigating this association [5,9,28,44]. Symptoms of carpal tunnel syndrome commonly appear in hypothyroid patients (40% higher compared to healthy controls), including patients with normally functioning thyroid glands [5,28]. The combination of hypothyroidism and carpal tunnel syndrome appears to be more prevalent in the elderly [46]. It is important to note that the risk of developing carpal tunnel syndrome increases when thyroid disease is untreated [47]. It is clear that more well-controlled studies are needed to elucidate the effect of thyroid disease on carpal tunnel compression.
Tophaceous gout, characterized by deposits of sodium urate (tophi) in the joints and external ear, is another health condition associated with carpal tunnel syndrome [38,48]. Patients (particularly men) with a history of gout are at increased risk for developing carpal tunnel syndrome, even when appropriate medical treatment is given [38].
Carpal tunnel syndrome has become an increasingly recognized problem in patients who undergo long-term hemodialysis [50,51]. A strong correlation has been noted between the duration of hemodialysis and the appearance of carpal tunnel syndrome. Arteriovenous fistula and amyloidosis have been identified as possible causes for the development of the syndrome in this patient population [50,52,53].
Rheumatoid arthritis has also been associated with carpal tunnel syndrome [9,54]. Patients with rheumatoid arthritis and carpal tunnel syndrome reportedly have a significantly higher incidence of enlarged areas of the median nerve than do arthritic patients and healthy persons without carpal tunnel syndrome. However, whether rheumatoid arthritis has a role in the development of carpal tunnel syndrome is uncertain, and in 2015, one study reported a similar rate of carpal tunnel syndrome in individuals with rheumatoid arthritis and those without the disorder [8,55].
Female gender is an independent risk factor for carpal tunnel syndrome, and fluid retention during pregnancy or menopause is frequently associated with development of the disease [1,19,39,47,54,56]. As many as 62% of women experience symptoms of carpal tunnel syndrome during pregnancy, although the rate varies considerably in the available literature [47,57]. Reduced pain tolerance associated with psychologic distress, depression, and/or anhedonia during pregnancy may further exacerbate uncomfortable sensations [47]. When onset is during pregnancy, symptoms usually appear in both hands and during the third trimester. Previous pregnancy does not increase the risk for carpal tunnel syndrome, but patient weight gain during pregnancy does. Pregnancy-induced carpal tunnel syndrome usually resolves spontaneously within 6 to 12 weeks following delivery, with significant improvement noted between weeks 6 and 12 postpartum [20,56].
Carpal tunnel syndrome has been reported among a variety of occupations, including clerical workers (e.g., cashiers, data entry workers, typists), assembly line workers (manufacturing, sewing, finishing, cleaning, meat packing), computer workers, and some healthcare professionals [3,9,10,20,25,26,27,59,60]. Information about the association of carpal tunnel syndrome with repetitive activity is now so widely available and easily obtained that many workers self-diagnose before obtaining a medical assessment.
Although a causal relationship between specific work activities and carpal tunnel syndrome has not been firmly established, studies have shown that intensive (i.e., greater than 4 kg of hand force), repetitive motion (at intervals less than 10 seconds), vibration, and extreme postures of the hand and wrist during job performance may contribute to the development of carpal tunnel syndrome by temporarily increasing pressure in the carpal tunnel, which threatens the viability of the median nerve and affects normal hand function [3,27,54,59,61,67]. However, many researchers feel that assigning work as the cause of carpal tunnel syndrome makes it easier for individuals to ignore their responsibility to address correctable lifestyle factors that may contribute to development of the syndrome. Furthermore, to date there is no solid evidence that computer operators are at risk, but the prevalence of self-reported carpal tunnel syndrome among this cohort is greater than 10% [25,26].
Obesity and lack of physical fitness (particularly no activities involving wrist strain) are considered to be primary risk factors in the development of carpal tunnel syndrome [1,7,8,40,67,68,69,70,106]. Obese individuals are more likely than non-obese individuals to have chronic health conditions, including diabetes, hypertension, and osteoarthritis [73]. The presence of these conditions, rather than excess body weight alone, may be the reason for a higher prevalence of carpal tunnel syndrome in obese individuals [74].
As noted, women are much more likely than men to develop carpal tunnel syndrome [7,9,67]. The dominant hand is usually affected first and produces the most severe pain [7]. The increased incidence in women may be partly due to hormonal factors, but in general, it is believed to be related to a propensity to and higher frequency of musculoskeletal problems among women [75]. The type of work performed may also be a contributing factor. Women who perform unskilled or semiskilled work (e.g., assembly work) appear to have a higher incidence of carpal tunnel syndrome than women who perform in higher-skilled jobs (e.g., computer work) [26,76]. Women with carpal tunnel syndrome also have a higher absence rate from work and a longer duration of disability than men.
Inherited variations in the size and shape of the hand and wrist, or in the size of the carpal tunnel and its contents, may predispose some individuals to carpal tunnel syndrome [20,31,77]. Individuals with bilateral disease reportedly also have a greater incidence of familial disease than those with either unilateral disease or no carpal tunnel syndrome [78].
There are many conditions with presenting symptoms that may mimic carpal tunnel syndrome. Consideration of these conditions during the assessment process will ensure accurate diagnosis and effective treatment.
Hand-arm vibration syndrome (HAVS) is often misdiagnosed as carpal tunnel syndrome due to similar symptoms and causes. Further complicating diagnosis is the fact that the two syndromes may coexist. HAVS consists of an array of injuries to the nerves, muscles, and tendons of the wrist and hand and commonly afflicts occupational groups who use handheld vibrating tools. The symptoms of HAVS include tenderness or pain and swelling of the fingers; numbness, weakness, or tingling in the fingers; reduced sensitivity to heat and cold; and loss of dexterity and coordination in the fingers [81].
Pronator syndrome and anterior interosseous nerve syndrome are median nerve compressions that may cause pain, tenderness, aching in the wrist, difficulty moving the index and middle fingers, a feeling of poor coordination, and paresthesia that extends into the hand. These syndromes are rare but should be suspected if a patient with carpal tunnel syndrome fails to respond to treatment [82].
Cervical spondylosis is a disorder caused by abnormal wear on the cervical vertebrae, resulting in chronic degeneration of the cervical spine and eventually weakness, compression of one or more nerve roots, and pain in the neck and arm [83]. Hand paresthesia is common. Because this symptom is also common in carpal tunnel syndrome, additional symptoms should be evaluated to properly distinguish between cervical spondylosis and carpal tunnel syndrome. Patients with cervical spondylosis generally have a higher incidence of neck and lower limb pain than patients with carpal tunnel syndrome [84].
Cubital tunnel syndrome is caused by pressure on the ulnar nerve at the elbow. When the pressure increases enough to disturb normal nerve function, pain, numbness, and tingling may occur in the forearm or hand. Most often this pain is present in the ring and little fingers. Other symptoms that mirror carpal tunnel syndrome include decreased grip strength, weakness while pinching, and a feeling of clumsiness [1,9,85]. Individuals with cubital tunnel syndrome are more likely than individuals with carpal tunnel syndrome to present with muscle atrophy [23].
