Advances have provided insightful evidence regarding the role of the trigeminal system, cortical spreading depression, ion-channel pathology, and signaling molecules, such as nitric oxide, adenosine, and calcitonin gene-related peptide (CGRP), in the pathophysiology of migraine. The differential diagnosis between migraine and the most common medical conditions (e.g., cluster and tension headache) has been extensively reviewed. However, the differential diagnosis and management of other cephalalgias relevant to medical and dental practice, such as cranial neuralgias, trigeminal pathology, temporomandibular joint dysfunction, and oral pathologies, are seldom addressed. An approach combining pharmacological and nonpharmacological therapies, including alternative and complementary approaches, will be discussed. This course provides an integrated approach to the clinically relevant advances in the understanding of migraine pathophysiology and novel therapies and focuses on the differential diagnosis between migraine and a group of common, yet often overlooked, medical and dental conditions.
This course is designed for physicians, physician assistants, nurses, nurse practitioners, and other healthcare professionals involved in the care of patients with known or suspected migraine.
The purpose of this course is to provide an update of research elucidating the pathophysiology of migraine, which has resulted in "mechanism-based" therapies; to review the differential diagnosis of headache disorders; and to summarize the current and evidence-based guidelines for clinical management of migraine. The course will highlight the need for a graded therapeutic response based on frequency of attacks and pattern of symptoms, and the importance of patient education and self-management techniques as a means of ensuring compliance and improving outcomes.
Upon completion of this course, you should be able to:
- Discuss the prevalence of migraine in relation to age, gender, and such factors as socioeconomic status, education, and comorbidities.
- Provide an updated overview of the progress made in the understanding of migraine pathophysiology.
- Review the clinical profiles and diagnostic criteria of migraine with or without aura, and summarize disease staging.
- Provide an updated overview of the differential diagnosis of migraines focusing on medical and dental conditions, such as temporomandibular disorders, sinusitis, and orofacial pain.
- Discuss the preventive and acute treatment of migraine.
A. José Lança, MD, PhD, received his Medical Degree at the University of Coimbra in Coimbra, Portugal, and completed his internship at the University Hospital, Coimbra. He received his PhD in Neurosciences from a joint program between the Faculties of Medicine of the University of Coimbra, Portugal, and the University of Toronto, Toronto, Canada. He was a Gulbenkian Foundation Scholar and received a Young Investigator Award by the American Brain & Behavior Research Foundation.
Dr. Lança participated in international courses and conferences on neurosciences. He has contributed to a better understanding of the mechanisms underlying the ontogenetic development of the brain opiatergic system. As a research scientist at the Addiction Research Foundation (ARF) in Toronto, he initiated research on the functional role played by dopaminergic cell transplants on alcohol consumption, leading to the publication of the first research reports on cell transplantation and modulation of an addictive behavior. Subsequently, he also investigated the role played by other neurotransmitter systems in the limbic system and mechanisms of reward, co-expression of classical neurotransmitters and neuropeptides and potential role in neuropsychiatric disorders.
He is an Assistant Professor in the Department of Pharmacology and Toxicology at the Faculty of Medicine and at the Faculty of Dentistry at the University of Toronto, where he lectures and directs several undergraduate and postgraduate pharmacology and clinical pharmacology courses. He was the Program Director for Undergraduate Studies in the Department of Pharmacology and Toxicology of the University of Toronto. He has developed clinical pharmacology courses for the Medical Radiation Sciences and Chiropody Programs of The Michener Institute for Health Sciences at the University of Toronto.
Dr. Lança’s commitment to medical education started while a medical student, teaching in the Department of Histology and Embryology, where he became cross-appointed after graduation. In Toronto, he has contributed extensively to curriculum development and teaching of pharmacology to undergraduate, graduate, and medical students.
He has authored research and continuing education in peer-reviewed publications and is the author of six chapters in pharmacology textbooks. Dr. Lança has conducted research in various areas including neuropharmacology, pharmacology of alcoholism and drug addiction, and herbal medications.
He has developed and taught courses and seminars in continuing medical education and continuing dental education. His commitment to continuing education emphasizes an interdisciplinary approach to clinical pharmacology.
Contributing faculty, A. José Lança, MD, PhD, has disclosed no relevant financial relationship with any product manufacturer or service provider mentioned.
John M. Leonard, MD
Mary Franks, MSN, APRN, FNP-C
Randall L. Allen, PharmD
The division planners have disclosed no relevant financial relationship with any product manufacturer or service provider mentioned.
Sarah Campbell
The Director of Development and Academic Affairs has disclosed no relevant financial relationship with any product manufacturer or service provider mentioned.
The purpose of NetCE is to provide challenging curricula to assist healthcare professionals to raise their levels of expertise while fulfilling their continuing education requirements, thereby improving the quality of healthcare.
Our contributing faculty members have taken care to ensure that the information and recommendations are accurate and compatible with the standards generally accepted at the time of publication. The publisher disclaims any liability, loss or damage incurred as a consequence, directly or indirectly, of the use and application of any of the contents. Participants are cautioned about the potential risk of using limited knowledge when integrating new techniques into practice.
It is the policy of NetCE not to accept commercial support. Furthermore, commercial interests are prohibited from distributing or providing access to this activity to learners.
Supported browsers for Windows include Microsoft Internet Explorer 9.0 and up, Mozilla Firefox 3.0 and up, Opera 9.0 and up, and Google Chrome. Supported browsers for Macintosh include Safari, Mozilla Firefox 3.0 and up, Opera 9.0 and up, and Google Chrome. Other operating systems and browsers that include complete implementations of ECMAScript edition 3 and CSS 2.0 may work, but are not supported. Supported browsers must utilize the TLS encryption protocol v1.1 or v1.2 in order to connect to pages that require a secured HTTPS connection. TLS v1.0 is not supported.
The role of implicit biases on healthcare outcomes has become a concern, as there is some evidence that implicit biases contribute to health disparities, professionals' attitudes toward and interactions with patients, quality of care, diagnoses, and treatment decisions. This may produce differences in help-seeking, diagnoses, and ultimately treatments and interventions. Implicit biases may also unwittingly produce professional behaviors, attitudes, and interactions that reduce patients' trust and comfort with their provider, leading to earlier termination of visits and/or reduced adherence and follow-up. Disadvantaged groups are marginalized in the healthcare system and vulnerable on multiple levels; health professionals' implicit biases can further exacerbate these existing disadvantages.
Interventions or strategies designed to reduce implicit bias may be categorized as change-based or control-based. Change-based interventions focus on reducing or changing cognitive associations underlying implicit biases. These interventions might include challenging stereotypes. Conversely, control-based interventions involve reducing the effects of the implicit bias on the individual's behaviors. These strategies include increasing awareness of biased thoughts and responses. The two types of interventions are not mutually exclusive and may be used synergistically.
#90073: Migraine: Diagnosis and Therapeutic Advances
Migraine is the leading condition of recurrent cephalalgias of moderate or severe intensity. It is the most common type of headache in patients who seek medical treatment. According to the 2021 Global Burden of Disease study, migraine was responsible for 43.4 million years of healthy life lost due to disability, or 4.7% of total years lost to disability in 2021. Migraine headache comprises 88.3% of the total burden of headache disorders[1]. Migraine is among the top five most disabling medical conditions worldwide and the burden is greatest in women between 15 and 45 years of age [2].
Migraine has been identified as one of the most common neurologic disorders, and in the United States, its prevalence in the general population is approximately 15% [3]. In children, the prevalence ranges from 1% to 4% and does not present a gender bias. However, after menarche, its prevalence in women (20.5%) is more than two times greater than the prevalence in men [4,5].
Medical advances have provided insightful evidence regarding the role of the trigeminal system, cortical spreading depression, ion-channel pathology, and signaling molecules (such as nitric oxide, adenosine, and calcitonin gene-related peptide [CGRP]) in the pathophysiology of migraine. Together, they have led to the "mechanism-based" development of new drugs that show promising clinical efficacy coupled with a lower occurrence of adverse effects. The improved risk/benefit profile of a newer generation of antimigraine medications will be discussed in this course.
The differential diagnosis and management of other cephalalgias relevant to medical and dental practice, such as cranial neuralgias, trigeminal pathology, temporomandibular joint dysfunction, and oral pathologies, are seldom addressed in discussions of migraine. However, this course will extensively review the differential diagnosis between migraine and the most common medical conditions with similar presentation (e.g., cluster and tension headache).
Cephalalgias have a lifetime prevalence of more than 90% and an estimated prevalence of 50% in the adult population worldwide [4,5]. Primary headaches are the sixth most common cause for patients to seek emergency care in the United States [6]. Secondary headaches, although less frequent, have well-defined etiologies, including infections (e.g., sinusitis, meningitis), cerebrovascular disorders (e.g., ischemia, thrombus, hemorrhage), or neoplasias, and are diagnosed based on history, examination, laboratory tests, and imaging studies (e.g., computed tomography [CT] scan, magnetic resonance imaging [MRI]) [7,8].
According to the International Classification of Headache Disorders, published by the International Headache Society, there are four main types of primary headaches: migraine, tension-type headache, cluster headache/trigeminal autonomic cephalalgias (TACs), and a group that includes other primary headache disorders [7,9]. Tension-type headache is the most common, with a prevalence of 30% to 78% [4,7,9,10]. Typically, tension-type headache is bilateral with mild-to-moderate intensity and non-pulsating quality. It is neither associated with nausea nor aggravated by routine physical activity [7,9,10].
Cluster headache/TACs are severe and uncommon headaches with a prevalence of 0.07% to 0.4% and occur more commonly in men than in women [11]. These headaches are intermittent, short-lasting, and excruciatingly painful unilateral headaches. The quality of the pain is sharp or stabbing but not pulsating, which typically differentiates them from migraines. The pain peaks within 10 to 15 minutes and persists for an average of one to three hours. During cluster headache, patients do not seek rest (quite unlike during migraine headache), but are noticeably agitated and restless and present with parasympathetic autonomic dysfunction (e.g., conjunctival injection, lacrimation) [7,9,10].
The miscellaneous group of primary headaches is made up of a variety of conditions, including thunderclap headache and exertional headache [7]. These conditions can mimic potentially serious secondary headaches and require thorough clinical evaluation supported by appropriate laboratory tests and imaging procedures. Thunderclap headache occurs suddenly, reaches maximum intensity within one minute, and lasts 1 to 24 hours or even several days. Typically, patients describe the pain of a thunderclap headache as an "explosion in the head" or "being hit with a bat" [12]. Thunderclap headache mimics the pain of a ruptured cerebral aneurysm [7]. Considering that up to 25% of patients with thunderclap headache have subarachnoid hemorrhage (SAH) and that the mortality rate from SAH is approximately 50%, these patients require emergency evaluation, including detailed physical examination and CT scan. Imaging tests are used in the differential diagnosis with other potentially life-threatening conditions, such as intracerebral hemorrhage, cerebral venous thrombosis, hypertensive emergency, and ischemic stroke, in addition to SAH. Lumbar puncture is recommended in patients with thunderclap headache and non-diagnostic CT scan. The risk/benefit of CT or MRI angiography should be taken into account in patients with normal brain CT and cerebrospinal fluid (CSF) analysis, considering that the risk of SAH and death is extremely low in this group [13,14]. Clinically, it is recommended that the diagnosis of thunderclap headache should apply only when no specific etiology is identified despite comprehensive diagnostic evaluation [9,12,13].
Exertional headache is triggered by physical exercise and is a pulsating headache that lasts from minutes to two days. These patients require comprehensive neurologic evaluation and imaging studies to help eliminate possible underlying secondary causes, including SAH and arterial dissection [7,9,10,15].
As noted, migraine is the leading condition of recurrent cephalalgias of moderate-to-severe intensity. Pain usually builds up over a 1- to 2-hour period and lasts 4 to 72 hours. These headaches present at least two of the following characteristics:
Typically pulsating or throbbing
Unilateral and localized in the frontotemporal and ocular area, although the pain may be felt anywhere in the head or neck
Aggravated by routine activity
In addition, migraine is usually accompanied by photophobia and/or phonophobia and nausea and/or vomiting [7,9,10].
In Western countries, including the United States, migraine has been identified as one of the most common neurologic disorders. The age-adjusted prevalence of migraine and severe headache in the United States has remained stable for more than two decades. According to a 2020 review of national health surveillance data, the prevalence of migraine is 15.9% in adults, and highest among those 18 to 44 years of age (18.7%) [16]. The biologic sex ratio is also stable, with 21% of women and 10.7% of men affected. The prevalence of migraine is highest in American Indian/Alaska Natives (22.1%) compared with White, Black, or Hispanic Americans (15.6% to 16.3%), and lowest in Asians (9.1%). In childhood, migraine is less common (1% to 4%) and equally prevalent among boys and girls [17,18]. The prevalence increases in adolescence (12%), affecting prepubertal boys and postmenarche girls [19]. The lifetime prevalence of migraine increases from age 12 to 40 years then declines thereafter in both sexes [20].
The individual, familial, and social impact of migraine is significant. In the United States, approximately 23% of households have at least one member who suffers from migraine [2,20]. More than half of migraineurs report that severe headaches cause substantial impairment in daily activities and require bed rest, while one-third of migraine sufferers missed at least one day of work or school in the previous three months because of migraine and work or school productivity was reduced by at least 50% [20]. An estimated 4 million emergency department visits each year are for migraine/severe headache, and among female patients 15 to 64 years of age, migraine is the third most common reason for emergency department visits [16].
The burden of migraine falls disproportionately on persons of lower socioeconomic status. Among respondents with migraine who participated in governmental surveys conducted between 2009 and 2018, 38% were unemployed, 42% subsisted at or near the poverty level, 34% had received a high school education or below, and 18% were uninsured [16]. Socioeconomic factors could influence prevalence and burden of migraine by exerting a negative impact on incidence and severity, nutritional status, and access to care and effective therapies.
Migraine accounts for nearly 4.7% of years lived with disability, and the Global Burden of Disease study has ranked it among the top four most disabling medical conditions [2,20,21,22,23]. Specifically, chronic migraine represents close to 50% of all cases of chronic headache and has a lifetime prevalence of 1% to 2%. The incidence is higher in women, those of two or more races, and those who are obese and/or have a diagnosis of diabetes [3,24,25]. Longitudinal studies of chronic migraine show the devastating effects of the condition, with most patients in the United States reporting increased disability after a two-year follow-up [26,27].
The International Classification of Headache Disorders categorizes migraines as acute or chronic [7,9]. Acute or episodic migraine with aura is characterized by "transient focal neurologic symptoms that usually precede or sometimes accompany the headache" [9]. Some patients have premonitory symptoms occurring hours or days before the headache as well as a headache resolution phase. Premonitory and resolution symptoms include hyperactivity, hypoactivity, depression, cravings for particular foods, repetitive yawning, fatigue, and neck stiffness and/or pain [9]. Twenty-five percent of patients with migraine with aura experience visual disturbances, including flashing lights (i.e., phosphenes), hemianopsia, and scotomas, that precede the onset of the cephalalgia and last no longer than 60 minutes [10]. In 30% of patients with migraine with aura, sensory symptoms, such as perioral numbness or tingling, are present. Although less common, hemiparesis, speech and/or language impairment (e.g., dysarthrias), and/or brainstem symptoms (e.g., vertigo, ataxia) may also occur [9,10].
Acute migraine without aura is defined as a recurrent headache disorder manifesting in attacks lasting 4 to 72 hours with unilateral location, pulsating quality, moderate or severe intensity, aggravation with routine physical activity, and association with nausea and/or photophobia and phonophobia, in the absence of aura. Migraine without aura is seen in less than 10% of women during their menstrual cycle, but tends to last longer and be accompanied by more severe nausea than cases occurring outside of menstruation [7,9].
The criteria of chronic migraine were updated and included in the revised ICHD-2R, and later confirmed in the ICHD-3 [9,28]. Chronic migraine is defined as a tension-type headache and/or migraine headache occurring 15 or more days per month for more than three months and having the features of migraine headache on at least eight days per month [9,28]. Pain medication overuse is the most common reversible cause of headaches resembling chronic migraine [9,29]. Previously, the ICHD-2R criteria noted that the diagnosis of chronic migraine should not apply to patients with medication overuse; however, the updated ICHD-3 includes medication overuse as the most common cause of symptoms suggestive of chronic migraine and indicates that chronic migraine often reverts to an episodic migraine after drug withdrawal in approximately 50% of patients [9].
