This course is designed to bridge the gap in knowledge of palliative care by providing an overview of the concept of palliative care and a discussion of the benefits and barriers to optimum palliative care at the end of life. Central to this discussion is an emphasis on the importance of talking to patients about the value of palliative care, of clearly presenting the prognosis and appropriate treatment options and goals, and of ensuring that advance planning is completed. The majority of the course focuses on the assessment and management of the most common end-of-life symptoms, with particular attention to pain, the most prevalent, as well as the most distressing, physical symptom. Psychosocial and spiritual needs of the patient and family are also discussed. Palliative care presents unique challenges for some patient populations, most notably older patients, children/adolescents, and patients receiving critical care. An overview of the most important issues specific to these settings is provided.
This course is designed for all members of the interprofessional team, including physicians, physician assistants, nurse practitioners, nurses, pharmacists, pharmacy technicians, social workers, marriage and family therapists, and other members seeking to enhance their knowledge of palliative care.
The purpose of this course is to provide an overview of the concept of palliative care as distinct from hospice care, including a discussion of challenges, benefits, and strategies for optimal palliative care and symptom management at the end of life.
Upon completion of this course, you should be able to:
- Describe how the definition of palliative care has evolved.
- Define the structure of palliative care delivery, including models of care and the interdisciplinary healthcare team.
- List the benefits of palliative care at the end of life.
- Anticipate the barriers to optimum delivery of palliative care through hospice.
- Effectively engage the components of communication and decision making for end-of-life care.
- Identify the common concerns and symptoms at the end of life for patients with life-limiting diseases.
- Discuss the barriers to effective relief of pain at the end of life.
- Assess pain accurately through use of clinical tools and other strategies.
- Select appropriate pharmacologic and/or non- pharmacologic therapies to manage pain in patients during the end-of-life period.
- Assess and manage the most common symptoms (other than pain) experienced by patients during the end-of-life period.
- Evaluate the psychosocial needs of patients at the end of life and their families and provide appropriate treatment or referral.
- Recognize and address the spiritual needs of patients at the end of life and provide appropriate treatment or referral.
- Develop a strategy for providing care to patients and their families over the last days and hours of life.
- Support appropriate grief and mourning.
- Explain the specific challenges and ethical considerations in delivering optimum palliative care to older patients, children, and patients in critical care settings.
John M. Leonard, MD, Professor of Medicine Emeritus, Vanderbilt University School of Medicine, completed his post-graduate clinical training at the Yale and Vanderbilt University Medical Centers before joining the Vanderbilt faculty in 1974. He is a clinician-educator and for many years served as director of residency training and student educational programs for the Vanderbilt University Department of Medicine. Over a career span of 40 years, Dr. Leonard conducted an active practice of general internal medicine and an inpatient consulting practice of infectious diseases.
Contributing faculty, John M. Leonard, MD, has disclosed no relevant financial relationship with any product manufacturer or service provider mentioned.
John V. Jurica, MD, MPH
Mary Franks, MSN, APRN, FNP-C
Alice Yick Flanagan, PhD, MSW
Margaret Donohue, PhD
Randall L. Allen, PharmD
The division planners have disclosed no relevant financial relationship with any product manufacturer or service provider mentioned.
Sarah Campbell
The Director of Development and Academic Affairs has disclosed no relevant financial relationship with any product manufacturer or service provider mentioned.
The purpose of NetCE is to provide challenging curricula to assist healthcare professionals to raise their levels of expertise while fulfilling their continuing education requirements, thereby improving the quality of healthcare.
Our contributing faculty members have taken care to ensure that the information and recommendations are accurate and compatible with the standards generally accepted at the time of publication. The publisher disclaims any liability, loss or damage incurred as a consequence, directly or indirectly, of the use and application of any of the contents. Participants are cautioned about the potential risk of using limited knowledge when integrating new techniques into practice.
It is the policy of NetCE not to accept commercial support. Furthermore, commercial interests are prohibited from distributing or providing access to this activity to learners.
Supported browsers for Windows include Microsoft Internet Explorer 9.0 and up, Mozilla Firefox 3.0 and up, Opera 9.0 and up, and Google Chrome. Supported browsers for Macintosh include Safari, Mozilla Firefox 3.0 and up, Opera 9.0 and up, and Google Chrome. Other operating systems and browsers that include complete implementations of ECMAScript edition 3 and CSS 2.0 may work, but are not supported. Supported browsers must utilize the TLS encryption protocol v1.1 or v1.2 in order to connect to pages that require a secured HTTPS connection. TLS v1.0 is not supported.
The role of implicit biases on healthcare outcomes has become a concern, as there is some evidence that implicit biases contribute to health disparities, professionals' attitudes toward and interactions with patients, quality of care, diagnoses, and treatment decisions. This may produce differences in help-seeking, diagnoses, and ultimately treatments and interventions. Implicit biases may also unwittingly produce professional behaviors, attitudes, and interactions that reduce patients' trust and comfort with their provider, leading to earlier termination of visits and/or reduced adherence and follow-up. Disadvantaged groups are marginalized in the healthcare system and vulnerable on multiple levels; health professionals' implicit biases can further exacerbate these existing disadvantages.