Tenosynovitis involves inflammation of the tendon and tendon sheath and is also known as de Quervain tenosynovitis of the wrist [86]. When the tendons at the base of the thumb become irritated or inflamed this causes the tunnel around the tendon to swell and results in pain and difficulty grasping and holding objects. Overuse is the most common cause [86]. New repetitive activity, hormonal fluctuations associated with pregnancy and breastfeeding, and wrist fractures also are possible causes of de Quervain tenosynovitis [87].
Stenosing tenosynovitis, also referred to as "trigger finger," occurs when the pulley/tendon relationship between the hand and fingers is restricted by thickening or swelling at the base of the fingers. This creates pain and a distinctive catching, popping, or locking action in the finger or thumb. A cycle of triggering, inflammation, and swelling is common. Like carpal tunnel syndrome, stenosing tenosynovitis has been associated with other health conditions, such as gout, diabetes, and rheumatoid arthritis. In many cases, the actual cause is not clear [88].
Early diagnosis of carpal tunnel syndrome is important to prevent muscle atrophy or damage to the median nerve that cannot be reversed by treatment [1,9]. Early diagnosis, including a physical examination, medical history, routine laboratory tests, and imaging, can also help to identify or rule out other health conditions that may present with similar signs and symptoms and require specialized treatment [89,90,127]. The physical examination should include specific testing, such as Phalen's maneuver or Tinel's sign, that can produce the symptoms of carpal tunnel syndrome [9,20]. In elderly patients, particular attention should be given to the objective evidence of carpal tunnel syndrome rather than subjective complaints [91].
Several tests are available to assess the nerves and tendons of the hand. While these tests are a vital step in diagnosing carpal tunnel syndrome, additional testing is necessary to confirm any findings.
During Phalen's maneuver (wrist-flexion test), tingling or numbness may be produced by asking the patient to flex the wrists while extending the fingers. If symptoms occur within one minute, the presence of carpal tunnel syndrome is suggested [9,23]. A positive result with Phalen's maneuver may indicate severe carpal tunnel syndrome [92]. The test is not a reliable indicator of carpal tunnel syndrome in the diabetic population [93].
Tinel's sign, also referred to as Tinel's test, consists of pressing or tapping on the median nerve in the patient's wrist. If tingling in the fingers or a shock-like sensation occurs, the presence of carpal tunnel syndrome is suggested [9,23]. A positive result on Tinel's sign is not an indication of the syndrome's severity [92]. A new test, the scratch collapse test, has shown higher sensitivity (64%) than Tinel's sign for carpal tunnel syndrome and a positive predictive value of 99% [94,95]. With this test, the examiner lightly scratches the patient's skin over the area of nerve compression as the patient performs resisted shoulder external rotation bilaterally. Momentary loss of resistance on the affected side is considered a positive test.
Other tests that may be part of the physical examination include the flick sign and the hand elevation test. In testing for the flick sign, the patient flicks the hand and wrist as if shaking a thermometer. If tingling or a shock-like sensation occurs, the presence of carpal tunnel syndrome is suggested; however, this test has been found to be of limited usefulness [96]. During the hand elevation test, the patient elevates the hand above the head as high as comfortably possible for about one minute. Symptoms of tingling and numbness indicate the presence of carpal tunnel syndrome. The hand elevation test has been found to be more specific than Phalen's maneuver and Tinel's sign, but overall, no statistically significant differences are apparent between the three tests, which all possess low sensitivity and low specificity compared to electrodiagnostics and/or neuromuscular ultrasound [7,97].
In the 2019 Academy of Orthopedic Physical Therapy clinical practice guidelines, monofilament threshold testing and static two-point discrimination (2PD) testing were each given evidence ratings of A, while Phalen's maneuver and Tinel's sign were each given B ratings [89]. Loss of two-point discrimination at 5 mm or less in in the median innervated digits is one of the elements of the CTS-6 evaluation tool, which has been recommended in the 2024 AAOS carpal tunnel management guidelines as a stand-alone diagnostic in leu of routine use of ultrasound and/or electrophysiologic studies [106].
After the diagnosis of carpal tunnel syndrome is suggested, it may be confirmed with additional testing [1,6,7,9,89]. Available methods include electrodiagnostic (electrophysiologic) studies, ultrasonography, magnetic resonance imaging (MRI), computed tomography (CT), and pressure-specified sensorimotor devices (PSSDs). The efficacy of each method and combinations of methods for confirming the diagnosis of carpal tunnel syndrome is an area of ongoing research and discussion. Following are descriptions of these methods as well as guidelines and recommendations for their use. A summary of recommendations is provided in Table 1.
SUMMARY OF RECOMMENDATIONS FOR DIAGNOSING CARPAL TUNNEL SYNDROME
| Test | Recommendations |
|---|---|
| Phalen's maneuver | Reliable diagnostic test; useful to determine severity of CTS. |
| Ultrasonography | Useful, accurate; able to define cause of nerve compression and estimate symptom severity. Comparable to EDX but not accurate enough to replace NCS. Useful to support diagnosis of CTS. May be used as an initial screening test, but not recommended for routine use. Color Doppler more accurate than gray-scale. |
| Electrodiagnostic testing | Generally not recommended for diagnosis. |
| Electrophysiologic studies | More useful than US in diagnosing idiopathic CTS |
| Tinel's sign | Not always useful |
| Scratch collapse test | Higher sensitivity than Tinel's sign; very high positive predictive value of CTS. |
| Flick sign | Limited usefulness; use to reproduce symptoms of CTS and to confirm EDX diagnosis. |
| Hand elevation test | Diagnostic results comparable to Phalen's maneuver and Tinel's sign. |
| Wrist x-ray | May help to rule out other diagnoses. Limited usefulness for carpal tunnel diagnosis. |
| History/physical exam | Recommended for all patients to determine severity and rule out other diagnoses. Use in conjunction with sensory testing. |
| Other | MRI, CT, PSSDs not recommended. NDE, NS not recommended as substitute for EDX studies. |
| CTS = carpal tunnel syndrome; EDX = electrodiagnostic; NCS = nerve conduction study; US = ultrasonography; MRI = magnetic resonance imaging; CT = computed tomography; PSSDs = pressure-specified sensorimotor devices; NDE = nervepace digital electroneurometer; NS = neurosentinel. | |
The electrodiagnostic (EDX) study is a two-part electrical test that includes a nerve conduction study (NCS) and electromyography. The EDX study is conducted to assess nerve health in patients with complaints of pain, weakness, numbness, or tingling. During the nerve conduction portion of the carpal tunnel syndrome test, an electrode placed near the elbow side of the tunnel generates a mild electrical current. The impulse travels in the nerve through the carpal tunnel to the hand. The time it takes the impulse to travel to the hand indicates the health of the nerve; a delayed impulse indicates nerve damage. The electromyography portion of the test consists of placing small needles into a sampling of muscles that are supplied by the median nerve. The electrical impulses of the muscles are measured both at rest and upon contraction. Poor or abnormal muscle performance indicates severe nerve compression [1,48].