Traditionally, migraine was classified as a typical neurovascular disorder with unilateral extracranial vasodilation of the frontal branch of the superficial temporal artery ipsilateral to the headache [30]. The vasogenic theory is consistent with the headache-inducing properties of vasodilating drugs (e.g., nitroglycerine) and the therapeutic properties of vasoconstrictors (e.g., ergotamine). This localized vasodilation was considered to be the rebound of an initial vasoconstriction and transient hypovascularization in discrete brain regions. However, a number of imaging studies have revealed a discrepancy between the temporal profile of vascular dysregulation and migraine pain. This discrepancy is further supported by the fact that vasodilating neuropeptides, such as vasoactive intestinal peptide, do not induce migraine pain [31,32].
Alternatively, the neurogenic theory views migraine as the combination of neuronal hyperactivity with a local process of neurogenic inflammation triggered by an increase in pro-inflammatory mediators such as CGRP, neurokinin, and substance P [31,33]. In addition, low levels of the endogenous opioid enkephalin found during migraine correlate to a decrease in pain threshold and are responsible for the reported regional allodynia of the head and upper trunk [34,35].
The diversity of clinical manifestations observed by patients with migraine is an indication no single theoretical model is likely to account for the complex pathophysiology of the disease. Rather, migraine is the product of multiple mechanisms affecting broad areas of the central nervous system. Over the past decade, research findings have provided insightful evidence regarding the role of cortical spreading depression, trigeminal nerve activity, signaling molecules (e.g., serotonin, CGRP, nitric oxide), and genetic alteration of ion channels and transporters in the pathophysiology of the disease [31,34,36,37]. It is now known that the pathogenesis of migraine involves the trigeminal nerve and its axonal projections to the intracranial vasculature (the trigeminovascular system) [38]. Neuronal afferent fibers innervate the meninges and its vessels and also project to areas within the brain. Activation of the trigeminovascular system, which releases vasoactive substances and inflammatory mediators, is followed by further sensitization and then relay of nociceptive signals to cortical areas that subserve perception of pain [38]. Progress in understanding these components of pathogenesis has enabled development of mechanism-based, targeted therapies with increased clinical efficacy and fewer adverse effects [39].
Cortical spreading depression is an intense wave of neuronal and glial excitation (i.e., depolarization) progressing in the cerebral cortex at a rate of 2–3 mm per minute. This wave of depolarization is followed by transient suppression of spontaneous neuronal activity (hyperpolarization) and changes in vascular diameter and blood flow caused partly by introduction of inflammatory molecules and CGRP to the dura [38,40]. Clinically, the net effect is an aura followed by migraine headache. Cortical spreading depression is the neurophysiologic event typically associated with migraine with aura and the activation of N-methyl-D-aspartate (NMDA) glutamate receptors. The direct intercellular transfer of ions via gap junctions and the release of inflammatory mediators are required for cortical spreading depression to occur [34,41,42]. However, the precise role of cortical spreading depression in migraine without aura remains elusive and somewhat controversial. Among the arguments against cortical spreading depression in migraine is that it is difficult to evoke in humans and that EEG readings are not flattened during migraine (as opposed to EEG during cortical spreading depression). Migraine can occur bilaterally, in contrast to cortical spreading depression, and is not accompanied by a disrupted blood-brain barrier, increased cerebral metabolism, or cerebral swelling. Additionally, cortical spreading depression does not explain the appearance of premonitory symptoms or allodynia, long before the actual onset of aura [43]. Animal models have shown that induction of cortical spreading depression causes meningeal vasodilation, a mechanism that requires participation of the trigeminal nerve [44,45]. The clinical relevance of cortical spreading depression in migraine has also been supported by imaging techniques, namely positron emission tomography (PET) and functional magnetic resonance imaging (fMRI) [46,47,48,49].
The trigeminal nerve (V) is a mixed cranial nerve that originates in the trigeminal nucleus located in the brain stem. Together with the trigeminal ganglion, motor output, and sensory input, it is known as the trigeminocervical complex. Its motor fibers innervate the masticatory muscles, whereas its three sensory branches—ophthalmic (V1), maxillary (V2), and mandibular (V3)—play a key role in the nociceptive perception of the front of the face, head, dura mater, regional meningeal vasculature, cheek, cornea, lower face, jaw, and anterior two-thirds of the tongue. The ophthalmic branch (V1) plays a key role in the nociception of orofacial pain, cephalalgias, and neurovascular pathology of migraine [34,50,51]. Sensory stimuli originating in the dural vessels activate the nociceptive trigeminal fibers, which initiate the ascending pathway to the brainstem, hypothalamus, thalamus, and finally the cerebral cortex [36,52].
It should be noted that the innervation of adjacent areas by trigeminal branches (i.e., V1/V2 and V2/V3) presents a certain degree of overlap and accounts for the occasional lack of definition of precise localization of pain that makes the differential diagnosis between sinusitis, odontalgia, and migraine challenging in some patients [53,54,55,56,57]. Guidelines for clinical evaluation and differential diagnosis will be discussed later in this course.
Signaling molecules are the neurochemical messengers used by neurons and glial cells to transfer information among each other [58]. Glial cells play a role beyond myelination and extracellular ionic homeostasis, as they also release proinflammatory mediators that regulate neuronal activity, vascular tone, and intercellular concentrations of ions [42,58,59].
Gap junctions between glial cells and neurons regulate ion transfer and neuronal depolarization in cortical spreading depression. Conflicting results of clinical trials have been noted with regard to using a gap junction blocker (e.g., tonabersat) for migraine prophylaxis. In one trial, tonabersat was shown to be effective, while another showed efficacy only in migraine without aura; another trial showed no proven efficacy [60]. Additional research and clinical studies are required to determine the efficacy of gap junction blockers for the treatment of migraine [60,61,62].
Voltage-gated calcium and sodium channels regulate neuronal excitability and intracellular signaling pathways [58]. Mutations in the genes encoding for these channels cause them to malfunction, leading to a variety of conditions known as channelopathies. Augmented channel function and neuronal hyperexcitability is associated with clinical conditions such as epilepsy and migraine, whereas decreased function is associated with hypoexcitability and paralysis [63,64,65]. Accordingly, channel blockers such as valproate and topiramate used in the management of epilepsy are also effective in migraine prevention [39,65,66].
Additional mechanisms, including an increase in synthesis and release of signaling molecules such as neurotransmitters (e.g., serotonin), neuropeptides (e.g., CGRP), vasodilators (e.g., nitric oxide), and pro-inflammatory mediators (e.g., histamine), play a key role in the pathogenesis of migraine. The association between serotonin (5-hydroxytryptamine or 5-HT) and vascular changes is well-established. Increases in synthesis and concentrations of 5-HT in the brain, as well as elevated urinary levels of the 5-HT metabolite 5-hydroxyindolacetic acid (5-HIAA), are observed during migraine attacks [39,67,68]. The multiple vascular effects of 5-HT observed in different organs depend on the subtype of the receptors involved. The effectiveness of ergotamine and its derivatives in the treatment of acute migraine results from their vasoconstrictive properties, which are mediated by their binding to the 5-HT1 receptors abundant in meningeal blood vessels [69,70]. These drugs are agonists at the 5-HT1 autoreceptors and inhibit presynaptic release of serotonin, causing vasoconstriction. Triptans are selective agonists at the 5-HT1B/1D receptor subtypes. This action triggers vasoconstriction of the cranial circulation, making these medications highly effective in the treatment of acute migraine and further supporting the role of the serotonergic system, and the 5-HT1B/1D receptor in particular, in migraine pathophysiology [39,67,68]. 5-HT1B/1D receptors are also present in high levels in cardiac vessels, thus explaining the potential for adverse cardiac effects (e.g., vasoconstriction of the coronary arteries) with ergotamine derivatives and triptans [69,70]. Although the therapeutic properties of triptans will be discussed in detail later in this course, it is relevant to point out that they result from the combination of three different mechanisms of action: vasoconstriction of meningeal vessels by direct effect on vascular smooth cells; inhibition of the release of vasoactive and proinflammatory peptides by trigeminal neurons; and inhibition of nociceptive transmission in the brainstem [69,71].
High levels of the excitatory neurotransmitter glutamate are present in the CSF of patients with migraine, and genetic studies support a crucial role played by a hyperactive glutamatergic system in migraine [72]. Furthermore, antagonists of the glutamate NMDA receptor (e.g., memantine) are effective in the prevention of migraine [63,64].
The role of dopamine in the pathophysiology of migraine is supported by two main points: the role of the dopaminergic system in nausea, vomiting, and blood pressure changes that occur during a migraine attack, and the therapeutic effectiveness of dopamine antagonists (e.g., metoclopramide, prochlorperazine, chlorpromazine) in the treatment of migraine [73,74]. However, these are not antimigraine drugs of choice, and their clinical use remains limited to the management of nausea and vomiting. They are parenterally administered in emergency settings in addition to triptans [51,75].
The activation of nociceptive fibers of the trigeminal ophthalmic (V1) and maxillary (V2) branches elicits the release of neuropeptides such as CGRP and substance P [31,40,76,77]. These peptides trigger mast cell degranulation and the release of histamine and nitric oxide, thus promoting meningeal vasodilation and plasma extravasation. Direct stimulation of the trigeminal ganglion activates the ascending nociceptive pathway, leading to sensitization and decreased pain threshold [31,34,37,40,76,78].
CGRP is a potent vasodilatory neuropeptide that increases blood flow in the meningeal arteries [77]. The fundamental role played by CGRP in migraine is supported by four main lines of evidence. First, CGRP blood levels are elevated during acute migraine pain. Second, infusion of CGRP in patients with migraine causes a migraine-like headache. Third, selective CGRP antagonists lower CGRP levels and are effective in the acute treatment of migraine. And finally, in a double-blind clinical trial a CGRP antagonist (telcagepant) had the same efficacy in migraine resolution as a 5-HT1B/1D agonist (zolmitriptan) [77,79,80]. After success in several clinical trials, three novel CGRP antagonists were approved by the FDA in 2018 for migraine prophylaxis [81,82,83,84]. Two additional CGRP antagonists received approval for an expanded indication for migraine prophylaxis in 2021 and 2023 [85,86,87].
The association between nitric oxide and migraine is supported by animal studies and clinical evidence that administration of nitric oxide donors (e.g., sodium nitroprusside, nitroglycerine) triggers headaches in patients with migraine, whereas nitric oxide synthase inhibitors reverse the condition and are effective in treating acute migraine [88]. However, non-selective nitric oxide synthase inhibitors cause hypertension and potentially other serious adverse effects, such as coronary vasoconstriction, precluding their clinical usefulness. Research is being actively conducted to develop nitric oxide synthase inhibitors selective to the regional vessels implicated in migraine [70,88,89].
Histamine mediates neuroinflammation, causes vasodilation, and triggers headaches with characteristics similar to the ones observed with nitric oxide increases. These effects are reversed by administration of antihistamines that block the H1 receptor (e.g., diphenhydramine, fexofenadine) [70].
In women, low levels of estrogen are correlated with an increase in migraine attacks in the perimenstrual and perimenopausal stages; high estrogen levels and pregnancy are associated with a reduction in the occurrence of migraine attacks [90]. However, the relationship between estrogen levels and migraine is complex and much debated. Research and updated CDC reports indicate that oral contraceptives may be used by women with migraine without aura, but the cardiovascular risks outweigh the benefits of oral contraceptives for women with migraine with aura [91,92]. Considering the increased risk of cardiovascular diseases in women with migraine (particularly migraine with aura) and the increased risk of stroke in women who take combination oral contraceptives, the risk should be carefully evaluated before oral contraceptives or hormone replacement are considered [93,94,95].
Genetic mutations that encode ion channels and pumps have been identified as the cause of familial hemiplegic migraine (FHM), a rare cause of migraine with aura, suggesting that disturbances in ion homeostasis in the brain are responsible for this migraine type [96]. FHM is the first migraine syndrome to be linked to a specific genetic polymorphism in specific loci in chromosomes 1 and 19 that encode for voltage-gated calcium and sodium/potassium channels. Mutations in calcium channels have been identified in FHM type 1 and mutations in the sodium/potassium channels in FHM type 2 [63,65,97]. These findings provide the mechanistic explanation for the therapeutic efficacy of channel blockers such as valproate and topiramate in the prevention of migraine [51,66,98].
Although the role played by genetic mutations in non-familial forms of migraine is unclear, half of patients with migraine have a first-degree relative also suffering from migraine, and in monozygotic twins, there is 50% heritability with a multifactorial basis [99,100,101]. Genetic variants related to the excitatory neurotransmitter glutamate and its receptors have also been identified in non-familial migraine [72]. This evidence further supports the therapeutic value of memantine—a glutamate NMDA receptor antagonist—in the treatment of migraine [102,103].
The dopaminergic system has also been implicated in the etiology of migraine, and although results regarding variability of dopamine receptor genes are not conclusive, evidence clearly demonstrates the association between variability of the dopamine hydroxylase and the dopamine transporter genes and the pathogenesis of migraine with aura [104]. These results provide support for the role of antidopaminergic medications in the treatment of migraine with aura [105,106].
Useful evidence-based clinical guidelines for the diagnosis of migraine have been developed and are summarized in the mnemonic POUND: pulsatile headache; one-day duration (4 to 72 hours); unilateral location; nausea or vomiting; and disabling intensity [107,108].
Acute or episodic migraine with aura occurs in 25% to 30% of migraines. Aura is a combination of focal neurologic symptoms that precede or accompany an attack, progress for 5 to 20 minutes and last less than 60 minutes. Auras are the clinical manifestations of focal cortical spreading depression originated in the occipital cortex and moving at a rate of 2–3 mm/minute [34,41,42]. Visual auras such as scotomas ("blind spots" in the visual field), phosphenes (scintillations or flashing lights), and teichopsia (zigzag lines) are the most common and frequently affect half the visual field [75,109]. Neurologic auras such as dysarthria, paresis, and paresthesia require thorough clinical evaluation if they last for more than 60 minutes, are accompanied by paralysis or syncope, or occur for the first time in patients 50 years of age or older or in women after initiation of oral contraception [109,110]. In women, migraine with aura is associated with a twofold increased risk for cardiovascular events such as myocardial infarction and stroke [111].
Typically, the headache is unilateral, although bilateral occurrence is commonly reported. Up to 50% of patients with unilateral pain report that either side can be affected in any particular migraine episode [11,112]. It begins as a dull ache that, within minutes or hours, progressively develops into an intense throbbing pain that worsens with each arterial pulse. The pain is often disabling and interferes with professional, social, and familial commitments [11,20]. The temporal profile of acute or episodic migraine attack includes an initial premonitory phase, a headache phase either with or without aura, and a resolution or recovery phase.
In acute or episodic migraine without aura, up to 80% of patients have premonitory symptoms or prodromes, such as fatigue, irritability, difficulty concentrating, neck stiffness, cold hands, frequent urination, and/or change in appetite, that precede the headache by up to 48 hours. Some patients recognize their prodromes, allowing them to follow an early management approach and effectively abort or minimize subsequent headache [9,109].
In some patients, migraine can be initiated by variety of triggers, such as monosodium glutamate (MSG), excess caffeine, and foods rich in nitrites, sulphates, tyramine, and/or a vasoactive amine present in aged cheese, red wine, and chocolate. Decompression (e.g., high altitudes and scuba diving), dehydration, and fluctuating estrogen levels (e.g., menarche, menstrual period, perimenopause) have also been identified as potential triggers of migraine [75,113]. Knowledge of a patient's triggers can be helpful in preventing a migraine attack.
Gastrointestinal symptoms of nausea and vomiting are reported by 90% and 30% of patients, respectively [75,114]. A variety of other autonomic symptoms accompanying acute migraine attacks include constipation, diarrhea, abdominal cramps, nasal stuffiness, facial pallor, and diaphoresis. Neurologic symptoms of sensory hypersensitivity are commonly reported by patients during migraine attacks and are manifested as photophobia, phonophobia, or hyperosmia, and patients tend to seek a dark, quiet location to rest. A variety of psychologic symptoms (e.g., anxiety, depression, drowsiness, irritability, restlessness) are also present in patterns that vary among patients but usually have a predictable pattern in each patient [75,109,114].
Potential complications of migraine include [9]:
Status migrainosus: Persistent (>72 hours), debilitating migraine with or without aura, often caused by medication overuse
Persistent aura without infarction: Aura symptoms persisting for one week or more without evidence of infarction on neuroimaging, often bilateral and lasting for months or years
Migrainous infarction: One or more migraine aura symptom associated with an ischemic brain lesion in the appropriate territory demonstrated by neuroimaging, with onset during course of a typical migraine with aura
Migraine aura-triggered seizure: A seizure triggered by an attack of migraine with aura
As the cephalalgia resolves, many patients experience a sense of fatigue or exhaustion, irritability, impaired concentration and memory, mood changes, and neck stiffness. This postdrome phase can last from a few hours to up to two days after termination of the headache [9,75,109,114,115].