Interventions or strategies designed to reduce implicit bias may be categorized as change-based or control-based. Change-based interventions focus on reducing or changing cognitive associations underlying implicit biases. These interventions might include challenging stereotypes. Conversely, control-based interventions involve reducing the effects of the implicit bias on the individual's behaviors. These strategies include increasing awareness of biased thoughts and responses. The two types of interventions are not mutually exclusive and may be used synergistically.
#97384: Palliative Care and Pain Management at the End of Life
The concept of palliative care has garnered much attention since the term was first used in the late 1960s to refer to a holistic approach to patient-centered care, with a focus on enhancing the quality of life for patients living with serious illness and their families. As currently practiced, palliative care is interdisciplinary team care designed to engage the expertise of providers from different clinical disciplines. The purpose of palliative care is to alleviate suffering and provide comfort; to this end, the primary goals are relief of pain and other distressing symptoms, effective communication with the patient and family in order to establish patient-centered goals of care, attentiveness to psychological and spiritual needs, and support for family members. With its roots in hospice care, the term "palliative care" has long been used interchangeably with "end-of-life care." However, in contrast to hospice, the initiation of palliative care is not contingent upon the expectation that the patient has less than six months to live or that disease-directed therapy has run its course. Across all specialties, the emphasis now is on the integration of palliative care into the ongoing management strategy for any patient with a serious, life-threatening illness, regardless of age. Hospice care is palliative care provided in the last weeks and months of life, when disease-directed or curative treatment has been exhausted or deemed no longer to be of benefit[1].
Palliative care at the end of life is delivered most effectively through hospice. Palliative care/hospice was once primarily confined to the cancer setting because of the evident and often rapid health decline to death with this disease. Hospice extended to the acquired immunodeficiency syndrome (AIDS) setting for the same reason. Ongoing advances in medicine have changed these once-lethal diseases into chronic conditions, shifting the trajectory of illness and leaving a growing number of patients in need of palliative care for longer periods of time. Similarly, individuals with other life-limiting diseases, such as heart failure, chronic obstructive pulmonary disease (COPD), end-stage renal disease, and dementia, are in need of similar care. Thus, a growing number of individuals could benefit from palliative care. However, palliative/hospice care is underutilized in the United States for a variety of reasons, and many patients experience an unnecessary degree of physical and psychological suffering at the end of life [1,2].
Both clinician- and patient-related factors contribute to the underuse of palliative/hospice care. In addition, evidence-based guidelines are lacking for end-of-life care for many noncancer life-threatening conditions. More research on the prevalence and severity of symptoms and functional status in patients with life-limiting diseases, as well as the efficacy of interventions is needed to generate these much-needed guidelines.
This course is designed to bridge the gap in knowledge of palliative care by providing an overview of the concept of palliative care and associated clinical issues and a discussion of the benefits and barriers to optimum palliative care at the end of life. Central to this discussion is an emphasis on the importance of talking to patients about the value of palliative care, of clearly presenting the prognosis and appropriate treatment options and goals, and of ensuring that advance planning is completed. Much of the course focuses on the assessment and management of the most common end-of-life needs, with particular attention to pain, the most prevalent, as well as the most distressing, physical symptom. Psychosocial and spiritual needs of the patient and family are also discussed. Palliative care presents unique challenges for some patient populations, most notably older patients, children/adolescents, and patients receiving critical care. An overview of the most important issues specific to these settings is provided.