Many researchers and clinicians have concluded that for diagnosing carpal tunnel syndrome, EDX studies are most effective when used in conjunction with other diagnostic methods, when the diagnosis of carpal tunnel syndrome is uncertain, or when surgical treatment is being considered [109,127]. In its published guideline on the diagnosis of carpal tunnel syndrome, the American Academy of Orthopaedic Surgeons (AAOS) recommends against the use of EDX studies considering other standardized, low-cost options [106]. The AAOS finds little evidence to support EDX studies for other purposes, such as differentiating among diagnoses [101,106].
Ultrasonography is a method in which high frequency sound waves (ultrasonic echoes) produce images or photographs of organs and tissues. Ultrasonography can reveal impaired movement of the median nerve. Doppler ultrasonography changes the sound waves into images that can be viewed on a monitor and measures the direction and velocity of the object being studied. Gray-scale ultrasonography measures the strength of ultrasound echoes and records the strongest echoes as white and the weakest echoes in shades of gray [48]. Color Doppler ultrasonography is believed to be more accurate than gray-scale in diagnosing carpal tunnel syndrome due to the increased perception of the circulatory status of the median nerve [103].
Studies comparing ultrasonography to other methods for diagnosing carpal tunnel syndrome have yielded a variety of conclusions regarding its usefulness. For example, some researchers have concluded that ultrasonography is comparable to EDX, with the positive predictive value of ultrasound 100% in one study, and that it should be considered the initial diagnostic test of choice [6,110,111]. Other researchers have concluded that while ultrasonography is somewhat useful (e.g., when diagnosing idiopathic carpal tunnel syndrome), it is not an ideal method for estimating the severity of symptoms and nerve damage [82,104,105,110,112,113,114,115]. In 2024 the AAOS recommended against the routine use of ultrasound [106].
Magnetic resonance imaging has been used in the development of a biomechanical model of the wrist and carpal tunnel, which can help during evaluation of median nerve health [116,117]. Although MRI is less accurate than EDX studies for confirming a diagnosis of carpal tunnel syndrome, it has proved to be useful in grading the severity of the disorder in patients with idiopathic symptoms, in explaining persistent symptoms following surgery, and in predicting whether a patient will benefit from surgery [118,119,120]. The routine use of MRI is not recommended for diagnosing patients with suspected carpal tunnel syndrome [56,101].
Computed tomography uses x-rays to produce detailed, cross-sectional images of selected structures inside the body [48]. In the diagnosis of carpal tunnel syndrome, CT imaging provides a view of any structural abnormalities of the carpal tunnel and median nerve [121,122]. The routine use of CT technology is not recommended for diagnosing patients with suspected carpal tunnel syndrome [101].
A pressure-specified sensorimotor device is an electromechanical device that measures motor function and sensory loss. The use of PSSDs has been favorably compared to EDX studies for diagnosing carpal tunnel syndrome, but current research supporting PSSDs as diagnostic tools is lacking [122,123]. The routine use of PSSD technology for diagnosing patients with suspected carpal tunnel syndrome is not recommended [101].
Surgery, corticosteroids, nonsteroidal anti-inflammatory drugs (NSAIDs), diuretics, wrist splints, exercise, ultrasound therapy, laser therapy, and yoga are among the methods that have been recommended for the treatment of carpal tunnel syndrome [72,99,124,125,126]. Although no single treatment method has been universally accepted, there is agreement that the treatment of carpal tunnel syndrome should begin as early as possible and should include attention to underlying causes, such as diabetes or rheumatoid arthritis. There is also agreement that successful treatment depends on patient compliance with the treatment program [9,106].
In its 2024 practice guideline for the management of carpal tunnel syndrome (Table 2), the AAOS recommended that treatment decisions be based on [106]:
Communication between the patient and the physician, with active patient participation and physician input based on the physician's experience and skill
Evaluation of the patient's current quality of life with carpal tunnel syndrome
Discussion of applicable and available non-surgical options and procedures
AAOS RECOMMENDATIONS FOR TREATMENT OF CARPAL TUNNEL SYNDROME
| Treatment Method | Strength of Recommendationa |
|---|---|
| Recommendations For | |
| Surgical release of the transverse carpal ligament: either endoscopic or open carpal tunnel release, no difference in patient-reported outcomes | |
| NSAIDs or acetaminophen should be used for postoperative pain management | |
| Use of local anesthesia (rather than intravenous regional anesthesia; may offer longer pain relief after carpal tunnel release) | |
| Therapeutic ultrasound | |
| Perioperative use of aspirin | |
| Recommendations Against | |
| No long-term benefit of local steroid injections | |
| No benefit of oral treatments (diuretic, gabapentin, astaxanthin capsules, NSAIDs, or pyridoxine) compared to placebo | |
| No benefit of non-operative treatments (acupressure, insulin injection, heat therapy, magnet therapy, nutritional supplementation, oral diuretic, oral NSAID, oral anticonvulsant, phonophoresis) compared to placebo. | |
| No long-term patient reported benefit for oral corticosteroid, hyaluronic acid injection, hydro dissection, kinesiotaping, laser therapy, peloid therapy, perineural injection therapy, topical treatment, shockwave therapy, exercise, ozone injection, massage therapy, manual therapy, pulsed radiofrequency | |
| No benefit of prescription of pre-operative antibiotics | |
| No long-term benefit to platelet-rich plasma injection in non-operative treatment | |
| No benefit to routine supervised therapy versus home programs in the immediate postoperative period | |
| No benefit to routine postoperative immobilization after carpal tunnel release | |
| aStrength of Recommendation Descriptions | |
| Strength Visual | Evidence Quality |
| | Evidence from two or more "high" quality studies with consistent findings for recommending for or against the intervention. |
| | Evidence from two or more "moderate" quality studies with consistent findings, or evidence from a single "high" quality study for recommending for or against the intervention |
| | Evidence from two or more "low" quality studies with consistent findings or evidence from a single "moderate" quality study recommending for against the intervention or diagnostic or the evidence is insufficient or conflicting and does not allow a recommendation for or against the intervention. |
| | There is no supporting evidence. In the absence of reliable evidence, the guideline development group is making a recommendation based on their clinical opinion. Consensus statements are published in a separate, complimentary document. |
| aLevels of Evidence | |
| Strength Visual | Overall Strength of Evidence |
| | Strong |
| | Moderate |
| | Low strength evidence or conflicting evidence |
| | No evidence |
Patients will present with a wide variety of needs, choices, and access to non-operative alternatives. Even when well informed about available non-operative therapies, patients may opt for surgical treatment.
Before deciding on a course of treatment, healthcare professionals and patients should discuss the desired outcome. Is the goal symptom improvement only? Is it a permanent modification of leisure time and/or work activity? Is it surgery followed by a return to work? Establishing goals prior to treatment allows healthcare professionals and patients to measure success and track progress [20].