Additional criteria that are useful to assist in making the correct diagnosis of migraine include:
Absence of daily headache
Stable pattern
History of similar events
Family history of migraine
Normal neurologic examination
Improvement with rest and/or sleep
Association with menses
Absence of aura and lack of identification of a selective trigger should not eliminate the diagnosis of migraine [7,9,28,75].
Clinical examination of the patient should pay close attention to the presence of alarm signs that play a crucial role in the differential diagnosis between migraine and potentially lethal conditions such as stroke, SAH, and ruptured aneurism. These signs include [75,109]:
Acute headache with focal neurologic signs or papillary edema
Acute headache in a patient 50 years of age or older
Acute onset of a headache described as "the first of this kind" and "the worst ever"
Intensifying pain of a subacute headache
Headache associated with systemic illness (e.g., fever, stiff neck, nausea, vomiting, skin rash)
Acute headache in patients with cancer or human immunodeficiency virus/acquired immune deficiency syndrome (HIV/AIDS)
Several imaging studies, including PET and fMRI, have provided insight regarding the involvement of specific brain structures, such as the visual motion processing network, in the pathophysiology of migraine with and without aura [116,117]. Blood oxygen level-dependent MRI studies of the visual cortex have shown that both visual aura and cortical spreading depression correspond to an initial stage of noticeable hyperemia that lasts for three to five minutes, which is followed by one to two hours of oligemia (mild hypoperfusion) [31]. Diffusion tensor MRI showed an increase in thickness of the visual cortex in areas involved in cortical spreading depression and visual aura as well as changes in the superior colliculus and lateral geniculate nucleus, areas also implicated in visual processing [117,118,119]. Morphologic changes in brainstem regions involved in pain modulation (periaqueductal gray) and serotonin-producing neurons (dorsolateral pons) have also been reported [120]. MRI findings of periventricular focal white matter hypertense lesions are four times more frequent in migraine patients than in non-migraine age- and sex-matched controls [121]. However, most patients with migraine with aura do not consistently present with these imaging alterations [40]. These findings should be evaluated on an individual basis, considering the history and pattern of the headache and differential diagnosis of early stages of multiple sclerosis or vascular diseases [121].
Imaging studies have shown that brainstem hyperactivity ipsilaterally correlates to acute migraine, suggesting that lateralization of the pain relates to unilateral brainstem dysfunction and altered transmission in the trigeminal nucleus caudalis. Hyperactivity in the thalamus is associated with allodynia, and activity in cortical regions normally associated with pain processing is observed with imaging during acute migraine [116,122]. These studies are particularly important because they demonstrate that structural and functional changes occur during acute migraine and that changes in vascular function do not represent the primary cause of migraine attacks, further validating the role of cortical spreading depression and the neural etiology of migraine [122].
According to clinical guidelines from the American Academy of Neurology and the U.S. Headache Consortium, neither imaging procedures nor clinical laboratory tests specific for migraine are available. As such, these modalities are not usually warranted for patients with migraine and normal neurologic examination and no recent changes in headache characteristics. Less than 0.2% of patients in this category show clinically significant intracranial lesions on neuroimaging [7,8,116,123,124,125]. The presence of abnormal neurologic examination or changes in headache patterns, such as intensity and temporal profile, are considered "red flags" and prompt MRI imaging is appropriate for these patients (Table 1) [8].
SIGNS AND SYMPTOMS THAT SUGGEST A SECONDARY CAUSE OF HEADACHE AND REQUIRE FURTHER CLINICAL AND IMAGING EVALUATIONS
|
The diagnosis of migraine is based solely on a constellation of signs and symptoms, and a comprehensive medical and neurologic examination is required to exclude secondary headache [109]. Competence of the clinician and effective communication with the patient play a crucial role in the diagnosis of migraine. It has been estimated that 50% of migraine patients remain undiagnosed or misdiagnosed, and only a small number (8% to 10%) of individuals with migraine take migraine-specific medications such as triptans or ergotamines [126,127,128].
Of particular clinical relevance is mounting evidence of an increased comorbidity of migraine and neurologic (e.g., transient ischemic attacks, ischemic stroke, epilepsy), psychiatric (e.g., anxiety, depression, bipolar disorder), cardiovascular (e.g., Raynaud phenomenon, angina, myocardial infarction), and metabolic (e.g., hypercholesterolemia, insulin resistance, obesity) disorders [75,111,129,130,131,132,133,134]. When compared with the rest of the population, patients with migraine with aura have a doubled risk of developing an ischemic stroke [135]. Migraine with aura in women using oral contraceptives has been identified as a risk factor for cardiovascular comorbidity [9]. Particularly relevant are the seven-fold higher odds of stroke in women with migraine with aura who smoke and take oral contraceptives compared with women with probable migraine with visual aura who do not smoke or use oral contraceptives [136].
Chronic migraine is defined as headaches that occur on 15 or more days per month for more than three months, which have the features of migraine headache on at least eight days per month [9]. The criterion that a patient must have at least 15 days of headache monthly is not intended to be restrictive, but rather a guideline that patients with a high number of monthly headaches should be included in this group and receive appropriate therapy [28,29].
Chronic migraine has a prevalence of 1% to 2%, and it represents approximately half of all cases of chronic primary headache. It is more frequently observed in women of European heritage, in patients who are obese, and during the fourth decade of life [24,26,137].
In chronic migraine, it is impossible to distinguish the individual episodes, and the characteristics of the headache often change frequently, even within the same day. It is also difficult to keep patients medication-free in order to observe the natural history of the headache. The most common cause of symptoms suggestive of chronic migraine is medication overuse, and in at least 50% of these patients, the condition is reversed after discontinuation of medications. Other patients, however, do not improve after drug discontinuation and their condition should not be diagnosed as medication-overuse headache [9,29]. Patient education regarding the judicious use of medications should begin before rather than after medication-overuse headache is established [109].
In addition to the findings of imaging studies related in the previous section, dysfunction of the descending inhibitory pathways is also observed in chronic migraine, resulting in hypofunction of the descending pain modulatory circuitry [138]. Chronic migraine should respond favorably to pharmacologic treatment with ergots or triptans [29].
The pattern of migraine presented by a patient changes over the lifetime, and its assessment determines the combination of clinical management with patient education, pharmacologic treatment, and behavioral interventions [109]. This evaluation takes into account frequency, intensity, and impact of migraine on the patient's life [109]. Based on the findings, patients may be categorized in one of four stages and treated accordingly.
In stage one, patients have one or fewer migraine attacks per month or two or fewer headache days per month and normal function between episodes. Early administration of over-the-counter medication (e.g., ibuprofen, naproxen, or a combination of acetaminophen, aspirin, and caffeine) and sleep are usually adequate to manage the condition. The patient is fully functional within a few hours and rarely presents for consultation. If severe pain is experienced, patients may seek medical treatment, and in these cases, either triptans or nonsteroidal anti-inflammatory drugs (NSAIDs) are usually effective to stop a migraine attack [109].
Patients in stage two present with one to three attacks monthly, with less than five headache days per month. Each event is limited in time, but occasional absenteeism from work or family or social functions may occur. Treatment with triptans, either alone or in combination with NSAIDs (e.g., sumatriptan, naproxen), is usually effective to stop a migraine attack [109]. Patient education should be aimed at limiting the use of analgesics to prevent medication-overuse headache, emphasizing that the use of analgesics should be limited to the early management of individual acute migraines and the need to limit drug administration to no more than twice per week [109].
In stage three, patients present with frequent attacks (four to eight per month with less than 12 headache days per month). Assessment should include the use of acute medications (NSAIDs and triptans) and determination of possible medication overuse. It is important to set strict limits on medication use or opt for discontinuation, with preventive therapy initiated concurrently. The choice among preventive medications should take into account the existence of comorbidities, such as beta-blockers in patients with hypertension and tricyclic antidepressants in patients with depression. However, it is important to remember that the appropriate dosage for prevention of migraine might be below the therapeutic effective for the comorbid condition [109].
Patients in stage four have more than eight attacks per month and more than 15 days of headache per month. These patients should be treated by headache specialists on interdisciplinary teams focused on pain management. Medication overuse should be evaluated in each patient and appropriately managed. The medication should be discontinued, and if necessary, a bridging therapy—such as naratriptan (1 mg twice daily for five days) or naproxen (440 mg twice daily for five days)—can be initiated to prevent or manage rebound headaches from the medication withdrawal. Preventive pharmacotherapy should preferably be initiated after discontinuation of previous medication(s). Management of patients with complex migraine often requires referral and interprofessional collaboration [139].
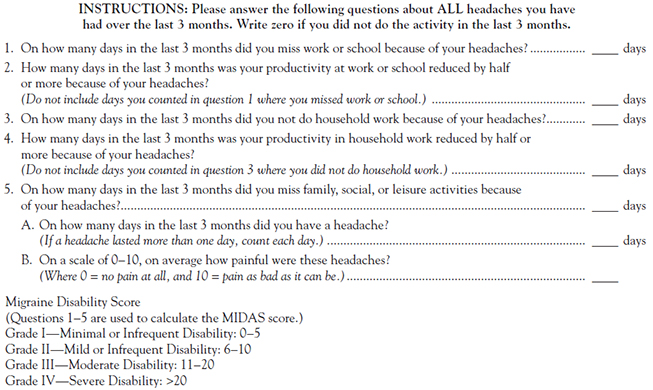
After migraine is properly diagnosed, the severity of the disease and its impact on quality of life and ability to function should be assessed using the Migraine Disability Assessment (MIDAS) questionnaire, a simple and reliable tool (Figure 1) [140,141].
Differentiating migraine from other primary or secondary headaches requires a thorough medical history and physical examination and an understanding of the typical characteristics of primary headaches. The initial differential diagnosis of migraine considers three main areas: other primary headaches, secondary headaches, and orofacial pain. Some red-flag signs and symptoms—including focal neurologic signs, papilledema, neck stiffness, an immunocompromised state, sudden onset of the worst headache in the patient's life, personality changes, headache after trauma, and headache that worsens with exercise—suggest serious underlying pathology and require neuroimaging and/or laboratory testing to evaluate the cause of headache.
Tension-Type Headache
Tension-type headache is the most common primary headache. The pain is dull and non-pulsating, with a mild-to-moderate intensity and a bilateral or a "hatband" distribution. Typically, tension-type headache is not associated with aura, nausea, or vomiting. Mild photo- or phonophobia may infrequently be reported. Palpation of the cervical or pericranial muscles may identify tender spots [7,11,75].
NSAIDs are effective drugs of choice in the treatment of tension-type headache. Ibuprofen (400 mg) and naproxen sodium (550 mg) provide better analgesia than acetaminophen (1,000 mg) and have fewer adverse effects than aspirin (650 mg). However, the choice should take into account cost and individual patient preference. Amitriptyline (10–25 mg at bedtime) is the most effective in the prophylaxis of tension-type headaches [11].
Cluster Headache/Trigeminal Autonomic Cephalalgias
Cluster headache and TACs are severe and uncommon headaches with a shorter duration (15 to 180 minutes) than migraine and occur up to eight times per day [9,11]. Cluster headache is more common in men than in women (at a ratio of 3:1) with age of onset between 20 to 40 years of age [9]. It often occurs at night and wakes patients from their sleep. Typically, cluster headache presents as a unilateral headache located behind the eye and radiating to the territory of the ipsilateral trigeminal nerve. It occurs in clusters followed by periods of complete remission that can last for weeks to months. Aura and gastrointestinal symptoms are not observed, but ipsilateral lacrimation, conjunctival injection, rhinorrhea, and blocked nasal passage are typically present [11,142]. Relevant to the differential diagnosis, patients experiencing a cluster headache do not seek rest during an attack but are noticeably agitated, restless, pacing, rocking, and even aggressive. This is in sharp contrast to patients with migraine, who seek relief by resting in a dark, quiet place and prefer to remain motionless during attacks [7,9,10,51,142]. The standard treatment for cluster headache/TAC is high-flow oxygen (100% O2 at 7–10 L/min for 15 to 30 minutes).
In addition to supplemental oxygen, sumatriptan and zolmitriptan are effective in the acute treatment of episodic cluster headache. Verapamil (240 mg/day) has been the first-line prophylactic therapy and can be used to treat chronic cluster headache; however, the CGRP antagonist galcanezumab-gnlm received FDA-approval in 2019 for cluster headache prophylaxis [81,143]. Further clinical studies are required to compare the effectiveness of these agents. Lithium (800–900 mg/day) is also effective, although it requires closer monitoring for adverse effects (e.g., hypothyroidism). More invasive treatments, including nerve stimulation and surgery, may be helpful in refractory cases [11,51,75,142,144,145].
Thunderclap Headache
Thunderclap headache occurs suddenly, reaches peak intensity in less than one minute, and lasts for at least five minutes and up to 24 hours. Patients often describe thunderclap headache as the "worst headache of their lives." These headaches are often associated with life-threatening vascular intracranial disorders such as SAH, intracerebral hemorrhage, cerebral venous sinus thrombosis, ischemic stroke, arterial dissection, and hypertensive encephalopathy [11,146,147]. Primary thunderclap headache should be a diagnosis of last resort, reached only when all organic causes have been demonstrably excluded [9].
Differentiating among thunderclap headache, migraine, and serious secondary headaches requires a comprehensive examination and initial CT scan and CSF analysis, possibly followed by an MRI if these are negative or inconclusive. Primary thunderclap headache responds poorly to analgesics, and the best management is provided by nimodipine (a dihydropyridine calcium channel antagonist) or gabapentin [51,146].
Clinical history and patient examination also play a critical role in differentiating migraine from potentially life-threatening secondary headaches resulting from SAH, cerebral parenchymal hemorrhage, cerebral vein thrombosis, cavernous sinus thrombosis, increased intracranial pressure, meningitis/encephalitis, hypertensive emergency, brain metastases, and HIV/AIDS [51,124,148]. A change in severity, frequency, or characteristics of the headache, the presence of a new progressive headache that persists for days, or headache developing after head trauma or associated with neck stiffness or fever is suggestive of secondary origin. Headache is also reported by 50% of patients diagnosed with either primary or metastatic brain tumor, with characteristics typical of migraine in 9% of patients and of tension-type headache in 77%; in one study, "classic" early morning brain tumor headache occurred in only 17% of patients [149].
Differential diagnosis of secondary headache requires a detailed history and thorough examination. If the situation is unclear, an initial CT scan of the head without contrast and CSF analysis are required, possibly followed by an MRI [51,124,148].
The multifaceted etiology of oral, facial, and head pain is the result not only of various pain mechanisms but also of the complex anatomy of the head and orofacial region. Its diagnosis and management often require a multidisciplinary approach and collaboration [150,151,152].
Approximately 20% of the population experiences orofacial pain more than once every six months [153]. Odontogenic pathology is the most common cause of orofacial pain, followed by nonodontogenic pain (e.g. temporomandibular disorders, neuropathies) and burning mouth syndrome [154,155]. Primary headaches, such as migraine, cluster headache, and tension-type headache, can also present as pain with orofacial location. The most prevalent etiology of nonodontogenic orofacial pain is musculoskeletal pathology (e.g., temporomandibular disorders), followed by episodic or chronic neuropathies (e.g., post-traumatic, trigeminal, post-herpetic) and oral cancer [151,156]. Sinusitis may also cause orofacial pain and headache, and a careful assessment of the patient is required to establish a differential diagnosis [9,55,154,157].
Odontogenic Pain
Odontogenic pain is caused by odontogenic pathology, such as injury or inflammation/infection of the dental pulp or periodontal tissues, and accounts for more than 50% of all orofacial pain [158]. Clinical and radiographic examination should be corroborated by at least one other test aimed at differentiating between odontogenic and nonodontogenic pain, including percussion, palpation, biting, or thermal. If radiographic and clinical examination are both negative, then two of these other tests must be positive in order to correctly establish the diagnosis and location of the pain [158].
Dentin hypersensitivity presents as a transient sharp pain in response to thermal, chemical, or tactile stimulation. Dental caries present as painful response to any stimulation and can be easily confirmed by clinical and radiographic examination.