In addition to discussing desired outcomes, patient response to treatment should be assessed by one or more of the following instruments [64,65,66,71]:
Boston Carpal Tunnel Questionnaire: A disease-specific, patient-based outcome questionnaire measuring symptom severity and functional status of patients with carpal tunnel syndrome
Disabilities of the arm, shoulder, and hand (DASH) tool: A region-specific outcome measure of upper limb function
Michigan Hand Outcomes Questionnaire (MHQ): A region-specific (hand/wrist) instrument designed to evaluate patients prior to and after hand surgery
Patient Evaluation Measure (PEM): A patient-completed questionnaire
Short Form Health Survey (SF-36 or SF-12): The SF-36 is a generic measure of overall physical health used to assess the health of general populations; the SF-12 is a shorter alternative of the SF-36 frequently used in large population health surveys
Non-surgical treatments for carpal tunnel syndrome are typically offered to patients with mild-to-moderate symptoms and to those who are waiting to undergo surgery [63,72]. Non-surgical treatment methods are generally considered successful in treating carpal tunnel syndrome when they have produced measurable improvement in the patient's symptoms and functional ability within two to seven weeks. The AAOS suggests that surgery or additional non-surgical treatment be considered if improvement is not seen within this or another patient/physician determined timeframe [101].
Local corticosteroid injections and splinting have demonstrated short-term benefit and symptomatic relief in patients with mild or moderate carpal tunnel syndrome [60,62,63,101]. Based on patient preference and clinical judgment, the use of local steroid injections may be considered before surgery. Local steroids are not effective for long-term treatment of carpal tunnel syndrome [106].
Corticosteroid injection has been found to improve patient satisfaction, symptoms, and function when measured at intervals of 2, 4, 8, and 12 weeks. It demonstrates a more significant overall improvement in the symptoms of carpal tunnel syndrome than oral corticosteroids, but does not appear to provide a better long-term outcome (greater than six months) than splinting or NSAIDs. Two treatment injections do not appear to provide any added benefit when compared to one treatment injection [63,125].
Splinting has been found to improve patient satisfaction, symptoms, and function when measured at intervals of 2, 4, and 12 weeks. This may be particularly helpful when weighing the risks of surgery versus the benefits. Splinting is not recommended for use after routine carpal tunnel release surgery. The benefit of splinting for postoperative rehabilitation is undetermined [63,101,106]. The 2024 AAOS guidelines do not address splinting in the context of nonsurgical treatment.
NSAIDs are used to treat a variety of acute and chronic pain conditions, including carpal tunnel syndrome, but opinion varies as to their effectiveness and safety for long-term use [48,58,62,106]. Specifically, NSAIDs have been associated with gastrointestinal and cardiovascular risks and toxicity with long-term use [107]. Long-term NSAID use is strongly discouraged by the AAOS [106].
Diuretics and vitamin B6 (pyridoxine) may also help with temporary relief of symptomatic carpal tunnel syndrome, but their long-term benefits are unproven [56,62,63]. Acupuncture, yoga, exercise, laser therapy, activity modification, and ergonomic workplace modifications also have been mentioned as non-surgical treatment alternatives, but most experts agree that either this approaches have no benefit or that further research is needed to determine the viability and efficacy of these methods [9,17,49,62,63,106,125].
Carpal tunnel release is the preferred treatment for patients with chronic or severe carpal tunnel syndrome. It is achieved by either an open or endoscopic procedure [9,99,101,106]. Both types of surgery are generally performed on an outpatient basis under local anesthesia. Open release surgery involves making an incision of up to 2 inches at the base of the palm of the hand and cutting the transverse carpal ligament, which releases pressure on the median nerve [9,45]. Endoscopic surgery involves making a small, one-half inch incision at the wrist and introducing an arthroscope beneath the transverse carpal ligament. Using the scope as a guide, the ligament is cut, relieving pressure on the median nerve [9,17,45].
The choice of open or endoscopic surgery is generally guided by the surgeon's and patient's preferences [124]. The two methods have shown comparable complication and return-to-work rates; however, at least one expert has noted the functional difference between having a one-inch incision in the palm of the hand, versus a half-inch incision in a wrist crease [43,102]. Surgical outcomes in the elderly (70 years of age and older) can be less predictable than in younger patients; however, surgical treatment in this group has been associated with better symptom relief and improvement in function than non-surgical treatments [42,126].
Patients with bilateral carpal tunnel syndrome may require surgical release in both hands. When compared to consecutive release, simultaneous release has been shown to offer comparable disability durations and substantial cost savings [21].
Although the number of cases of carpal tunnel syndrome among U.S. workers has been declining, the resulting number of reported days away from work remains high [13]. This lost work time and decreased employee productivity have led employers to develop organizational approaches to managing employee health, safety, and productivity, with an emphasis on prevention and returning employees to work as quickly as possible [29,30]. Rising healthcare costs and the focus on preventing carpal tunnel syndrome have led researchers to study and recommend a variety of prevention strategies, including the application of ergonomic principles to job and workstation design, the use of ergonomically sound equipment (including ergonomic keyboards and dual numeric keyboards), the development of predictive models, and the use of exercise regimens and patient education and safety programs [17,22,24].
The concept of work-related carpal tunnel syndrome, though unproven, has had a significant societal impact in the United States [11]. The U.S. Department of Labor Occupational Safety and Health Administration (OSHA) has developed a four-point approach designed to reduce and prevent illness and injury resulting from musculoskeletal disorders (MSDs) in the workplace. OSHA's four-point approach includes [15]:
Guidelines designed to prevent/reduce workplace MSDs
Enforcement designed to prosecute serious ergonomic violations in the workplace
Outreach and assistance designed to assist businesses with the management of ergonomic issues
A National Advisory Committee on Ergonomics, created to advise OSHA on ergonomic guidelines and identify gaps in research
OSHA's research component may be the most important point in its approach to carpal tunnel syndrome, as none of the prevention strategies studied to date have conclusively demonstrated that they prevent carpal tunnel syndrome [9,106]. Despite this, there are a multitude of recommendations that apply to many types of workers and work environments [17,20]:
Take multiple "microbreaks" (about three minutes each) from work throughout the work day that include stretches (e.g., wrist, fingers, hand, forearm, shoulders, neck) and breathing exercises. These are good times to incorporate exercises aimed at reducing eye fatigue.
Maintain a good posture relative to the type of work being performed. For computer workers, this means sitting with the spine against the back of the chair with the shoulders relaxed, neck flexible, and head upright, with the work at eye level.
For computer users and other types of workers, wrist position is critical. Wrists should not remain flexed, greatly extended, or deviate from side to side for prolonged periods of time.
Workspaces and furniture should be designed to be comfortable for the worker. Specially designed chairs and desks can promote correct posture and potentially save money by decreasing healthcare expenditures and worker absences.
The grip and force used on tools, implements, and controls (including pencils and keyboards) should be as light as possible.
Hands should be kept warm or should be warmed before beginning work. If the work environment will remain cold, gloves should be worn to keep the hands and wrists at a reasonably comfortable temperature.
There are many examples of specific exercises to help prevent carpal tunnel. One example of wrist exercise instructs the individual to hold the second and third fingers up while the others remain closed; draw five clockwise circles in the air with the two fingertips; draw five more counterclockwise circles; and then repeat with the other hand [17].