Pulpitis is an inflammation of the dental pulp caused either by caries or fracture. Reversible pulpitis is a mild inflammation and presents as localized, sharp, and intermittent pain elicited by thermal changes, particularly cold drinks. Irreversible pulpitis results from chronic inflammation and infection associated with pulpar necrosis, which can be either associated with throbbing pain with no response to thermal stimuli or with poorly localized, dull, and persistent pain [158,159]. A localized periapical abscess is a common complication of pulpitis, and symptoms include tenderness on tapping and lymphadenopathy. This condition requires dental referral for drainage and subsequent reconstruction or extraction; antibiotics are usually not recommended. If the infection has spread to adjacent teeth or surrounding tissues, causing cellulitis, or if the clinical situation does not allow for immediate dental surgical treatment, appropriate antimicrobial therapy with broad-spectrum antibiotics, specifically amoxicillin with clavulanate, should be initiated before referral. Clindamycin is a recommended alternative, particularly in patients with an allergy to penicillins [158,159,160]. It is important to remember that antibiotics are not substitutes to curative dental treatment. In fact, very seldom are antibiotics an appropriate substitute for removal of the source of the infection (i.e., extraction, endodontic treatment, incision and drainage, periodontal scaling and root planing) [160].
Periodontalgia resulting from gingivitis or periodontal abscess is not as deep-seated, intense, and throbbing as endodontic pain. This pain is associated with gingival inflammation, localized bleeding, and tooth mobility and is usually more generalized than endodontic pain. Antibiotic therapy is an option, and referral to periodontal treatment is required [158].
Nonodontogenic Tooth Pain
Nonodontogenic tooth pain is defined as pain that presents as tooth pain but without dental pathology. Although it often coexists with true tooth pathology, its true nature is revealed when the dental pain is treated. It can present as a deep, dull ache with occasional lancinating pain in the ear, temple, or face. The most prevalent etiology of nonodontogenic tooth pain is muscular. These presentations include myospasm, myalgia, and myofascial pain syndrome, with pain elicited by the stimulation of trigger points in the muscles involved. For example, stimulation of the anterior digastric muscle trigger points can cause referred pain in the lower incisors, whereas stimulation of the anterior or posterior temporal muscle trigger points causes pain in the maxillary anterior or posterior teeth, respectively [161]. Local injection of neuromuscular blocker botulinum toxin (e.g., Botox, Dysport, Xeomin) is effective treatment.
Atypical odontalgia, also known as neuropathic tooth pain, neurovascular odontalgia, oral neuropathic pain, or atypical facial pain, is a nonodontogenic pain of neuropathic origin. Classically, atypical odontalgia presents as throbbing, persistent pain in the teeth or alveolar process occurring over a prolonged period of time without any pathologic, clinical, or radiologic findings [162]. Onset can coincide with dental treatment, including denervation or dental extraction, a condition known as phantom tooth pain [163]. Most patients are women in their mid-40s, and they are often misdiagnosed and submitted to repeated endodontic therapy and dental extractions that fail to relieve their pain [164]. Diagnosis and management are challenging, but tricyclic antidepressants such as amitriptyline or imipramine are the treatment of choice. Gabapentin, baclofen, topical anesthetics, and opioids are possible alternatives [165].
Temporomandibular Disorders
Temporomandibular disorders have a lifetime prevalence of 75% and account for approximately 5% of orofacial pain that requires therapeutic management [154,155]. These disorders are associated with usually unilateral pain with temporal, periorbital, or frontal location. The pain is persistent and dull, with well-localized trigger points in the muscle, fascia, or tendons. Temporomandibular pain of myogenous origin includes jaw and facial pain arising from masticatory muscles, whereas pain of arthrogenous origin is associated with joint noise, incoordination of the disk-condyle relationship either with or without locking, and limited range of motion.
Typically, temporomandibular pain is triggered or aggravated by clinical examination with palpation, passive movement, and active movement (e.g., yawning, chewing, talking) and intensified when muscle is contracted against fixed resistance [154,166,167]. The role of temporomandibular disorder as a cause of chronic headaches and facial pain is often overlooked, and patients may be misdiagnosed as suffering from daily migraines or chronic sinusitis or rhinitis [154,157].
Imaging with MRI is indicated to study soft tissues and assess disk position. In the past, panoramic and tomographic studies were considered the most appropriate to evaluate bone, although cone-beam CT is now the first choice [154]. Referral to an expert in temporomandibular pain is advised to establish the treatment plan, which will be determined by the degree of impairment and complexity of the disorder. Interventions range from patient education (e.g., avoid chewy foods and chewing gum) and physical therapy (e.g., apply heat or ice, perform jaw-stretching exercises) to pharmacotherapy with NSAIDs, muscle relaxants, botulinum toxin, sedatives, corticosteroids (e.g., methylprednisolone, triamcinolone), or topical analgesics (e.g., capsaicin, lidocaine in transdermal patch). Advanced and complex cases require surgery (e.g., arthrocentesis, arthrotomy, joint replacement) [151,154].
Sinusitis and Rhinosinusitis
Sinusitis and rhinosinusitis are potential causes of facial pain and headache. The floor of the maxillary sinus is in close proximity to the roots of the maxillary teeth, specifically the second premolar and the first premolar. It might extend as far anteriorly as the canine and posteriorly as far as the third molar [168]. Up to 11% of patients with maxillary sinusitis report toothache, and the involved maxillary teeth may be tender to percussion and hypersensitive to cold stimuli, with tenderness, edema, and erythema of the oral mucosa adjacent to the compromised sinus. Periapical radiographs may also illustrate widening of the periodontal ligament. Together, this constellation of signs and symptoms requires a thorough history and examination [168,169,170].
The frontal, ethmoid, and sphenoid sinuses are each contiguous with the intracranial vault, and congestion or inflammation in any of these sinuses frequently leads to headache, the character and location of which is determined by the specific sinus involved. The floor of the frontal sinus forms a portion of the roof of the orbit. Frontal sinusitis causes pain (headache) above the eye in the frontal region of the skull, accompanied by local tenderness and occasionally slight edema of the eyelid. This headache often occurs mid-morning and is aggravated by bending forward. The ethmoid air cells are variable in number and occupy the boney area between the nasal cavity and the medial wall of the orbit. Headache associated with anterior ethmoid sinusitis is referred to the parietal area of the head, while posterior ethmoiditis causes headache in the mastoid or occipital regions. The sphenoid sinus is located behind the orbit, and the roof of this sinus forms the pituitary fossa at the base of the brain. Sphenoid sinusitis produces a deep, boring retro-orbital pain and coronal headache that can become severe and unremitting.
The cardinal clinical features of sinusitis are nasal congestion/obstruction, purulent nasal discharge, and pain (regional facial pain and/or headache). Commonly, the discomfort of sinus congestion becomes worse when the patient bends over or lies down. Sinusitis may be unilateral or bilateral and more than one anatomic sinus is often affected (e.g., fronto-maxillary or fronto-ethmoid sinusitis). Regional pain may be accompanied by the sensation of periorbital and frontal pressure, and there may be localized tenderness, mild erythema, or edema adjacent to the involved sinus. Fever is not a prominent feature and is more common in children than in adults. Complaints of increased post-nasal drainage and cough, particularly at night, are common. The diagnosis can usually be made by careful clinical assessment combined with sinus transillumination and, perhaps, plain radiographs of the face ("sinus views"). Head neuroimaging is reserved for persistent, recurrent, or complicated cases.
Sinusitis usually develops as a complication of viral upper respiratory infection or nasal allergy; however, persistent or progressive symptoms are often the result of secondary bacterial infection. The treatment regimen is designed to promote drainage, relieve pain, and treat bacterial infection. A systemic and/or topical decongestant (e.g., phenylephrine, oxymetazoline) should be administered, perhaps combined with nasal corticosteroid (e.g., fluticasone, mometasone) for patients if nasal allergy is prominent. Amoxacillin, either alone or in combination with clavulanate, is the antibiotic of choice for most cases [171,172].
Patients suffering from daily migraines may be misdiagnosed with chronic sinusitis or rhinitis and repeatedly and unsuccessfully treated with broad-spectrum antibiotics [154,157]. A systematic review found that if thorough otolaryngologic and neurologic examinations are performed, the majority of patients presenting with sinus headache in the absence of significant acute inflammatory findings are diagnosed with migraine. The researchers recommend that the appropriate treatment for these patients is migraine-specific medication [173].
Giant Cell Arteritis
Giant cell arteritis should be considered as part of the differential diagnosis of orofacial pain in patients 50 years of age and older [174]. Arteritis of the temporal artery presents as sudden, severe, and pulsating temporal pain that worsens with cold temperatures. Patients also often display tenderness to palpation, jaw claudication with limited range of motion, and allodynia of the scalp. It is commonly associated with signs of systemic inflammation (e.g., fever, fatigue, malaise, anorexia, sweating). The constellation of signs associated with the throbbing temporal pain in giant cell arteritis allows for a reliable differential diagnosis with migraine. Imaging tests may appear normal, but laboratory tests will show elevated erythrocyte sedimentation rate (ESR) and C-reactive protein. Giant cell arteritis is considered a medical emergency because partial or total obstruction of the blood vessel may result in transient ischemic attacks, stroke, or permanent loss of vision. Prompt treatment with prednisone (starting at 10–20 mg and increasing up to 60 mg/day), either alone or in conjunction with aspirin (81 mg/day), is very effective in most cases. ESR values can be used to monitor progression and response to therapy [175,176,177].
Burning Mouth Syndrome
Burning mouth syndrome, also referred to as glossodynia, is a condition of unclear (possibly neuropathic) etiology, and diagnosis is established when other known causes (e.g., xerostomia, candidiasis, diabetes mellitus, food sensitivity, deficiencies in vitamin B12 or iron) have been excluded. As the diagnosis is made by exclusion of other known conditions, a detailed medical history and pain history are required [178]. The International Headache Society defines burning mouth syndrome as "an intraoral burning or dysaesthetic sensation, recurring daily for more than two hours per day over more than three months, without clinically evident causative lesions" [7]. It is most commonly observed in postmenopausal women and is usually confined to the tip of the tongue. It may be associated with xerostomia and loss of taste (ageusia) [179,180]. Burning mouth syndrome may develop as an adverse effect of angiotensin-converting enzyme inhibitors, with the condition subsiding after drug discontinuation [178]. If pharmacotherapy is required, clonazepam and gabapentin are the most commonly prescribed drugs for this condition [180].
Nonpharmacologic alternatives to migraine treatment include a variety of lifestyle changes and complementary and alternative therapies. Lifestyle changes play an important role in the prevention of acute as well as chronic migraine [29,109]. These changes include a structured lifestyle, healthy diet, consistent hydration, regular exercise, regular sleep patterns, quitting smoking, avoidance of specific headache triggers (e.g., excess caffeine, alcohol, chocolate), and avoidance and management of stress. Increased general fitness and moderate physical activity, such as 30-minute walks three to five times per week, are recommended, although high-intensity exercise and irregular patterns of exercise may trigger headache [181].
Complementary and alternative therapies, such as relaxation techniques, biofeedback, cognitive-behavioral therapy, massage, acupuncture, botulinum toxin, coenzyme Q10, vitamin B12 or B2 supplementation, and herbal medications such as feverfew (Tanacetum parthenium) and butterbur (Petasites hybridus), have also been evaluated in migraine prophylaxis, with varying levels of success [182,183,184,185,186]. Patient education is another important tool in migraine management, and useful information for migraineurs is available online (Resources).
The management of acute migraine attacks includes pharmacologic and nonpharmacologic approaches. The patient will usually first cope with symptoms by lying down in a dark and quiet location. However, medication is often necessary. The appropriate drug choice takes into account the severity of the attack and previous individual response to specific medications. An estimated 50% to 70% of mild and moderate migraine attacks can be managed with oral medications; severe events require parenteral treatment. As a general rule, medications used to alleviate the pain of a migraine attack should be taken early after onset, when the headache is still mild.
The U.S. Headache Consortium has identified several goals for the treatment of acute attacks [187,188]:
Treat the attacks rapidly and consistently and eliminate recurrence of the attack
Restore the patient's ability to function
Minimize the use of backup and rescue medications
Optimize self-care and reduce subsequent use of resources
Institute cost-effective approaches for overall management
Minimize or avoid adverse events
A comparison of the effectiveness of various abortive medications is limited due to the paucity of clinical trials directly comparing different drug classes. However, five general guidelines have been developed [187,188]:
Educate patients with migraine about their condition and its treatment and encourage them to participate in their own management.
Use migraine-specific agents in patients with more severe migraine and in those whose headaches respond poorly to NSAIDs or combination analgesics such as aspirin plus acetaminophen plus caffeine.
Select a non-oral route of administration for patients whose migraines are characterized by nausea or vomiting early in the course of an attack.
Consider use of a self-administered rescue medication for patients with severe migraines that fail to respond well to other treatments.
Guard against medication-overuse headache.
Face-to-face education with a healthcare professional has been found to increase medication efficacy by 11% compared with written patient instructions without altering the placebo response [109].
Lifestyle modifications, including identification and avoidance of possible triggers and adherence to a structured sleep schedule, are an effective and often neglected tool in the prevention and management of migraine [181,189]. The role of exercise is supported by a three-month randomized, controlled trial that showed exercising for 40 minutes three times per week provided benefits comparable to relaxation according to a recorded program or daily topiramate use titrated to the individual's highest tolerable dose (maximum: 200 mg/day) [190].
The primary endpoint in the acute treatment of migraine is to optimize the number of patients who are pain-free at two hours after administration of medication, and prompt initiation of treatment as soon as possible after first symptoms provides the maximum benefit [105,107,191,192,193]. Medications used in the treatment of acute migraine attacks are either non-specific analgesics, such as NSAIDs, acetaminophen, and opioids, or migraine-specific drugs, such as agonists at the serotonin receptor 5-HT1B/1D (ergots and triptans) and dopamine antagonists.
It should be noted that opioids are not recommended in the treatment of acute migraine, except when administered intravenously in the emergency department [194]. Opioid treatment is associated with a high recurrence rate of migraine headache and an inherent potential for misuse, abuse, and dependence. It is recommended that opioids may only be considered for short-term use in cases of intractable, severe migraines or end-of-life care [195].
Clinical practice guidelines developed by the Institute for Clinical Systems Improvement recommend a stepwise escalation of medical management of migraine headaches. Treatment of severe migraine headache in emergency settings should start with triptans and NSAIDs, progressing to dihydroergotamine and ultimately neuroleptics. Opioids and dexamethasone may be added as adjuncts in refractory cases [188,196].
Non-Specific Medications
The heterogeneous group of non-specific migraine medications consists of a variety of drugs that do not target the 5-HT1B/1D serotonin receptor. This includes anti-inflammatory medications and/or analgesics (e.g., NSAIDs, opioids, corticosteroids), antidopaminergics, (e.g., metoclopramide, chlorpromazine, haloperidol), antihistamines (e.g., diphenhydramine, dimenhydrinate, hydroxyzine), steroids (e.g., dexamethasone, prednisone), anticonvulsants (e.g., valproate), anesthetics (e.g., lidocaine, bupivacaine, nitrous oxide, propofol), and magnesium sulphate.
NSAIDs inhibit the neuroinflammatory cascade that leads to release of vasoactive mediators that cause vasodilation. They also inhibit the release of prostaglandins that activate nociceptive neurons in the trigeminal nucleus [192]. More than 50% of patients use non-prescription NSAIDs effectively to treat acute migraine, and those who present with complaint of migraine have usually tried these medications unsuccessfully [6,107,197]. NSAIDs evaluated for the treatment of acute migraine include a combination of acetaminophen, aspirin, and caffeine (Excedrin Migraine, two tablets every six hours, for a maximum of 48 hours), ibuprofen (Advil, Motrin, generic, 400 mg every three to four hours), and naproxen (Aleve, generic, 200–550 mg twice per day). When administered early in a migraine attack, NSAIDs are effective, and they are approved by the U.S. Food and Drug Administration (FDA) for the treatment of mild-to-moderate attacks [6,51,107,197]. Ketorolac (30 mg IV or 60 mg IM) has also been shown to be effective and is recommended for acute treatment in emergency settings [106,198,199,200].
As discussed, opioids (e.g., morphine, fentanyl, buprenorphine, meperidine, nalbuphine, tramadol) are not currently recommended in the treatment of acute migraine, except when administered intravenously in the emergency department, when necessary for end-of-life care, and when effective analgesia was not achieved and patients are not able to tolerate specific medications due to pre-existing comorbidity (e.g., cardiovascular disease) [106,194,195,198,201]. In these cases, intractable migraine pain may be managed with an opioid (not meperidine) or dexamethasone. However, if at all possible, clinicians should avoid opioids. The brief pain-relief window, induction of inflammatory neurochemical release, and vasodilatation are counterproductive to treatment issues and migraine pathophysiology. Meperidine is not recommended because its neurotoxic metabolite (normeperidine) may promote seizures [196].