As a result of the evolving racial and immigration demographics in the United States, interaction with patients for whom English is not a native language is inevitable. Because patient history is such a vital aspect of the assessment of carpal tunnel syndrome, it is each practitioner's responsibility to ensure that information and instructions are explained in such a way that allows for patient understanding. When there is an obvious disconnect in the communication process between the practitioner and patient due to the patient's lack of proficiency in the English language, an interpreter is required.
In this multicultural landscape, interpreters are a valuable resource to help bridge the communication and cultural gap between clients/patients and practitioners. Interpreters are more than passive agents who translate and transmit information back and forth from party to party. When they are enlisted and treated as part of the interdisciplinary clinical team, they serve as cultural brokers, who ultimately enhance the clinical encounter. In any case in which information regarding diagnostic procedures, treatment options and medication/treatment measures are being provided, the use of an interpreter should be considered.
Patient A is a woman, 54 years of age, who has been employed for 17 years in the manufacturing industry. She has missed little work and continues to perform her regular duties, which include spending many hours each day at an assembly station. Patient A also spends time each day at her home computer. The patient presents to her physician's office with chronic pain, tingling, and numbness in her right hand and wrist as well as pain, tingling, and numbness in her neck and shoulders. Patient A indicates that she is unable to take anti-inflammatory medication due to a peptic ulcer and that she has had no success alleviating symptoms with other medications. She also reports a history of hypertension and recent-onset arthritis.
Comments and rationale : Patient A's gender, age, medical history, and symptoms are positive risk factors for carpal tunnel syndrome. A physical examination including laboratory tests and imaging should be conducted to confirm the medical history of hypertension and rheumatoid arthritis.
Phalen's maneuver is performed and reveals significant weakness in Patient A's right hand. Ultrasound and a two-part EDX study are ordered, which confirm the initial diagnosis of carpal tunnel syndrome. A single cortisone injection at the right wrist is recommended while the patient considers further treatment options. The injection provides Patient A with temporary symptom relief (for four weeks). The patient then elects to undergo outpatient endoscopic carpal tunnel release. Postoperative instructions include no computer or other repetitive hand use for a minimum of four weeks. The patient demonstrates significant symptom improvement three weeks postoperatively and reports being pain-free six weeks postoperatively. Patient A relates that she is able to cook and play tennis with no related pain. A follow-up examination at one year shows no recurrence of symptoms.
Carpal tunnel syndrome is possibly the most common nerve disorder diagnosed today. Determining the causes of carpal tunnel syndrome remains an area of ongoing research and may be a synergy between genetics, co-existing health conditions, and personal lifestyle factors. Researchers continue to study the clinical course of carpal tunnel syndrome. By identifying the biomechanical factors related to pain, researchers hope to better understand, treat, and prevent carpal tunnel syndrome and to find new ways to limit or prevent its occurrence.
1. American College of Rheumatology. Carpal Tunnel Syndrome. Available at https://www.rheumatology.org/I-Am-A/Patient-Caregiver/Diseases-Conditions/Carpal-Tunnel-Syndrome. Last accessed June 20, 2024.
2. Stecco C, Aldegheri R. Historical review of carpal tunnel syndrome. Chir Organi Mov. 2008;92(1):7-10.
3. van Rijn RM, Huisstede BM, Koes BW, Burdorf A. Associations between work-related factors and the carpal tunnel syndrome—a systematic review. Scand J Work Environ Health. 2009;35(1):19-36.
4. Hendriks SH, van Dijk PR, Groenier KH, Houpt P, Bilo HJ, Kleefstra N. Type 2 diabetes seems not to be a risk factor for the carpal tunnel syndrome: a case control study. BMC Musculoskelet Disord. 2014;15:346.
5. Shiri R. Hypothyroidism and carpal tunnel syndrome: a meta-analysis. Muscle Nerve. 2014;50(6):879-883.
6. 6. Pastare D, Therimadasamy AK, Lee E, Wilder-Smith EP. Sonography versus nerve conduction studies in patients referred with a clinical diagnosis of carpal tunnel syndrome. J Clin Ultrasound. 2009;37(7):389-393.
7. Basiri K, Katirji B. Practical approach to electrodiagnosis of the carpal tunnel syndrome: a review. Advanced Biomedical Research. 2015;4:50.
8. Lee KH, Lee CH, Lee BG, Park JS, Choi WS. The incidence of carpal tunnel syndrome in patients with rheumatoid arthritis. Int J Rheum Dis. 2015;18(1):52-57.
9. National Institute of Neurological Disorders and Stroke. Carpal Tunnel Syndrome Fact Sheet. Available at https://www.ninds.nih.gov/sites/default/files/migrate-documents/carpal_tunnel_syndrome_e_march_2020_508c_0.pdf. Last accessed June 20, 2024.
10. Shiri R, Falah-Hassani K. Computer use and carpal tunnel syndrome: a meta-analysis. J Neurol Sci. 2015;349(1-2):15-19.
11. Derebery J. Work-related carpal tunnel syndrome: the facts and the myths. Clin Occup Environ Med. 2006;5(2):353-367.
12. U.S. Department of Labor, Bureau of Labor Statistics. Economic News Release: Nonfatal Occupational Injuries and Illnesses Requiring Days Away from Work, 2010. Available at https://www.bls.gov/news.release/archives/osh2_11092011.pdf. Last accessed June 20, 2024.
13. U.S. Department of Labor, Bureau of Labor Statistics. Nonfatal Occupational Injuries and Illnesses Requiring Days Away from Work, 2015. Available at https://www.bls.gov/news.release/pdf/osh2.pdf. Last accessed June 20, 2024.
14. Foley M, Silverstein B, Polissar N. The economic burden of carpal tunnel syndrome: long-term earnings of CTS claimants in Washington State. Am J Ind Med. 2007;50(3):155-172.
15. U.S. Department of Labor Occupational Safety and Health Administration. Ergonomics. Available at https://www.osha.gov/ergonomics/control-hazards. Last accessed June 20, 2024.
17. Mount Sinai Medical Center. Carpal Tunnel Syndrome. Available at https://https://www.mountsinai.org/health-library/diseases-conditions/carpal-tunnel-syndrome. Last accessed June 20, 2024.
18. Ratzlaff CR, Gillies JH, Koehoorn MW. Work-related repetitive strain injury and leisure-time physical activity. Arthritis Rheum. 2007;57(3):495-500.
19. American Academy of Family Physicians. Carpal Tunnel Syndrome: What is Carpal Tunnel Syndrome? Available at https://familydoctor.org/condition/carpal-tunnel-syndrome/. Last accessed June 20, 2024.
20. Mayo Clinic. Carpal Tunnel Syndrome. Available at https://www.mayoclinic.org/diseases-conditions/carpal-tunnel-syndrome/symptoms-causes/syc-20355603. Last accessed June 20, 2024.
21. Weber RA, Boyer KM. Consecutive versus simultaneous bilateral carpal tunnel release. Ann Plast Surg. 2005;54(1):15-19.
22. Tiric-Campara M, Krupic F, Biscevic M, et al. Occupational overuse syndrome (technological diseases): carpal tunnel syndrome, a mouse shoulder, cervical pain syndrome. Acta Inform Med. 2014;22(5):333-340.