Antidopaminergic drugs may be categorized as either antiemetics (e.g., metoclopramide) or neuroleptics (e.g., chlorpromazine, haloperidol, droperidol). Several antiemetics, including metoclopramide, are effective in the management of nausea in acute migraine. Metoclopramide blocks D2 dopamine and 5-HT3 serotonin receptors in the chemoreceptor trigger zone and accelerates gastric emptying. Its antidopaminergic properties also offer additional antimigraine effects [107]. Metoclopramide (Reglan) 10–20 mg IV is used in emergency settings, and its efficacy is supported by an exhaustive review of the literature published in 2015 [198,200]. Granisetron (Granisol), a selective 5-HT3 antagonist, has also been used in the emergency settings, although studies are limited and show a greater risk of adverse effects [105,198]. One study showed that granisetron is more beneficial than metoclopramide, because it also controls migraine-related emesis [202]. However, more studies are required to determine if the benefits outweigh the risks of granisetron.
The butyrophenones haloperidol (Haldol, generic, 5 mg in 500 mL IV solution) and droperidol (Inapsine, generic, 0.1–2.5 mg IV) are effective in 80% and 54% of the patients, respectively [105]. Common side effects include sedation and akathisia, and these effects have resulted in almost 20% of patients being unwilling to be treated with haloperidol again [203]. The neurologic side effects of butyrophenones and their cardiovascular risks (e.g., QT prolongation, arrhythmias) outweigh their benefits, and their use in the treatment of acute migraine is generally not recommended [198,200].
The phenothiazine neuroleptics, prochlorperazine (10 mg IV) and chlorpromazine (12.5–25 mg IV), have been found to provide pain relief to up to 90% and 70% of patients, respectively [105,198]. Side effects are less common with prochlorperazine than with chlorpromazine, but both agents are recommended in the treatment of acute migraine in emergency settings [105,198].
Antihistamine drugs (e.g., diphenhydramine, hydroxyzine) have been evaluated in combination with other medications for the treatment of acute migraine attack, with variable outcomes [105]. One trial showed benefits with diphenhydramine 12.5 mg IV plus prochlorperazine 10 mg IV, when compared with sumatriptan 6 mg subcutaneous [204]. However, another trial found that there was no improvement to migraine when diphenhydramine 50 mg IV was added in conjunction with metoclopramide 10 mg IV [205]. More high-quality data are required to determine the efficacy of diphenhydramine administered in combination with other drugs for the treatment of migraine.
The anticonvulsant valproate (900–1,200 mg IV) has been evaluated for intractable migraine attack in emergency settings, with a reduction in pain within 50 to 60 minutes in 75% of patients [206]. However, its use as acute therapy is not recommended due to a lack of clear evidence of a favorable risk-benefit profile [198].
In patients with severe acute migraine resistant to treatment, anesthetics may be considered. Topical 4% lidocaine (0.5 mL) may be administered either by the physician or the patient into the nostril of the affected side over 30 seconds, with patient in the supine position [105,107,207]. Intravenous lidocaine and propofol are not recommended, as serious side effects outweigh possible benefits [198].
Steroids—specifically dexamethasone (IV 6–24 mg) or prednisone (40 mg/day)—are used as adjuncts to the standard emergent treatment of migraine [208]. These agents act to suppress inflammation underlying migraine. In one study, combined dexamethasone (6 mg IV) plus metoclopramide (5–10 mg IV) provided migraine pain relief at 30 minutes in approximately 80% of patients, an outcome similar to dihydroergotamine (0.75–1 mg IV) plus metoclopramide (5–10 mg IV) [208]. Steroids should be used cautiously in diabetic patients. Repeated administration increases the risk of osteoporosis and well-known endocrine disorders [107,192].
Magnesium has also been used in the treatment of acute migraine, and interestingly, up to 50% of patients have lowered levels of magnesium in the plasma during an acute migraine attack [191,209]. Magnesium has an effect on a variety of neurotransmitters and receptors underlying acute migraine, including serotonin receptors, NMDA receptors, nitric oxide, and substance P [191,209]. Research has shown that magnesium sulphate (1 g IV) is effective in 80% of patients 15 minutes postinfusion in emergency settings [191,210]. The most common adverse effect is facial flushing. Considering that only a few small clinical trials have evaluated the efficacy of magnesium, the established guidelines do not recommend its use in the treatment of acute migraine [198,201].
Migraine-Specific Medications
Moderate and severe acute migraines are more effectively treated with migraine-specific medications, particularly ergots and triptans. Interestingly, these medications do not have analgesic properties; rather their clinical effectiveness results from their targeting of the pathophysiologic mechanism underlying migraine. Migraine-specific medications are agonists at the serotonin 5-HT1B/1D autoreceptor, preventing release of serotonin from the presynaptic terminals and causing vasoconstriction of the meningeal blood vessels. These drugs also target the serotonin autoreceptors on terminals of the trigeminal nerve, which results in the inhibition of the release of proinflammatory vasoactive peptides and inhibition of nociceptive transmission in the brainstem [69,71,126,211].
The ergot alkaloids ergotamine and dihydroergotamine are non-selective agonists at the 5-HT1 serotonin receptor, with a lower affinity for alpha-adrenergic and dopaminergic receptors. On the other hand, triptans are considered to be highly selective agonists at the 5-HT1B/1D serotonin receptor subtype, with lower affinity for binding to other serotonin receptors.
Ergotamine is available in oral formulation (Ergomar) or in combination with caffeine for either oral (Cafergot) or rectal (Migergot) administration. Dihydroergotamine is available for nasal administration (Migranal, generic) or for IV and subcutaneous injection (DHE, generic). The use of ergots has declined since the introduction of triptans, although clinical studies have demonstrated that both drug groups have a similar efficacy in the treatment of acute migraine [195]. Adverse effects of ergots include nausea and vomiting, tingling of the extremities, muscle cramps, and chest discomfort [195]. As discussed, 5-HT1B/1D receptors are also expressed in high levels in the coronary arteries, resulting in the increased potential for adverse cardiac effects (i.e., coronary vasoconstriction) associated with ergotamine derivatives and triptans [195]. Ergots are contraindicated in patients with heart conditions or hypertension, and any chest or cardiac symptoms should be appropriately evaluated [69,70,81,195]. Dihydroergotamine is oxytocic and should not be used during pregnancy or breastfeeding [81,211]. Dihydroergotamine causes fewer adverse effects than ergotamine, but the use of any ergot alkaloids should be avoided within 24 hours of administration of triptans and serotonergic agonists, due to risk of severe vasoconstriction, and within two weeks of discontinuing monoamine oxidase (MAO) inhibitors. Ergots are contraindicated with potent inhibitors of CYP3A4, such as azole antifungals, macrolide antibiotics, and protease inhibitors [81,191].
Triptans are considered the first-line therapy for the acute treatment of migraine in patients resistant to NSAIDs. As noted, triptans have a higher selectivity than ergots for the 5-HT1B/1D receptors and very low or no affinity for adrenergic or dopaminergic receptors. Their clinical efficacy results from their vasoconstrictive properties, which are mediated by their binding to the 5-HT1 receptors abundant in meningeal blood vessels [69,70,211]. As of 2024, seven triptans are available in the United States: naratriptan (Amerge), rizatriptan (Maxalt), eletriptan (Relpax), sumatriptan (Imitrex), zolmitriptan (Zomig), almotriptan (Axert), and frovatriptan (Frova). The pharmacodynamic properties and efficacy of all triptans are similar, and their clinical variability relates to the route of administration and individual patient response [81,191,195]. Failure or intolerance to one triptan warrants the trial of an alternative agent [191,195]. It is advisable to switch from one oral triptan to another if three migraine attacks have been treated without success [38]. In one study, sumatriptan 50 mg was similar to ibuprofen 400 mg and to effervescent aspirin 1,000 mg in reducing moderate-to-severe migraine pain, although sumatriptan was superior to the other medications at two hours after administration [212]. A combination of sumatriptan 85 mg and naproxen 500 mg (Trexima) has been shown to provide better pain relief than either drug alone [107]. However, prediction of a patient's response to a particular medication is difficult, and complete pain relief within two hours is only achieved in 45% to 77% of patients taking triptans [107,213].
Potential side effects of triptans include paresthesias, dizziness, flushing, chest pain, nausea, vomiting, local bleeding, bruising at the site of the injection, and nasal discomfort and dysgeusia for intranasally administered drugs [81,191,195]. Triptans are contraindicated in patients with a history of myocardial infarction, cerebrovascular accident, Prinzmetal angina, uncontrolled hypertension, and patients treated with MAO inhibitors. Patients being treated with selective serotonin reuptake inhibitors should avoid triptans due to the increased risk of life-threatening serotonin syndrome [107,126]. In 2014, analysis of the 16-year Sumatriptan, Naratriptan, and Treximet Pregnancy Registry found that the risk of major birth defects following in utero exposure to these drugs during the first trimester was not increased when compared with studies of birth defects among migraineurs with and without other medication exposure during pregnancy [214]. However, the authors caution that these findings should not be extrapolated to other medications in the triptan class, and triptans are usually avoided during pregnancy [214]. Additionally, a 2017 study supported the position that triptans have no effect on pregnancy outcome, although it was noted that sumatriptan is the best-studied triptan and, therefore, likely the safest choice [205].
In 2019, lasmiditan, a ditan, was approved for the treatment of migraine [81]. Lasmiditan is similar to a triptan but is a high-affinity, highly selective 5-HT1F receptor agonist. The selective targeting of the 5-HT1F receptor is hypothesized to decrease stimulation of the trigeminal system and treat migraine pain without causing vasoconstriction. In a phase 3 study, patients reporting being free of headache after two hours with lasmiditan 200 mg (32.2%) or 100 mg (28.2%) compared with placebo (15.3%). Patients who received lasmiditan were also significantly more likely to report alleviation of their most bothersome symptom compared with placebo [215]. Adverse events were mostly mild or moderate in intensity.
In some patients, the frequency, severity, and unresponsiveness of migraine attacks to abortive medications require the initiation of preventive therapy. In patients with repeated acute attacks, the overuse of medications—opioids and barbiturates in particular—may lead to migraine chronification [9,216].
Preventive pharmacotherapy is used in conjunction with effective nonpharmacologic approaches as part of a comprehensive plan including avoidance of migraine triggers, implementation of lifestyle changes, stress management techniques, and a reduction in the use of analgesics or acute migraine medications [217]. Patients with migraine should be considered for preventive treatment in any of the following situations [218,219,220]:
Use abortive medications at least two times per week with limited effectiveness
Frequent attacks (i.e., four or more per month)
Attacks significantly interfere with daily routines despite abortive treatment
Have adverse effects with abortive treatment
Have migraine attacks with serious and unusual symptoms
Have an established pattern of medication overuse
Preventive medications improve patients' quality of life and health outcomes and reduce disability and healthcare costs [221,222]. The decision to opt for preventive pharmacotherapy should be discussed with the patient and should take into consideration the variability in patient response and the possibility of significant side effects [222].
In 2018, the first medications in a novel class of drugs received FDA-approval for the prevention of migraine [81,82,83,84]. As previously noted, CGRP is a potent vasodilatory neuropeptide that increases blood flow in the meningeal arteries [77]. It has long been postulated that one cause of episodic migraine is a combination of neuronal hyperactivity and a local process of neurogenic inflammation triggered by an increase in pro-inflammatory mediators such as CGRP, neurokinin, and substance P [31,33]. Following the development of a monoclonal antibody that blocks the activity of the CGRP peptide, a significant reduction in days with migraine was shown in clinical trials with CGRP antagonists [82,223,224,225].
The first of three clinical trials prior to FDA-approval showed that six months of treatment with erenumab-aaoe resulted in one to two fewer monthly migraine days on average than those on placebo among 955 patients. A second study of 577 patients with episodic migraine showed one fewer migraine day over the course of three months. A third study of 677 patients with chronic migraine showed 2.5 fewer monthly migraine days after three months of treatment [82,223]. Erenumab-aaoe is recommended for those who do not respond to conventional treatment.
Erenumab-aaoe is initially administered at a dose of 70 mg once-monthly by subcutaneous self-injection, but this can be increased to a maximum of 140 mg once-monthly in divided doses [81]. There are no contraindications to erenumab-aaoe, and known side effects are limited to injection site reactions (less than 6%) and constipation (3%) [81]. Pregnancy and breastfeeding considerations are unknown; however, adverse events were not seen in animal reproduction studies [81].
The results of multiple phase II and phase III clinical trials resulted in additional CGRP antagonists receiving FDA approval in 2018, 2019, and 2020 [224,226]. Like erenumad, fremanezumab-vfrm, galcanezumab, ubrogepant, and eptinezumab-jjmr are administered subcutaneously for prevention of migraine in adults [83,84]. Fremanezumab-vfrm is administered either as a 225-mg monthly dose or 675 mg every three months [83]. The initial dose of galcanezumab is 240 mg, followed by 120-mg monthly doses [84]. Ubregepant is taken orally at a dose of 50–100 mg (maximum in 24 hours: 200 mg) [226]. The initial dose of eptinezumab-jjmr is 100 mg every three months, but it may be titrated up to a maximum of 300 mg every three months.
The precise mechanism of action of drugs used for the conventional prophylactic treatment of migraine is unclear. It has been postulated that these medications prevent the underlying processes that set a migraine attack into motion and raise the threshold for migraine headache.
Initially, treatment should begin with the lowest possible dose, and a trial of at least two medications at the appropriate dosage is typically required before effectiveness can be assessed. If required, the dose should be slowly titrated up until benefits or unacceptable adverse reactions are observed. When possible, long-acting formulations should be used in order improve patient compliance. In addition, selecting medication that may also treat co-existing conditions, such as hypertension or depression, can improve adherence to the treatment plan [227]. One challenging scenario is presented by migraineurs who become less responsive (i.e., tolerant) to preventive migraine medications. This greatly impacts quality of life, and the establishment of an effective treatment plan for these patients requires an understanding of the mechanisms underlying tolerance to migraine therapy [217].
Although preventive treatments do not completely prevent the occurrence of migraines, they do reduce the frequency by at least 50% [222,228]. Evidence-based guidelines regarding drug effectiveness for the prevention of episodic migraine have haven prepared by the American Headache Society and the American Academy of Neurology (AHS/AAN) (Table 2) [95,220,227]. These guidelines categorize the available prophylactic medications according to the level of available evidence. The following oral treatments have established efficacy and should be offered for prevention of migraine: antiepileptic drugs (e.g., divalproex sodium, valproate sodium, topiramate), beta-blockers (e.g., metoprolol, propranolol, timolol), and frovatriptan (for short-term preventive treatment of menstrual migraine). An exception to the use of valproate sodium and topiramate is that, due to risk of birth defects, it should not be prescribed to women of childbearing potential who are not using a reliable method of contraception [220]. Evidence indicates the following treatment options are probably effective and should be considered for prevention: antidepressants (e.g., amitriptyline, venlafaxine), beta-blockers (e.g., atenolol, nadolol), and angiotensin receptor blockers (e.g., cardisartan) [220].
MEDICATIONS USED FOR THE PREVENTION OF EPISODIC MIGRAINE
| Drug Class | Medications and Dose Ranges | |||||
|---|---|---|---|---|---|---|
| Level A: Established as effective, should be offered to patients requiring migraine prophylaxis | ||||||
| Anticonvulsants |
| |||||
| Antihypertensives, beta blockers |
| |||||
| Other | Butterbur (Petasites hybridus) (50–75 mg twice daily) | |||||
| Level B: Probably effective, should be considered for patients requiring migraine prophylaxis | ||||||
| Tricyclic antidepressants | Amitriptyline (25–150 mg/day) | |||||
| Serotonin/norepinephrine reuptake inhibitors | Extended-release venlafaxine (150 mg /day) | |||||
| Nonsteroidal anti-inflammatory drugs (NSAIDs) |
| |||||
| Antihypertensive, beta blockers | Atenolol (100 mg/day) | |||||
| Other |
| |||||
| Level C: Possibly effective, may be considered for patients requiring migraine prophylaxis | ||||||
| Antihypertensive, angiotensin II receptor blockers (ARBs) | Candesartan (16 mg/day) | |||||
| Antihypertensive, angiotensin-converting enzyme (ACE) inhibitors | Lisinopril (10–20 mg/day) | |||||
| Anticonvulsants | Carbamazepine (600 mg/day) | |||||
| Antihypertensive, alpha-2 agonists |
| |||||
| Antihypertensive, beta blocker partial agonists | Pindolol 10 (mg/day) | |||||
| Antihypertensive, selective beta-1 blockers | Nebivolol (5 mg/day) | |||||
| NSAIDs |
| |||||
| Antihistamine, H1 antagonists | Cyproheptadine (4 mg/day) | |||||
| Other | Coenzyme Q10 (100 mg three times daily) | |||||
| aApproved by the FDA for prophylactic treatment of migraine. | ||||||
Caution is required when NSAIDs are used for preventive therapy, as their use is associated with induction of medication-overuse headache and chronification of migraine [222]. Although the Canadian Headache Society guideline for migraine prophylaxis recommends the use of the anticonvulsant gabapentin, this is not supported by a 2015 Cochrane review or a 2016 review of literature, which confirmed the effectiveness of topiramate, divalproex, and sodium valproate, but concluded that the evidence was insufficient to support the use of gabapentin [185,230,231]. Extended-release topiramate is contraindicated in patients with metabolic acidosis taking metformin, during pregnancy, in women of childbearing age not using contraception, and in patients with recent alcohol use (within six hours prior or six hours following administration). Divalproex and sodium valproate are contraindicated in patients with impaired liver function, urea cycle disorders, and pregnant women (for the prevention of migrane) [81].
For the prevention of menstrual migraines, the AHS/AAN recommend frovatriptan (2.5 mg twice daily perimenstrually, following a loading dose), naratriptan (1 mg twice daily perimenstrually for five days), or zolmitriptan (2.5 mg two or three times per day perimenstrually). It should be noted, however, that the FDA did not feel evidence for triptans, including frovatriptan, was sufficient to approve these medications for prevention of migraine [95,227,232]. The AHS recommends an NSAID (such as naproxen 550 mg) twice-daily for five to seven days surrounding the menstrual window, estrogen supplementation of 1 mg per day during menstruation, and magnesium supplementation 15 days from the start of menses until menses begins [232].
Up to 10% of migraine sufferers become less responsive to preventive migraine medications. A variety of mechanisms have been implicated in tolerance, including pharmacokinetic (e.g., metabolic, drug-drug interactions), pharmacodynamic (e.g., receptor down-regulation), behavioral (e.g., unconscious adaptations), drug-induced disease progression (e.g., medication overuse, opioid abuse), and natural variability of migraine factors [233]. For these patients, a review of therapy compliance, drug quality and delivery, and environmental aggravating factors is the effective first step. Drug dosages should be adjusted or patients may be switched to an alternative medication. An effort should be made to identify and manage environmental and lifestyle triggers (e.g., sleep patterns, smoking, excess caffeine). Patients may benefit from a drug holiday of two to three months to obtain accurate baseline information and compare treatment effects.
Research has provided a better understanding of the pathophysiology of migraine, and effective translational medicine is beginning to lead to the availability of new drugs.
As previously noted, gap junction channels appear to be involved in several ways in the pathophysiology of migraine, although limited research has been conducted on gap junction blockers in the prevention or treatment of migraine and results have been conflicting. Clinical studies have shown that efficacy for the gap junction blocker tonabersat remains unclear [60,234,235].
Occipital nerve stimulation has been found to be effective in the treatment of medication-resistant chronic migraine. The European Headache Federation recommends the use of this modality after all alternative drug and behavioral therapies have failed [236].
In 2013, the FDA approved a device using transcranial magnetic stimulation (TMS) technology for use when a patient with migraine feels a headache or migraine coming on or when the pain begins. This device is held to the back of head with both hands and a button is quickly pressed and released, sending a magnetic pulse to stimulate the brain's occipital cortex. This is the only device that has received FDA approval to treat migraine with aura [237].
In 2014, the FDA approved the first transcutaneous electrical nerve stimulation (TENS) device as an alternative to medication for migraine prevention [237]. This approach consists of a small, portable, battery-powered, prescription device that resembles a plastic headband worn across the forehead. The patient positions the device in the center of the forehead, just above the eyes, using a self-adhesive electrode. The device applies an electric current to stimulate branches of the trigeminal nerve [237]. The TENS device is specifically authorized to be used prior to the onset of headache in patients with a history of chronic migraine.
Migraine in children and adolescents is relatively common and potentially disabling. It may be more prevalent than data from national health surveys indicate. A systematic review of population-based studies found that the prevalence of migraine is 9.7% in female children and adolescents and 6% in male children and adolescents [238]. Adolescents with migraine are reported to have high levels of disability, low health-related quality of life, and tend to have inferior academic performance as compared to their peers [239]. A Canadian health survey, conducted over multiple time periods and involving 61,000 subjects between 12 and 19 years of age, found a strong and consistent association between migraine and anxiety/mood disorders and perceived mental health in adolescents [239]. The authors recommended screening for symptoms of anxiety and depression in children and adolescents presenting with migraines. According to a review of pediatric clinical studies, the most effective pediatric/adolescent management strategy includes the combination of timely pharmacologic interventions (NSAIDs and/or triptans) for acute attacks combined with education in self-management techniques and biopsychosocial approaches such as biofeedback, relaxation therapy, and cognitive-behavioral therapy [240].
In 2019, the AAN and the AHS published practice guidelines for treatment of acute migraine in children and adolescents [241]. Ibuprofen oral solution (10 mg/kg) is the initial treatment option recommended to reduce pain and is more likely to be effective when administered early, within one hour of headache onset. The efficacy of triptans is less well established, and triptans are less commonly prescribed in children than in adults. Four triptans have been approved by the FDA for treatment of migraine in adolescents (12 to 17 years of age): sumatriptan/naproxen, almotriptan, rizatriptan, and zolmitriptan. When response to a triptan is less than satisfactory, ibuprofen or naproxen in combination should be offered to improve migraine relief. It is important to counsel patients and families on the cumulative duration limits of NSAID and triptan use to avoid adverse effects and overuse headache. AAN/AHS guidelines recommend that ibuprofen or acetaminophen use be limited to no more than 14 days per month, and triptan use limited to no more than 9 days per month [239]. Ergots and naproxen for acute migraine have not been studied in children [240].
The FDA has certified a remote electrical neuromodulation (REN) device for the acute and/or preventive treatment of migraine in patients 12 years of age or older. The REN is a nonpharmacologic, prescribed, wearable device [241]. A group of 83 adolescents were analyzed to determine whether frequent use of the REN resulted in a reduction in monthly migraine treatment days. The participants used the REN on at least 10 days per month, following the REN migraine prevention guideline of an every-other-day pattern. Results demonstrated a substantial month-to-month reduction in the mean number of REN treatment days from 12.6 days in the first month, to 9.0 days in the second month, to 7.4 days in the third month. Additionally, 61.9% of users reported experiencing pain relief, 24.% reported freedom from pain, 67.4% reported relief in functional disability, and 41.3% reported complete freedom from functional disability [241].
As a result of the evolving demographics in the United States, interaction with patients for whom English is not a native language is inevitable. Because patient history is such a vital aspect of the assessment of migraine, it is each practitioner's responsibility to ensure that information and instructions are explained in such a way that allows for patient understanding. In this multicultural landscape, interpreters are a valuable resource to help bridge the communication and cultural gap between clients/patients and practitioners. Interpreters are more than passive agents who translate and transmit information back and forth from party to party. When they are enlisted and treated as part of the interdisciplinary clinical team, they serve as cultural brokers, who ultimately enhance the clinical encounter. In any case in which information regarding diagnostic procedures, treatment options, and medication/treatment measures is being provided, the use of an interpreter should be considered.
Migraine is a complex and multifaceted condition that requires an appropriate evaluation, detailed medical history, and neurologic examination. Other primary and secondary causes of headache should be considered in the clinical evaluation in order to ensure the correct diagnosis. After the diagnosis of migraine is established, an individualized management strategy should be crafted using the combination of nonpharmacologic, pharmacologic, and patient education interventions. Optimization of therapy for either abortive or prophylactic management of acute or chronic migraine is required, and interprofessional collaboration between primary care providers and specialists is necessary to effectively treat patients with challenging migraines.
| American Academy of Neurology |
| https://www.aan.com |
| American Migraine Foundation |
| https://americanmigrainefoundation.org |
| National Institute of Neurological Disorders and Stroke (NINDS) |
| https://www.ninds.nih.gov |
| American Headache Society |
| https://americanheadachesociety.org |
| European Headache Federation |
| https://ehf-org.org |
| Migraine Research Foundation |
| https://migraineresearchfoundation.org |
1. Borgdorff P. Arguments against the role of cortical spreading depression in migraine.Neurol Res. 2018;40(3):173-181.
2. Steiner TJ, Stovner LJ, Vos T. GBD 2015: migraine is the third cause of disability in under 50s. J Headache and Pain. 2016;17(1):104.
3. Centers for Disease Control and Prevention. Health, United States, 2015: With Special Feature on Racial and Ethnic Disparities. Available at https://www.cdc.gov/nchs/data/hus/hus15.pdf. Last accessed June 20, 2024.
5. Stovner LJ, Hagen K, Jensen R, et al. The global burden of headache: a documentation of headache prevalence and disability worldwide. Cephalalgia. 2007;27(3):193-210.
6. National Center for Health Statistics. National Hospital Ambulatory Medical Care Survey: 2021 Emergency Department Summary Tables. Available at https://www.cdc.gov/nchs/data/nhamcs/web_tables/2021-nhamcs-ed-web-tables-508.pdf. Last accessed June 20, 2024.
7. IHS Classification ICHD-3. The International Classification of Headache Disorders, 3rd Edition. Available at https://ichd-3.org. Last accessed June 20, 2024.
9. Headache Classification Committee of the International Headache Society. The International Classification of Headache Disorders, 3rd edition. Cephalalgia. 2018;38(1):1-211.
10. Lipton RB, Bigal ME, Steiner TJ, Silberstein SD, Olesen J. Classification of primary headaches. Neurology. 2004;63(3):427-435.
11. Crosby SJ. Headache. In: Zeind CS, Carvalho MG (eds). Applied Therapeutics: The Clinical Use of Drugs. 11th ed. Philadelphia, PA: Lippincott Williams & Wilkins; 2018: 1233-1245.
12. Schwedt TJ. Thunderclap headaches: a focus on etiology and diagnostic evaluation. Headache. 2013;53(3):563-569.
13. Edlow JA, Panagos PD, Godwin SA, Thomas TL, Decker WW. Clinical policy: critical issues in the evaluation and management of adult patients presenting to the emergency department with acute headache. Ann Emerg Med. 2008;52(4):407-436.
14. Savitz SI, Levitan EB, Wears R., Edlow JA. Pooled analysis of patients with thunderclap headache evaluated by CT and LP: is angiography necessary in patients with negative evaluations? J Neurol Sci. 2009;276(1-2):123-125.
15. Halker RB, Vargas BB. Primary exertional headache: updates in the literature. Curr Pain Headache Rep. 2013;17(6):1-4.
16. Burch R, Rizzoli P, Loder E. The prevalence and impact of migraine and severe headache in the United States: updated age, sex, and socioeconomic-specific estimates from government health surveys. Headache. 2021;61:60-68.
17. Hershey A. Current approaches to the diagnosis and management of paediatric migraine. Lancet Neurol. 2010;9(2):120-204.
18. Winner P. Epidemiology of pediatric headache. In: Hershey AD, Powers SW, Winner P, Kabouche M (eds). Pediatric Headaches in Clinical Practice. Chichester: John Wiley & Sons, Ltd.; 2009: 31-39.
19. Fuh JL, Wang SJ, Lu SR, Liao YC, Chen SP, Yang CY. Headache disability among adolescents: a student population-based study. Headache. 2010;50(2):210-218.
20. Lipton RB, Stewart WF, Diamond S, Diamond ML, Reed M. Prevalence and burden of migraine in the United States: data from the American Migraine Study II. Headache. 2001;41(7):646-657.
21. Lipton RB, Bigal ME, Diamond M, et al. Migraine prevalence, disease burden, and need for preventive therapy. Neurology. 2007;68(5):343-349.
22. Global Health Data Exchange. Global Burden of Disease Study 2021 (GBD 2021) Data Resources. Available at https://ghdx.healthdata.org/gbd-2021. Last accessed June 20, 2024.
23. World Health Organization. Lifting the Burden: Atlas of Headache Disorders and Resources in the World, 2011. Available at https://www.who.int/publications/i/item/9789241564212. Last accessed June 20, 2024.
24. Natoli JL, Manack A, Dean B, et al. Global prevalence of chronic migraine: a systematic review. Cephalalgia. 2010;30(5):599-609.
25. Scher AI, Stewart WF, Ricci JA, Lipton RB. Factors associated with the onset and remission of chronic daily headache in a population-based study. Pain. 2003;106(1-2):81-89.
26. Buse DC, Manack AN, Fanning KM, et al. Chronic migraine prevalence, disability, and sociodemographic factors: results from the American Migraine Prevalence and Prevention Study. Headache. 2012;52(10):1456-1470.
27. Manack A, Buse DC, Serrano D, Turkel CC, Lipton RB. Rates, predictors, and consequences of remission from chronic migraine to episodic migraine. Neurology. 2011;76(8):711-718.
28. Headache Classification Committee, Olesen J, Bousser MG, et al. New appendix criteria open for a broader concept of chronic migraine. Cephalalgia. 2006;26(6):742-746.
29. Diener HC, Dodick DW, Goadsby PJ, Lipton RB, Olesen J, Silberstein SD. Chronic migraine: classification, characteristics and treatment. Nat Rev Neurol. 2012;8(3):162-171.
32. De Hoon JNJM. Migraine and Antimigraine Drugs: Focus on Cardiovascular Aspects [Dissertation]. Maastricht: University of Maastricht; 2000.
33. Chapman LF, Ramos AO, Goodell H, Silverman G, Wolff HG. A humoral agent implicated in vascular headache of the migraine type. Arch Neurol. 1960;3:223-229.
34. Bernstein C, Burstein R. Sensitization of the trigeminovascular pathway: perspective and implications to migraine pathophysiology. J Clin Neurol. 2012;8(2):89-99.
35. Sicuteri F, Renzi D, Geppetti P. Substance P and enkephalins: a creditable tandem in the pathophysiology of cluster headache and migraine. Adv Exp Med Biol. 1986;198(Pt B):145-152.
36. Akerman S, Holland PR, Goadsby PJ. Diencephalic and brainstem mechanisms in migraine. Nat Rev Neurosci. 2011;12(10):570-584.
37. Messlinger K, Fischer MJM, Lennerz JK. Neuropeptide effects in the trigeminal system: pathophysiology and clinical relevance in migraine. Keio J Med. 2011;60(3):82-89.
39. Olesen J, Ashina M. Emerging migraine treatments and drug targets. Trends Pharmacol Sci. 2011;32(6):352-359.
40. Charles A, Brennan KC. Cortical spreading depression: new insights and persistent questions. Cephalalgia. 2009;29(10):1115-1124.
41. Eikermann-Haerter K, Ayata C. Cortical spreading depression and migraine. Curr Neurol Neurosci Rep. 2010;10(3):167-173.
43. Bolay H, Reuter U, Dunn AK, Huang Z, Boas DA, Moskowitz MA. Intrinsic brain activity triggers trigeminal meningeal afferents in a migraine model. Nat Med. 2002;8(2):136-142.
44. Kowa H, Takigawa H, Nakashima K. Cortical spreading depression and pain: a missing link in the pathophysiology of migraine? Rinsho Shinkeigaku. 2014;54(12):1006-1008.
45. Bowyer SM, Aurora KS, Moran JE, Tepley N, Welch KM. Magnetoencephalographic fields from patients with spontaneous and induced migraine aura. Ann Neurol. 2001;50(5):582-587.
46. D'Esposito M, Deouell LY, Gazzaley A. Alterations in the BOLD fMRI signal with ageing and disease: a challenge for neuroimaging. Nat Rev Neurosci. 2003;4(11):863-872.
47. Woods RP, Iacobini M, Mazziotta JC. Brief report: bilateral spreading cerebral hypoperfusion during spontaneous migraine headache. N Engl J Med. 1994;331(25):1689-1692.
48. Lauritzen M, Dreier JP, Fabricius M, Hartings JA, Graf R, Strong AJ. Clinical relevance of cortical spreading depression in neurological disorders: migraine, malignant stroke, subarachnoid and intracranial hemorrhage, and traumatic brain injury. J Cereb Blood Flow Metab. 2011;31(1):17-35.
49. Goadsby PJ, Charbit AR, Anreou AP, Akerman S, Holland PR. Neurobiology of migraine. Neuroscience. 2009;161(2):327-341.