23. Mallette P, Zhao M, Zurakowski D, Ring D. Muscle atrophy at diagnosis of carpal and cubital tunnel syndrome. J Hand Surg Am. 2007;32(6):855-858.
24. Keir PJ, Bach JM, Hudes M, Rempel DM. Guidelines for wrist posture based on carpal tunnel pressure thresholds. Hum Factors. 2007;49(1):88-99.
25. Giersiepen K, Spallek M. Carpal tunnel syndrome as an occupational disease. Dtsch Arztebl Int. 2011;108(14):238-242.
26. Ghasemi M, Rezaee M, Chavoshi F, Mojtahed M, Shams Koushki E. Carpal tunnel syndrome: the role of occupational factors among 906 workers. Trauma Mon. 2012;17(2):296-300.
27. Occhionero V, Korpinen L, Gobba F. Upper limb musculoskeletal disorders in healthcare personnel. Ergonomics. 2014;57(8):1166-1191.
28. Vashishtha M, Varghese B, Mosley F, Kadakia A, de Jager W. Screening for thyroid dysfunction and diabetes in patients with carpal tunnel syndrome. Surgeon. 2016;14(3):147-149.
29. Gimeno D, Amick BC III, Habeck RV, Ossmann J, Katz JN. The role of job strain on return to work after carpal tunnel surgery. Occup Environ Med. 2005;62(11):778-785.
31. Lozano-Calderón NS, Anthony S, Ring D. The quality and strength of evidence for etiology: example of carpal tunnel syndrome. J Hand Surg AM. 2008;33(4):525-538.
32. Ettema AM, Amadio PC, Zhao C, et al. Changes in the functional structure of the tenosynovium in idiopathic carpal tunnel syndrome: a scanning electron microscope study. Plast Reconstr Surg. 2006;118(6):1413-1422.
33. van Doesburg MHM, van der Molen AB, Henderson J, Cha SS, An KN, Amadio PC. Subsynovial connective tissue thickness in patients with carpal tunnel syndrome. JUM. 2012;31(1):31-36.
34. Ettema AM, Amadio PC, Zhao C, Wold LE, An KN. A histological and immunohistochemical study of the subsynovial connective tissue in idiopathic carpal tunnel syndrome. J Bone Joint Surg Am. 2004;86-A(7):1458-1466.
36. Ettema AM, An KN, Zhao C, O'Byrne MM, Amadio PC. Flexor tendon and synovial gliding during simultaneous and single digit flexion in idiopathic carpal tunnel syndrome. J Biomech. 2008;41(2):292-298.
37. Osamura N, Zhao C, Zobitz ME, An KN, Amadio PC. Evaluation of the material properties of the subsynovial connective tissue in carpal tunnel syndrome. Clin Biomech. 2007;22(9):999-1003.
38. Kim HS. Carpal tunnel syndrome caused by tophaceous gout. Korean J Intern Med. 2014;29(4):544-545.
39. Balci K, Utku U. Carpal tunnel syndrome and metabolic syndrome. Acta Neurol Scand. 2007;116(2):113-117.
41. Singh R, Gamble G, Cundy T. Lifetime risk of symptomatic carpal tunnel syndrome in type 1 diabetes. Diabet Med. 2005;22(5):625-630.
42. Hobby JL, Venkatesh R, Motkur P. The effect of age and gender upon symptoms and surgical outcomes in carpal tunnel syndrome. J Hand Surg Br. 2005;30(6):599-604.
43. Schmelzer RE, Della Rocca GJ, Caplin DA. Endoscopic carpal tunnel release: a review of 753 cases in 486 patients. Plast Reconstr Surg. 2006;117(1):177-185.
44. Bland JD. The relationship of obesity, age, and carpal tunnel syndrome: more complex than was thought? Muscle Nerv. 2005;32(4):527-532.
45. American Society for Surgery of the Hand. Carpal Tunnel Syndrome. Available at https://www.assh.org/handcare/condition/carpal-tunnel-syndrome. Last accessed June 20, 2024.
46. Eslamian F, Bahrami A, Aghamohammadzadeh N, Niafar M, Salekzamani Y, Behkamrad K. Electrophysiologic changes in patients with untreated primary hypothyroidism. J Clin Neurophysiol. 2011;28(3):323-328.
47. Truijens SE, Meems M, Kuppens SM, et al. The HAPPY study (Holistic Approach to Pregnancy and the first Postpartum Year): design of a large prospective cohort study. BMC Pregnancy Childbirth. 2014;14:312.
48. Taber's Online Medical Dictionary. Available at https://www.tabers.com/tabersonline. Last accessed June 20, 2024.
49. Naeser MA, Hahn KA, Lieberman BE, Branco KF. Carpal tunnel syndrome pain treated with low-level laser and microamperes TENS: a controlled study. Arch Phys Med Rehabil. 2002;83(7):978-988.
50. Gousheh J, Iranpour A. Association between carpal tunnel syndrome and arteriovenous fistula in hemodialysis patients. Plast Reconstr Surg. 2005;116(2):508-513.
51. Gibbons CP. Neurological complications of vascular access. J Vasc Access. 2015;16(Suppl 9):73-77.
52. Namazi H, Majd Z. Carpal tunnel syndrome in patients who are receiving long-term renal hemodialysis. Arch Orthop Trauma Surg. 2007;127(8):725-728.
53. Kopeć J, Gadek A, Drozdz M, et al. Carpal tunnel syndrome in hemodialysis patients as a dialysis-related amyloidosis manifestation: incidence, risk factors and results of surgical treatment. Med Sci Monit. 2011;17(9):CR505-CR509.
54. Makowiec-Dabrowska T, Sinczuk-Walczak H, Józwiak ZW, Krawczyk-Adamus P. Work performance as a risk factor for carpal tunnel syndrome. Med Pr. 2007;58(4):361-372.
55. 55. Hammer HB, Hovden IA, Haavardsholm EA, Kvien TK. Ultrasonography shows increased cross-sectional area of the median nerve in patients with arthritis and carpal tunnel syndrome. Rheumatology (Oxford). 2006;45(5):584-588.
56. Work Loss Data Institute. Carpal Tunnel Syndrome (Acute and Chronic). Encinitas, CA: Work Loss Data Institute; 2011.
57. Ablove RH, Ablove TS. Prevalence of carpal tunnel syndrome in pregnant women. WMJ. 2009;108(4):194-196.
58. Herndon CM, Hutchison RW, Berdine HJ, et al. Management of chronic nonmalignant pain with nonsteroidal anti-inflammatory drugs. Pharmacotherapy. 2008;28(6):788-805.
59. Liu CW, Chen TW, Wang MC, Chen CH, Lee CL, Huang MH. Relationship between carpal tunnel syndrome and wrist angle in computer workers. Kaohsiung J Med Sci. 2003;19(12):617-623.
60. 60. Ly-Pen D, Andréu JL, de Blas G, Sánchez-Olaso A, Millán I. Surgical decompression versus local steroid injection in carpal tunnel syndrome: a one-year, prospective, randomized, open, controlled clinical trial. Arthritis Rheumat. 2005;52(2):612-619.
61. Gell N, Werner RA, Franzblau A, Ulin SS, Armstrong TJ. A longitudinal study of industrial and clerical workers: incidence of carpal tunnel syndrome and assessment of risk factors. J Occup Rehabil. 2005;15(1):47-55.
62. Piazzini DB, Aprile I, Ferrara PE, et al. A systematic review of conservative treatment of carpal tunnel syndrome. Clin Rehabil. 2007;21(4):299-314.
63. O'Connor D, Marshall SC, Massy-Westropp N. Non-surgical treatment (other than steroid injection) for carpal tunnel syndrome. Cochrane Database Syst Rev. 2003;(1):CD003219.
64. Rand Health. 12-Item Short Form Survey (SF-12). Available at https://www.rand.org/health/surveys_tools/mos/12-item-short-form.html. Last accessed June 20, 2024.
65. Dias JJ, Bhowal B, Wildin CJ, Thompson JR. Assessing the outcome of disorders of the hand: is the patient evaluation measure reliable, valid, responsive and without bias? J Bone Joint Surg Br. 2001;83(2):235-240.
66. Chung KC, Pillsbury MS, Walters MR, Hayward RA. Reliability and validity testing of the Michigan Hand Outcomes Questionnaire. J Hand Surg Am. 1998;23(4):575-587.
67. Nathan PA, Istvan JA, Meadows KD. A longitudinal study of predictors of research-defined carpal tunnel syndrome in industrial workers: findings at 17 years. J Hand Surg. 2005;30(6):593-598.
68. Werner RA, Franzblau A, Gell N, Ulin SS, Armstrong TJ. A longitudinal study of industrial and clerical workers: predictors of upper extremity tendonitis. J Occup Rehabil. 2005;15(1):37-46.
69. Goodson JT, DeBerard MS, Wheeler AJ, Colledge AL. Occupational and biopsychosocial risk factors for carpal tunnel syndrome. J Occup Environ Med. 2014;56(9):965-972.
70. Boz C, Ozmenoglu M, Altunayoglu V, Velioglu S, Alioglu Z. Individual risk factors for carpal tunnel syndrome: an evaluation of body mass index, wrist index and hand anthropometric measurements. Clin Neurol Neurosurg. 2004;106(4):294-299.
71. Greenslade JR, Mehta RL, Belward P, Warwick DJ. DASH and Boston Questionnaire assessment of carpal tunnel syndrome outcome: what is the responsiveness of an outcome questionnaire? J Hand Surg. 2004;29(2):159-164.
72. Baysal O, Altay Z, Ozcan C, Ertem K, Yologlu S, Kayhan A. Comparison of three conservative treatment protocols in carpal tunnel syndrome. Int J Clin Pract. 2006;60(7):820-828.
73. Frankenburg FR, Zanarini MC. Obesity and obesity-related illnesses in borderline patients. J Personal Disord. 2006;20(1):71-80.
74. Kurt S, Kisacik B, Kaplan Y, Yildirim B, Etikan I, Karaer H. Obesity and carpal tunnel syndrome: is there a causal relationship? Eur Neurol. 2008;59(5):253-257.
75. Ferry S, Hannaford P, Warskyj M, Lewis M, Croft P. Carpal tunnel syndrome: a nested case-control study of risk factors in women. Am J Epidemiol. 2000;151(6):566-574.
76. Bongers FJM, Schellevis FG, van den Bosch WJHM, van der Zee J. Carpal tunnel syndrome in general practice (1987 and 2001): incidence and the role of occupational and nonoccupational factors. Br J Gen Pract. 2007;57(534):36-39.
77. Kamolz LP, Beck H, Haslik W, et al. Carpal tunnel syndrome: a question of hand and wrist configurations? J Hand Surg Br. 2004;29(4):321-324.
78. Alford JW, Weiss APC, Akelman E. The familial incidence of carpal tunnel syndrome in patients with unilateral and bilateral disease. Am J Orthop. 2004;33(8):397-400.
79. Bodofsky EB, Campellone JV, Wu KD, Greenberg WM. Age and the severity of carpal tunnel syndrome. Electromyogr Clin Neurophysiol. 2004;44(4):195-199.
80. Ashworth NL. Carpal Tunnel Syndrome. Available at https://emedicine.medscape.com/article/327330-overview. Last accessed June 20, 2024.
82. Lee MJ, LaStayo PC. Pronator syndrome and other nerve compressions that mimic carpal tunnel syndrome. J Orthop Sports Phys Ther. 2004;34(10):601-609.
83. MedlinePlus. Cervical Spondylosis. Available at https://medlineplus.gov/ency/article/000436.htm. Last accessed June 20, 2024.
84. Chow CS, Hung LK, Chiu CP, et al. Is symptomatology useful in distinguishing between carpal tunnel syndrome and cervical spondylosis? Hand Surg. 2005;10(1):1-5.
85. American Society for Surgery of the Hand. Cubital Tunnel Syndrome. Available at https://www.assh.org/handcare/condition/cubital-tunnel-syndrome. Last accessed June 20, 2024.
86. Dangers JE. Carpal Tunnel Syndrome in Emergency Medicine. Available at https://emedicine.medscape.com/article/822792-overview. Last accessed June 20, 2024.
87. American Society for Surgery of the Hand. de Quervain's Tendonitis. Available at https://www.assh.org/handcare/condition/dequervains-tenosynovitis. Last accessed June 20, 2024
88. 88. American Society for Surgery of the Hand. Trigger Finger. Available at https://www.assh.org/handcare/condition/trigger-finger. Last accessed June 20, 2024.
89. Erickson M, Lawrence M, Stegink Jansen CW, et al. Hand pain and sensory deficits: carpal tunnel syndrome: clinical practice guidelines linked to the International Classification of Functioning, Disability and Health from the Academy of Hand and Upper Extremity Physical Therapy and the Academy of Orthopaedic Physical Therapy of the American Physical Therapy Association. J Orthop Sports Phys Ther. 2019;49(5):CPG1-CPG85.
90. Washington State Department of Labor and Industries. Work-Related Carpal Tunnel Syndrome Diagnosis and Treatment Guideline. Olympia, WA: Washington State Department of Labor and Industries; 2014.
91. Blumenthal S, Herskovitz S, Verghese J. Carpal tunnel syndrome in older adults. Muscle Nerve. 2006;34(1):78-83.
92. Priganc VW, Henry SM. The relationship among five common carpal tunnel syndrome tests and the severity of carpal tunnel syndrome. J Hand Ther. 2003;16(3):225-236.
93. Edwards A. Phalen's test with carpal compression: testing in diabetics for the diagnosis of carpal tunnel syndrome. Orthopedics. 2002;25(5):519-520.
94. Cheng CJ, Mackinnon-Patterson B, Beck JL, Mackinnon SE. Scratch collapse test for evaluation of carpal and cubital tunnel syndrome. J Hand Surg Arm. 2008;33(9):1518-1524.