50. Goadsby PJ, Raskin NH. Headache. In: Jameson J, Fauci A, Kasper D, Hauser S, Longo D, Loscalzo J (eds). Harrison's Principles of Internal Medicine. 20th ed. McGrawHill; New York, NY: 2018.
51. Holland PR. Modulation of trigeminaovascular processing: novel insights into primary headache disorders. Cephalalgia. 2009:29(Suppl 3):1-6.
52. Alonso AA, Nixdorf DR. Case studies of four different headache types presenting as tooth pain. J Endod. 2006;32(11):1110-1113.
53. Cady RK, Schreiber CP. Sinus problems as a cause of headache refractoriness and migraine chronification. Curr Pain Headache Rep. 2009;13(4):319-325.
54. Eross E, Dodick D, Eross M. The sinus, allergy and migraine study (SAMS). Headache. 2007;47(2);213-224.
55. Obermann M, Mueller D, Yoon M-S, Pageler L, Diener HC, Katsarava Z. Migraine with isolated facial pain: a diagnostic challenge. Cephalalgia. 2007;27(11):1278-1282.
56. Hegarty AM, Zakrzewska JM. Differential diagnosis for orofacial pain, including sinusitis, TMD, and trigeminal neuralgia. Dent Update. 2011;38(6):396-408.
57. Lança AJ. Functional and neurochemical organization of the central nervous system. In: Kalant H, Grant DM, Mitchell J (eds). Principles of Medical Pharmacology. 7th ed. Toronto: Elsevier; 2007: 187-210.
58. Haydon PG, Carmignoto G. Astrocyte control of synaptic transmission and neurovascular coupling. Physiol Rev. 2006;86(3):1009-1031.
59. Sarrouilhe D, Dejean C, Mesnil M. Involvement of gap junction channels in the pathophysiology of migraine with aura. Front Physiol. 2014;5:78.
60. Silberstein SD. Tonabersat, a novel gap-junction modulator for the prevention of migraine. Cephalalgia. 2009;29(Suppl 2):28-35.
61. Goadsby PJ, Ferrari MD, Csanyi A, Olesen J, Mills JG; Tonabersat TON-01-05 Study Group. Randomized, double-blind, placebo-controlled, proof-of-concept study of the cortical spreading depression inhibiting agent tonabersat in migraine prophylaxis. Cephalalgia. 2009;29(7):742-750.
62. Catterall WA, Dib-Hajj S, Meisler MH, Pietrobon D. Inherited neuronal ion channelopathies: new windows on complex neurological diseases. J Neurosci. 2008;28(46):11768-11777.
63. Rogawski MA. Common patholophysiologic mechanisms in migraine and epilepsy. Arch Neurol. 2008;65(6):709-714.
64. Waxman SG. Channel, neuronal and clinical function in sodium channelopathies: from genotype to phenotype. Nat Neurosci. 2007;10(4):405-409.
65. Mantegazza M, Curia G, Biagini G, Ragsdale DS, Avoli M. Voltage-gated sodium channels as therapeutic targets in epilepsy and other neurological disorders. Lancet Neurol. 2010;9(4):413-424.
66. Hamel E. Serotonin and migraine: biology and clinical implications. Cephalalgia. 2007;27(11):1295-1300.
67. Schwedt TJ. Serotonin and migraine: the latest developments. Cephalalgia. 2007;27(11):1301-1307.
68. Barra S, Lanero S, Materazzi C, Vitagliano G, Ames PR, Gaeta G. Sumatriptan therapy for headache and myocardial infarction. Expert Opin Pharmacother. 2010;11(16):2727-2737.
69. Gupta S, Nahas SJ, Peterlin BL. Chemical mediators of migraine: preclinical and clinical observations. Headache. 2011;51(6):1029-1045.
70. Marmura MJ, Silberstein SD. Current understanding and treatment of headache disorders: five new things. Neurology. 2011;76(7 Suppl 2):S31-S36.
71. Schürks M. Genetics of migraine in the age of genome-wide association studies. J Headache Pain. 2012;13(1):1-9.
72. Sicuteri F. Dopamine, the second putative protagonist in headache. Headache. 1977;17(3):129-131.
73. Akerman S, Goadsby PJ. Dopamine and migraine: biology and clinical implications. Cephalalgia. 2007;27(11):1308-1314.
74. Minor DS, Harrell TK. Headache disorders. In: DiPiro JT, Talbert RL, Yee GC, Matzke GR, Wells BG, Posey LM (eds). Pharmacotherapy: A Pathophysiologic Approach. 10th ed. New York, NY: McGraw-Hill; 2017: 927-942.
76. Villalon CM, Olesen J. The role of CGTP in the pathophysiology of migraine and efficacy of CGRP receptor antagonists as acute migraine drugs. Pharmacol Ther. 2009;124(3):309-323.
77. Sprenger T, Goadsby PJ. Migraine pathogenesis and state of pharmacological treatment options. BMC Medicine. 2009;7:71.
78. Farinelli I, De Filippis S, Coloprisco G, Missori S, Martelletti P. Future drugs for migraine. Intern Emerg Med. 2009;4(5):367-373.
79. Ho TW, Ferrari MD, Dodick DW, et al. Efficacy and tolerability of MK-0974 (telcagepant), a new oral antagonist of calcitonin gene-related peptide receptor, compared with zolmitriptan for acute migraine: a randomised, placebo-controlled, parallel-treatment trial. Lancet. 2008;372(9656):2115-2123.
80. Lexicomp Online. Available at http://online.lexi.com. Last accessed June 20, 2024.
81. U.S. Food and Drug Administration. FDA Approves Novel Preventive Treatment for Migraine. Available at https://www.fda.gov/news-events/press-announcements/fda-approves-novel-preventive-treatment-migraine. Last accessed June 20, 2024.
82. U.S. Food and Drug Administration. Highlights of Prescribing Information: Ajovy (Fremanezumab-vfrm). Available at https://www.accessdata.fda.gov/drugsatfda_docs/label/2018/761089s000lbl.pdf. Last accessed June 20, 2024.
83. U.S. Food and Drug Administration. Highlights of Prescribing Information: Emgality (Galcanezumab-gnlm). Available at https://www.accessdata.fda.gov/drugsatfda_docs/label/2018/761063s000lbl.pdf. Last accessed June 20, 2024.
84. Biscaldi L. FDA Approves Expanded Indication for Atogepant for prevention of Chronic Migraine. Available at https://www.drugtopics.com/view/fda-approves-expanded-indication-for-atogepant-for-prevention-of-chronic-migraine. Last accessed June 20, 2024.
85. U.S. Food and Drug Administration. Highlights of Prescribing Information: Qulipta. Available at https://www.accessdata.fda.gov/drugsatfda_docs/label/2021/215206Orig1s000lbl.pdf. Last accessed June 20, 2024.
86. American Headache Society. NURTEC ODT (Rimegepant) Receives Additional Approval for Preventive Treatment for Adult Patients with Episodic Migraine. Available at https://americanheadachesociety.org/news/nurtec-odt-rimegepant-receives-additional-approval-for-preventive-treatment-for-adult-patients-with-episodic-migraine/. Last accessed June 20, 2024.
88. Pradhan AA, Bertels Z, Akerman S. Targeted nitric oxide synthase inhibitors for migraine. Neurotherapeutics. 2018;15(2):391-401.
89. Sacco S, Ricci S, Degan D, Carolei A. Migraine in women: the role of hormones and their impact on vascular diseases. J Headache Pain. 2012;13(3):177-189.
90. Curtis KM, Tepper NK, Jatlaoui TC, et al. U.S. medical eligibility criteria for contraceptive use, 2016. MMWR. 2016;65(RR-3):1-104.
91. Calhoun AH, Batur P. Combined hormonal contraceptives and migraine: an update on the evidence. Clev Clin J Med. 2017;84(8):631-638.
92. Bousser MG, Conard J, Kittner S, et al. Recommendations on the risk of ischaemic stroke associated with use of combined oral contraceptives and hormone replacement therapy in women with migraine: the International Headache Society Task Force on combined oral contraceptives and hormone replacement therapy. Cephalalgia. 2000;20(3):155-156.
93. ACOG Committee on Practice Bulletins. ACOG practice bulletin no. 73: use of hormonal contraception in women with coexisting medical conditions. Obstet Gynecol. 2006;107(6):1453-1472.
94. Holland S, Silberstein SD, Freitag F, et al. Evidence-based guideline update: NSAIDs and other complementary treatments for episodic migraine prevention in adults [RETIRED]: report of the Quality Standards Subcommittee of the American Academy of Neurology and the American Headache Society. Neurology. 2012;78(17):1346-1353.
95. de Vries B, Frants RR, Ferrari MD, van den Maagdenberg AM. Molecular genetics of migraine. Hum Genet. 2009;126(1):115-132.
96. Barrett CF, van den Maagdenberg AM, Frants RR, Ferrari MD. Familial hemiplegic migraine. Adv Genet. 2008;63:57-83.
99. Mulder EJ, Van Baal C, Gaist D, et al. Genetic and enviormental influences on migraine: a twin study across six countries. Twin Res. 2003;6(5):422-431.
100. Svennsson DA, Larsson B, Walsenlind E, Pedersen NL. Shared rearing enviroment in migraine: results from twins reared apart and twins reared together. Headache. 2003;43(3):235-244.
101. Bigal M, Rapoport A, Sheftell F, Tepper D, Tepper S. Memantine in the preventive treatment of refractory migraine. Headache. 2008;48(9):1337-1342.
102. Charles A, Flippen C, Romero-Reyes M, Brennan KC. Memantine for prevention of migraine: a retrospective study of 60 cases.J Headache Pain. 2007;8(4):248-250.
103. Todt U, Netzer C, Toliat M, et al. New genetic evidence for involvement of the dopamine system in migraine with aura. Hum Genet. 2009;125(3):265-279.
104. Kelley NE, Tepper DE. Rescue therapy for acute migraine. Part 2: neuroleptics, antihistamines, and others. Headache. 2012;52(2):292-306.
105. Saguil A, Lax JW. Acute migraine treatment in emergency settings. Am Fam Physician. 2014;89(9):742-744.
106. Gilmore B, Michael M. Treatment of acute migraine headache. Am Fam Physician. 2011;83(3):271-280.
107. Laine C, Goldmann D, Wilson JF. In the clinic: migraine. Ann Intern Med. 2007;147(5):ITC11-1-ITC11-16.
108. Cady RK, Farmer K. Migraine. In: Jay GW (ed). Clinician's Guide to Chronic Headache and Facial Pain. New York, NY: Informa Healthcare USA; 2010: 1-15.
109. Schürks M, Rist PM, Bigal ME, Buring JE, Lipton RB, Kurth T. Migraine and cardiovascular disease: systematic review and meta-analysis. BMJ. 2009;339:b3914.
110. Kurth T, Gaziano JM, Cook NR, Logroscino G, Diener HC, Buring JE. Migraine and risk of cardiovascular disease in women. JAMA. 2006;296(3):283-291.
111. Selby G, Lance JW. Observations on 500 cases of migraine and allied vascular headache. J Neurol Neurosurg Psychiatry. 1960;23(1):23-32.
112. Crawford P, Simmons M, Hoock J. What dietary modifications are indicated for migraines? J Fam Pract. 2006;55(1):62-63.
114. Cutrer FM, Bajwa ZH, Sabahat A. Pathophysiology, clinical manifestations, and diagnosis of migraine in adults. UptoDate. 2012;17(3):1-23.
115. Sprenger T, Borsook D. Migraine changes the brain: neuroimaging makes its mark. Curr Opin Neurol. 2012;25(3):252-262.
118. Granziera C, DaSilva AF, Snyder J, Tuch DS, Hadjikhani N. Anatomical alterations of the visual motion processing network in migraine with and without aura. PLoS Med. 2006;3(10):e402.
119. May A, Matharu M. New insights into migraine: application of functional and structural imaging. Curr Opin Neurol. 2007;20(3):306-309.
120. Moschiano F, D'Amico D, Di Stefano M, Rocca N, Bussone G. The role of the clinician in interpreting conventional neuroimaging findings in migraine patients. Neurol Sci. 2007;28(Suppl 2):S114-S117.
121. Lakhan SE, Avramut M. Structural and functional neuroimaging in migraine: insight from three decades of research. Headache. 2013;53(1):46-66.
123. Sudlow C. US guidelines on neuroimaging in patients with non-acute headache: a commentary. J Neurol Neurosurg Psychiatry. 2002;72(Suppl II):ii16-ii18.
124. Detsky ME, McDonald DR, Baerlocher MO, Tomlinson GA, McCrory DC, Booth CM. Does this patient with headache have a migraine or need neuroimaging? JAMA. 2006;296(10):1274-1283.
125. Dahlöf C, Maassen Van Den Brink A. Dihydroergotamine, ergotamine, methysergide and sumatriptan: basic science in relation to migraine treatment. Headache. 2012;52(4):707-714.
126. Lipton RB, Diamond S, Reed M, Diamond ML, Stewart WF. Migraine diagnosis and treatment: results from the American Migraine Study II. Headache. 2001;41(7):638-645.
127. Cooke LJ, Becker WJ. Migraine prevalence, treatment and impact: the Canadian Women Migraine Study. Can J Neurol Sci. 2010;37(5):580-587.
128. Bigal ME, Ferrari M, Silberstein SD, Lipton RB, Goadsby PJ. Migraine in the triptan era: lessons from epidemiology, pathophysiology, and clinical science. Headache. 2009;49(Suppl 1):S21-S33.
129. Bigal ME. Migraine, lipid profile, and cardiovascular disease. Eur J Neurol. 2010;17(3):342-343.
130. Bond DS, Roth J, Nash JM, Wing RR. Migraine and obesity: epidemiology, possible mechanisms and the potential role of weight loss treatment. Obes Rev. 2011;12(5):362-371.
131. Gruber H-J, Bernecker C, Pailer S, et al. Lipid profile in normal weight migraineurs: evidence for cardiovascular risk. Eur J Neurol. 2010:17(3):419-425.
132. Jensen R, Stovner LJ. Epidemiology and comorbidity of headache. Lancet Neurol. 2008;7(4):354-361.
133. Sacco S, Cerone D, Carolei A. Comorbid neuropathologies in migraine: an update on cerebrovascular and cardiovascular aspects.J Headache Pain. 2008;9(4):237-248.
134. Silva IR, Freitas GR. Migraine patients should be cautiously followed for risk factors leading to cardiovascular disease. Arq Neuropsiquiatr. 2013;71(2):119-124.
135. Bushnell C, McCullough LD, Awad IA, et al. Guidelines for the prevention of stroke in women: a statement for healthcare professionals from the American Heart Association/American Stroke Association. Stroke. 2014;45(5):1545-1588.
136. Linde M, Stovner LJ, Zwart JA, Hagen K. Time trends in the prevalence of headache disorders: the Nord-Trondelag Health Studies (HUNT 2 and HUNT 3). Cephalalgia. 2011;31(5):585-596.
137. Matharu MS, Cohen AS, McGonigle DJ, Ward N, Frackowiak RS, Goadsby PJ. Posterior hypthalamic and brainstem activation in hemicrania continua. Headache. 2004;44(8):747-761.
138. Wallasch TM, Angeli A, Kropp P. Outcomes of a headache-specific cross-sectional multidisciplinary treatment program. Headache. 2012;52(7):1094-1105.
139. Edmeads J, Láinez JM, Brandes JL, Schoenen J, Freitag F. Potential of the Migraine Disability Assessment (MIDAS) questionnaire as a public health initiative and in clinical practice. Neurology. 2001;56(6 Suppl 1):S29-S34.
140. Stewart WF, Lipton RB, Dowson AJ, Sawyer J. Development and testing of the Migraine Disability Assessment (MIDAS) questionnaire to assess headache-related disability. Neurology. 2001;56(6 Suppl 1):S20-S28.
142. U.S. Food and Drug Administration. FDA Approves First Treatment for Episodic Cluster Headache that Reduces the Frequency of Attacks. Available at https://www.fda.gov/news-events/press-announcements/fda-approves-first-treatment-episodic-cluster-headache-reduces-frequency-attacks. Last accessed June 20, 2024.
144. Robbins MS, Starling AJ, Pringsheim TM, Becker WJ, Schwedt TJ. Treatment of cluster headache: the American Headache Society evidence-based guidelines. Headache. 2016;56(7):1093-1106.
145. Ferrante E, Tassorelli C, Rossi P, Lisotto C, Nappi G. Focus on the management of thunderclap headache: from nosography to treatment. J Headache Pain. 2011;12(2):251-258.