95. Douglas R. Scratch collapse test for the evaluation of carpal and cubital tunnel syndrome. J Hand Ther. 2009;22(4):384.
96. Hansen PA, Micklesen P, Robinson LR. Clinical utility of the flick maneuver in diagnosing carpal tunnel syndrome. Am J Phys Med Rehabil. 2004;83(5):363-367.
97. Ma H, Kim I. The diagnostic assessment of hand elevation test in carpal tunnel syndrome. J Korean Neurosurg Soc. 2012;52(5): 472-475.
98. Amirfeyz R, Gozzard C, Leslie IJ. Hand elevation test for assessment of carpal tunnel syndrome. J Hand Surg. 2005;30(4):361-364.
99. Verdugo RJ, Salinas RA, Castillo JL, Cea JG. Surgical versus non-surgical treatment for carpal tunnel syndrome. Cochrane Database Syst Rev. 2008;(4):CD001552.
100. Homan MM, Franzblau A, Werner RA, Albers JW, Armstrong TJ, Bromberg MB. Agreement between symptom surveys, physical examination procedures and electrodiagnostic findings for the carpal tunnel syndrome. Scand J Work Environ Health. 1999;25(2): 115-124.
101. American Academy of Orthopaedic Surgeons. Carpal Tunnel Syndrome. Available at https://orthoinfo.aaos.org/en/diseases--conditions/carpal-tunnel-syndrome. Last accessed June 20, 2024.
102. Clendening J. Minimally invasive carpal tunnel surgery offers quicker healing. Available at https://news.vumc.org/2020/03/19/minimally-invasive-carpal-tunnel-surgery-offers-quicker-healing/. Last accessed June 20, 2024.
103. Mallouhi A, Pülzl P, Trieb T, Piza H, Bodner G. Predictors of carpal tunnel syndrome: accuracy of gray-scale and color Doppler sonography. Am J Roentgenol. 2006;186(5):1240-1245.
104. El Miedany YM, Aty SA, Ashour S. Ultrasonography versus nerve conduction study in patients with carpal tunnel syndrome: substantive or complementary tests? Rheumatology (Oxford). 2004;43(7):887-895.
105. Kaymak B, Ozçakar L, Cetin A, Candan Cetin M, Akinci A, Hasçelik Z. A comparison of the benefits of sonography and electrophysiologic measurements as predictors of symptom severity and functional status in patients with carpal tunnel syndrome. Arch Phys Med Rehabil. 2008;89(4):743-748.
106. American Academy of Orthopaedic Surgeons. Clinical Practice Guideline on the Management of Carpal Tunnel Syndrome. Rosemont, IL: American Academy of Orthopaedic Surgeons; 2024.
107. Hegmann KT. Hand, wrist, and forearm disorders not including carpal tunnel syndrome. In: Hegmann KT (ed). Occupational Medicine Practice Guidelines: Evaluation and Management of Common Health Problems and Functional Recovery in Workers. 3rd ed. Elk Grove Village, IL: American College of Occupational and Environmental Medicine; 2011: 1-188.
108. Blebea JS, Lott KE, Daffner RH, et al. ACR Appropriateness Criteria: Chronic Wrist Pain. Reston, VA: American College of Radiology; 2009.
110. Wong SM, Griffith JF, Hui AC, Lo SK, Fu M, Wong KS. Carpal tunnel syndrome: diagnostic usefulness of sonography. Radiology. 2004;232(1):93-99.
111. Mondelli M, Filippou G, Gallo A, Frediani B. Diagnostic utility of ultrasonography versus nerve conduction studies in mild carpal tunnel syndrome. Arthritis Rheum. 2008;59(3):357-366.
112. Iannicelli E, Almberger M, Chianta GA, et al. High resolution ultrasonography in the diagnosis of carpal tunnel syndrome. Radiol Med (Torino). 2005;110(5-6):623-629.
113. Yesildag A, Kutluhan S, Sengul N, et al. The role of ultrasonographic measurements of the median nerve in the diagnosis of carpal tunnel syndrome. Clin Radiol. 2004;59(10):910-915.
114. Kwon BC, Jung KI, Baek GH. Comparison of sonography and electrodiagnostic testing in the diagnosis of carpal tunnel syndrome. J Hand Surg. 2008;33(1):65-71.
115. Naranjo A, Ojeda S, Mendoza D, Francisco F, Quevedo JC, Erqusquin C. What is the diagnostic value of ultrasonography compared to physical evaluation in patients with idiopathic carpal tunnel syndrome? Clin Exp Rheumatol. 2007;25(6):853-859.
116. Mogk JP, Keir PJ. Evaluation of the carpal tunnel based on 3-D reconstruction from MRI. J Biomech. 2007;40(10):2222-2229.
117. Keir PJ. Magnetic resonance imaging as a research tool for biomechanical studies of the wrist. Semin Musculoskelet Radiol. 2001;5(3):241-250.
118. Jarvik JG, Comstock BA, Heagerty PJ, et al. Magnetic resonance imaging compared with electrodiagnostic studies in patients with suspected carpal tunnel syndrome: predicting symptoms, function, and surgical benefit at 1 year. J Neurosurg. 2008;108(3):541-550.
119. Martins RS, Siqueira MG, Simplicio H, Agapito D, Medeiros M. Magnetic resonance imaging of idiopathic carpal tunnel syndrome: correlation with clinical findings and electrophysiological investigation. Clin Neurol Neurosurg. 2008;110(1):38-45.
120. Wilder-Smith EP, Seet RCS, Lim ECH. Diagnosing carpal tunnel syndrome—clinical criteria and ancillary tests. Nat Clin Pract Neurol. 2006;2(7):366-374.
121. Lee CH, Kim TK, Yoon ES, Dhong ES. Correlation of high-resolution ultrasonographic findings with the clinical symptoms and electrodiagnostic data in carpal tunnel syndrome. Ann Plast Surg. 2005;54(1):20-23.
122. Weber RA, Schuchmann JA, Albers JH, Ortiz J. A prospective blinded evaluation of nerve conduction velocity versus Pressure-Specified Sensory Testing in carpal tunnel syndrome. Ann Plast Surg. 2000;45(3):252-257.
123. Tassler PL, Dellon AL. Correlation of measurements of pressure perception using the pressure-specified sensory device with electrodiagnostic testing. J Occup Environ Med. 1995;37(7):862-866.
124. Scholten RJPM, Mink van der Molen A, Uitdehaag BMJ, Bouter LM, de Vet HCW. Surgical treatment options for carpal tunnel syndrome. Cochrane Database Syst Rev. 2007;(4):CD003905.
125. Marshall SC, Tardif G, Ashworth NL. Local corticosteroid injection for carpal tunnel syndrome. Cochrane Database Syst Rev. 2007;(2):CD001554.
1. American Academy of Orthopaedic Surgeons. Management of Carpal Tunnel Syndrome: Evidence-Based Clinical Practice Guideline. Available at https://www.aaos.org/globalassets/quality-and-practice-resources/carpal-tunnel/carpal-tunnel-2024/cts-cpg.pdf. Last accessed June 26, 2024.
Mention of commercial products does not indicate endorsement.