146. Moukhachen O, Grgurich P. Ischemic and hemorrhagic stroke. In: Zeind CS, Carvalho MG (eds). Applied Therapeutics: The Clinical Use of Drugs. 11th ed. Philadelphia, PA: Lippincott Williams & Wilkins; 2018: 1301-1318.
147. Porter RS (ed). Neurologic disorders. In: Merck Manual of Diagnosis and Therapy. 20th ed. Whitehouse Station, NJ: MerckSharp & Dohme; 2018.
148. Forsyth PA, Posner JB. Headaches in patients with brain tumors: a study of 111 patients. Neurology. 1993;43(9):1678-1683.
149. Israel HA, Scrivani SJ. The interdisciplinary approach to oral, facial and head pain. J Am Dent Assoc. 2000;131(7):919-926.
150. Okeson JP, de Leeuw R. Differential diagnosis of temporomandibular disorders and other orofacial pain disorders. Dent Clin North Am. 2011;55(1):105-120.
151. Romero-Reyes M, Uyanik JM. Orofacial pain management: current perspectives. J Pain Res. 2014;7:99-115.
152. Lipton JA, Ship JA, Larach-Robinson D. Estimated prevalence and distribution of reported orofacial pain in the United States. J Am Dent Assoc. 1993;124(10):115-121.
153. Graff-Radford SB. Facial pain, cervical pain, and headache. Continuum (Minneap Minn). 2012;18(4):869-882.
154. Klausner, JJ. Epidemiology of chronic facial pain: diagnostic usefulness in patient care. J Am Dent Assoc. 1994;125(12):1604-1611.
155. Mitrirattanakul S, Merrill RL. Headache impact in patients with orofacial pain. JADA. 2006;137(9):1267-1274.
156. Lupoli TA, Lockey RF, Temporomandibular dysfunction: an often overlooked cause of chronic headaches. Ann Allergy Asthma Immunol. 2007;99(4):314-318.
157. Germain L. Differential diagnosis of toothache pain. Part 1: odontogenic etiologies. Dent Today. 2012;31(7):92-97.
158. Nguyen DH, Martin JT. Common dental infections in the primary care setting. Am Fam Physician. 2008;77(6):797-802.
159. American Association of Endodontists. Use and Abuse of Antibiotics. Available at https://www.aae.org/specialty/wp-content/uploads/sites/2/2017/07/ecfewinter12final.pdf. Last accessed June 20, 2024.
160. Simons DG, Travell JG, Simons LS. Travell & Simons' Myofascial Pain and Dysfunction: The Trigger Point Manual. 2nd ed. Baltimore, MD: Williams & Wilkins; 1999.
161. Koratkar H, Parashar V, Koratkar S. A review of neuropathic pain conditions affecting teeth. Gen Dent. 2010;58(5):436-441.
162. Marbach JJ, Raphael KG. Phantom tooth pain: a new look at an old dilemma. Pain Med. 2000;1(1):68-77.
163. Germain L. Differential diagnosis of toothache pain. Part 2: nonodontogenic etiologies. Dent Today. 2012;31(8):84-89.
164. Clark GT. Persistent orodental pain, atypical odontalgia, and phantom tooth pain: when are they neuropathic disorders? J Calif Dent Assoc. 2006;34(8):599-609.
165. Hersh EV, Balasubramaniam R, Pinto A. Pharmacologic management of temporomandibular disorders. Oral Maxillofac Surg Clin North Am. 2008;20(2):197-210.
166. Smith PF, Epstein JB. Orofacial pain. In: Davies AN, Epstein JB (eds). Oral Complications of Cancer and Its Management. Oxford: Oxford University Press; 2010: 241-251.
168. Scully C. Oral and Maxillofacial Medicine: The Basis of Diagnosis and Treatment. 3rd ed. Edinburgh: Churchill Livingstone; 2013: 125-135.
169. Williams JW, Simel DL. Does this patient have sinusitis? Diagnosing sinusitis by history and physical examination. JAMA. 1993;270:1242-1246.
171. Kamani T, Jones NS. 12 minute consultation: evidence based management of a patient with facial pain. Clin Otolaryngol. 2012;37(3):207-212.
172. Patel ZM, Kennedy DW, Setzen M, Poetker DM, DelGaudio JM. "Sinus headache:" rhinogenic headache or migraine? An evidence-based guide to diagnosis and treatment. Int Forum Allergy Rhinol. 2013;3(3):221-230.
173. Bamford CC, Mays M, Tepper SJ. Unusual headaches in the elderly. Curr Pain Headache Rep. 2011;15(4):295-301.
174. Langford CA, Fauci AS. The vasculitis syndromes. In: Jameson J, Fauci A, Kasper D, Hauser S, Longo D, Loscalzo J (eds). Harrison's Principles of Internal Medicine. 20th ed. New York, NY: McGraw-Hill: 2018.
175. Reiter S, Winocur E, Goldsmith C, Emodi-Perlman A, Gorsky M. Giant cell arteritis misdiagnosed as temporomandibular disorder: a case report and review of the literature. J Orofac Pain. 2009;23(4):360-365.
176. Zborowska B, Ell J, McGhee-Collett M, Scolyer R, McCluskey PJ. Progressive visual loss in a patient with presumed temporal arteritis despite treatment: how to make the diagnosis. Clin Experiment Ophthalmol. 2004;32(3):335-336.
177. Durso SC. Oral manifestations of disease. In: Longo D, Fauci A, Kasper D, Hauser S, Jameson J, Loscalzo J (eds). Harrison's Principles of Internal Medicine. 20th ed. New York, NY: McGraw-Hill; 2018.
179. McMillan R, Forssell H, Buchanan JA, Glenny AM, Weldon JC, Zakrzewska JM. Interventions for treating burning mouth syndrome. Cochrane Database Syst Rev. 2016;11:CD002779.
180. American Migraine Foundation. Sleep, Insomnia and Migraine. Available at https://americanmigrainefoundation.org/?articles-cat=migraine-triggers. Last accessed June 20, 2024.
181. Aukerman G, Knutson D, Mise WF. Management of the acute migraine headache. Am Fam Physician. 2002;66(11):2123-2130.
184. Pringsheim T, Davenport W, Mackie G, et al. Canadian Headache Society guideline for migraine prophylaxis. Can J Neurol Sci. 2012;39(2 Suppl 2):S1-S59.
185. Shaik MM, Tan HL, Kamal MA, Gan SH1. Do folate, vitamins B6 and B12 play a role in the pathogenesis of migraine? The role of pharmacoepigenomics. CNS Neurol Disord Drug Targets. 2014;13(5):828-835.
186. Morey SS. Headache Consortium releases guidelines for use of CT or MRI in migraine work-up. Am Fam Physician. 2000;62(7):1699-1701.
187. Marmura MJ, Silberstein SD, Schwedt TJ. The acute treatment of migraine in adults: the American Headache Society evidence assessment of migraine pharmacotherapies. Headache. 2015;55(1):3-20.
188. Chopra R, Robert T, Watson DB. Non-pharmacological and pharmacological prevention of episodic migraine and chronic daily headache. W V Med J. 2012;108(3):88-91.
189. Varkey E, Cider A, Carlsson J, Linde M. Exercise as migraine prophylaxis: a randomized study using relaxation and topiramate as controls. Cephalalgia. 2011;31(14):1428-1438.
190. Kelley NE, Tepper DE. Rescue therapy for acute migraine. Part 1: triptans, dihydroergotamine, and magnesium. Headache. 2012;52(1):114-128.
191. Kelley NE, Tepper DE. Rescue therapy for acute migraine. Part 3: opioids, NSAIDs, steroids, and post-discharge medications. Headache. 2012;52(3):467-482.
192. Valade D. Early treatment of acute migraine: new evidence of benefits. Cephalalgia. 2009;29(Suppl 3):15-21.
193. Robertson CE, Black DF, Swanson JW. Management of migraine headache in the emergency department. Semin Neurol. 2010;30(2):201-212.
194. DeMaagd G. The pharmacological management of migraine. Part 1: overview and abortive therapy. PT. 2008:33(7):404-416.
195. Institute for Clinical Systems Improvement. Diagnosis and Treatment of Headache. Available at https://www.icsi.org/wp-content/uploads/2019/01/Headache.pdf. Last accessed June 20, 2024.
196. Rabbie R, Derry S, Moore RA. Ibuprofen with or without an antiemetic for acute migraine headaches in adults. Cochrane Database Syst Rev. 2013;4:CD008039.
197. Orr SL, Aubé M, Becker WJ, et al. Canadian Headache Society systemic review and recommendations on the treatment of migraine pain in emergency settings. Cephalagia. 2015;35(3):271-284.
198. Taggart E, Doran S, Kokotillo A, Campbell S, Villa-Roel C, Rowe BH. Ketorolac in the treatment of acute migraine: a systematic review. Headache. 2013;53(2):277-287.
200. Sumamo Schellenberg E, Dryden DM, Pasichnyk D, et al. Acute Migraine Treatment in Emergency Settings. Rockville, MD: Agency for Healthcare Research and Quality; 2012.
201. Friedman BW, Cabral L, Adewunmi V, et al. Diphenhydramine as adjuvant therapy for acute migraine: an ED-based randomized clinical trial. Ann Emerg Med. 2016;67(1):32-39.
202. Honkaniemi J, Liimatainen S, Rainesalo S, Sulavuori S. Haloperidol in the acute treatment of migraine: a randomized, double-blind, placebo-controlled study. Headache. 2006;46(5):781-787.
203. Kostic MA, Gutierrez FJ, Rieg TS, Moore TS, Gendron RT. A prospective, randomized trial of intravenous prochlorperazine vs. subcutaneous sumatriptan in acute migraine therapy in the emergency department. Ann Emerg Med. 2010;56(1):1-6.
204. Spielmann K, Kayser A, Beck E, Meister R, Schaefer C. Pregnancy outcome after anti-migraine triptan use: a prospective observational cohort study. Cephalalgia. 2017;38(6):1081-1092.
205. Shahien R, Saleh SA, Bowirrat A. Intravenous sodium valproate aborts migraine headaches rapidly. Acta Neurol Scand. 2011;123(4):257-265.
206. Maizels M, Geiger AM. Intranasal lidocaine for migraine: a randomized trial and open-label follow-up. Headache. 1999;39(8):543-551.
207. Klapper JA, Stanton JS. The emergency treatment of acute migraine headache: a comparison of intravenous dihydroergotamine, dexamethasone and placebo. Cephalalgia. 1991;11(Suppl 11):159-160.
208. Mauskop A, Altura BM. Role of magnesium in the pathogenesis and treatment of migraines. Clin Neurosci. 1998;5(1):24-27.
209. Mauskop A, Altura BT, Cracco RQ, Altura BM. Intravenous magnesium sulphate rapidly alleviates headaches of various types. Headache. 1996;36(3):154-160.
210. Katzung BG. Histamine, serotonin and the ergot alkaloids. In: Katzung BG (ed). Basic and Clinical Pharmacology. 14th ed. New York, NY: McGraw-Hill; 2018: 277-299.
211. Diener HC, Bussone G, de Liano H. Placebo-controlled comparison of effervescent acetylsalicylic acid, sumatriptan, and ibuprofen in the treatment of migraine attacks. Cephalalgia. 2004;24(11):947-954.
212. Ferrari MD, Roon KI, Lipton RB, Goasby PJ. Oral triptans (serotonin 5-HT (1B/1D) agonists) in acute migraine treatment: a meta-analysis of 53 trials. Lancet. 2001;358(9294):1668-1675.
213. Ephross SA, Sinclair SM. Final results from the 16-year Sumatriptan, Naratriptan, and Treximet Pregnancy Registry. Headache. 2014;54(7):1158-1172.
214. Kuca B, Silberstein SD, Wietecha L, et al. Lasmiditan is an effective acute treatment for migraine: a phase 3 randomized study. Neurology. 2018;91(24):e2222-e2232.
216. Loder EW, Rizzoli P. Tolerance and loss of beneficial effect during migraine prophylaxis: clinical considerations. Headache. 2011;51(8):1336-1345.
217. DeMaagd G. The pharmacological management of migraine. Part 2: preventive therapy. PT. 2008:33(8):480-487.
219. AHS Consensus Statement. The American Headache Society Position Statement on Integrating New Migraine Treatments into Clinical Practice. Available at https://headachejournal.onlinelibrary.wiley.com/doi/full/10.1111/head.13456. Last accessed June 20, 2024.
222. Goadsby PJ, Reuter U, Hallstrom Y, et al. A controlled trial of erenumab for episodic migraine. N Engl J Med. 2017;377:2123-2132.
223. Khan S, Olesen A, Ashina M. CGRP, a target for preventive therapy in migraine and cluster headache: systematic review of clinical data. Cephalalgia. 2017.
224. Schuster NM, Rapoport AM. Calcitonin gene-related peptide-targeted therapies for migraine and cluster headache: a review. Clin Neuropharmacol. 2017;40(4):169-174.
225. U.S. Food and Drug Administration. FDA Approves New Treatment for Adults with Migraine. Available at https://www.fda.gov/news-events/press-announcements/fda-approves-new-treatment-adults-migraine. Last accessed June 20, 2024.
226. Silberstein SD, Holland S, Freitag F, et al. Evidence-based guideline update: pharmacologic treatment for episodic migraine prevention in adults: report of the Quality Standards Subcommittee of the American Academy of Neurology and the American Headache Society. Neurology. 2012;78(17):1337-1345.
228. Loder E, Burch R, Rizzoli P. The 2012 AHS/AAN guidelines for prevention of episodic migraine: a summary and comparison with other recent clinical practice guidelines. Headache. 2012;52(6):930-945.
229. Mulleners WM, McCrory DC, Linde M. Antiepileptics in migraine prophylaxis: an updated Cochrane review. Cephalalgia. 2015;35(1):51-62.
230. Perloff MD, Berlin RK, Gillette M, Petersile MJ, Kurowski D. Gabapentin in headache disorders: what is the evidence? Pain Medicine. 2016;17(1):162-171.
231. American Headache Society. Headache Toolbox: Menstrual Migraine. Available at https://americanheadachesociety.org/wp-content/uploads/2018/05/Menstrual-Migraine-Feb-2014.pdf. Last accessed June 20, 2024.
232. Rizzoli P, Loder EW. Tolerance and loss of beneficial effects of prophylactic migraine drugs: a systematic review of causes and mechanisms. Headache. 2011;51(8):1323-1335.
233. Cao Y, Zheng OJ. Tonabersat for migraine prophylaxis: a systematic review. Pain Physician. 2014;17(1):1-8.
234. Sarrouilhe D, Dejean C, Mesnil M. Involvement of gap junction channels in the pathophysiology of migraine with aura. Front Physiol. 2014;5:78.
235. Martelletti P, Jensen RH, Antal A, et al. Neuromodulation of chronic headaches: position statement from the European Headache Federation. J Headache Pain. 2013;14(1):86.
236. U.S. Food and Drug Administration. Treating Migraines: Ways to Fight the Pain with Medication. Available at https://www.fda.gov/consumers/consumer-updates/treating-migraines-ways-fight-pain-medication. Last accessed June 20, 2024.
237. Abu-Arafeh I, Razak S, Silvaraman B, Graham C. Prevalence of headache and migraine in children and adolescents: a systematic review of population-based studies. Dev Med Child Neurol. 2010;52:1088-1097.
238. Orr SL, Potter BK, Ma J, Colman I. Migraine and mental health in a population-based sample of adolescents. Canad J Neurol Sci. 2016;44:44-50.
239. Orr SL, Kabbouche MA, O'Brien HL, et al. Paediatric migraine: evidence-based management and future directions. Nat Rev Neurol. 2018;14:515-527.
240. American Academy of Neurology/American Headache Society. Practice Guideline Update: Acute Treatment of Migraine in Children and Adolescents, August 2019. Available at https://www.aan.com/Guidelines/Home/GuidelineDetail/966. Last accessed June 20, 2024.
1. Douglas AC, Wippold FJ II, Broderick DF, et al. ACR Appropriateness Criteria: Headache. Reston, VA: American College of Radiology; 2022. Available at https://acsearch.acr.org/docs/69482/Narrative. Last accessed June 24, 2024.
2. Beithon J, Gallenberg M, Johnson K, et al. Diagnosis and Treatment of Headache. Bloomington, MN: Institute for Clinical Systems Improvement; 2013. Available at https://www.icsi.org/wp-content/uploads/2019/01/HeadacheRR.pdf. Last accessed June 24, 2024.2023;4:1247313.
Mention of commercial products does not indicate endorsement.