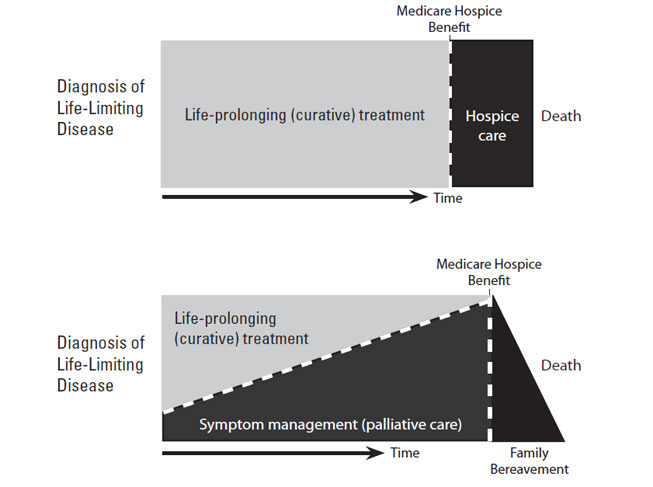
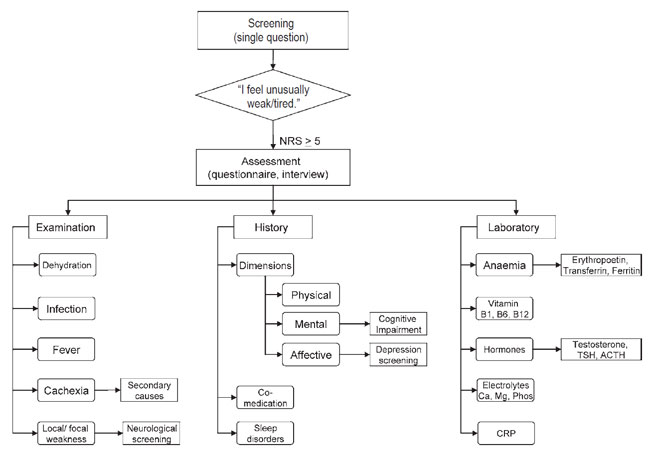
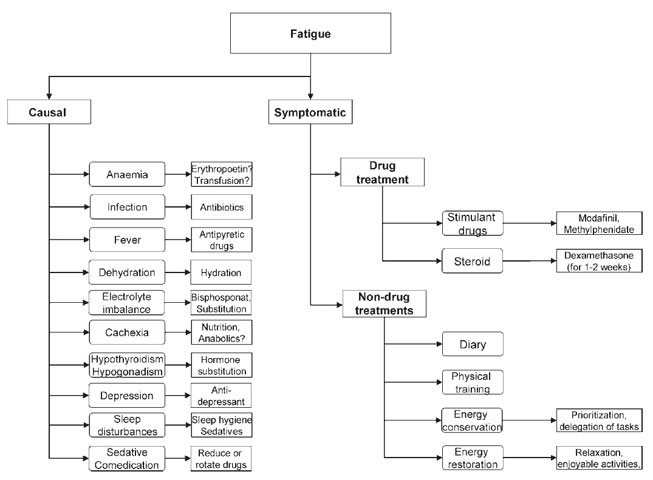
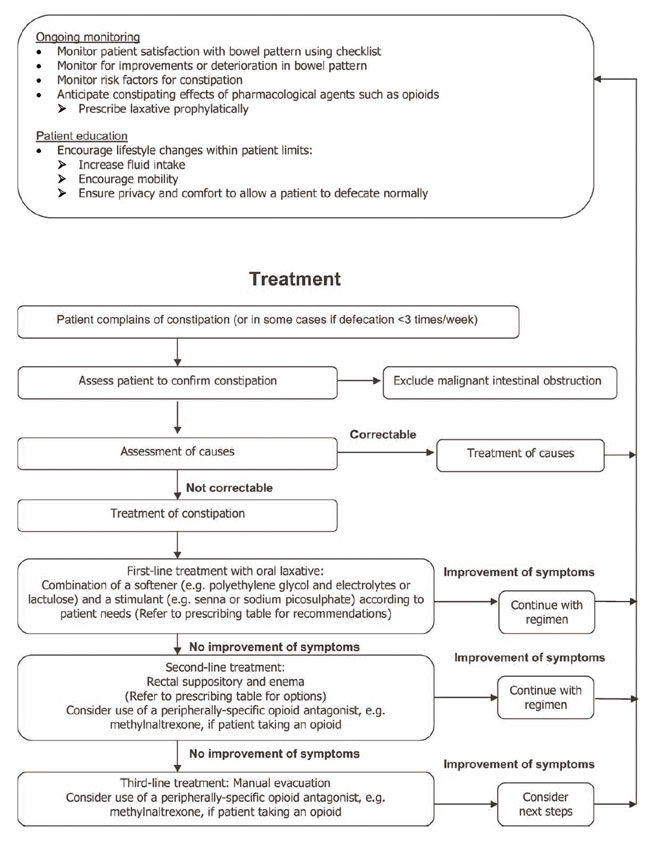
The term "palliative care" was first used by Balfour Mount, a Canada-trained physician and visiting professor at St. Christopher's Hospice, the first program of its kind. Dr. Mount subsequently established a palliative care program at Royal Victoria Hospital in Montreal, the first such program to be integrated in an academic teaching hospital [3]. Since that time, many attempts have been made to craft a definition of palliative care that represents its unique focus and goals. The challenge in defining palliative care has been encompassing all that such care refers to while specifying the timing of it (Table 1) [4,5,6,7,8]. The timing of palliative care remains an important point of discussion. As a result of its roots in hospice care, the term "palliative care" has often been considered to be synonymous with "end-of-life care." However, the current emphasis is to integrate palliative care earlier in the overall continuum of care (Figure 1) [6,9].
EVOLVING DEFINITION OF PALLIATIVE CARE
| Year | Source and Definition | Comments | ||
|---|---|---|---|---|
| 1990 | World Health Organization (WHO): "…The active total care of patients whose disease is not responsive to curative treatment." | Does not apply exclusively to palliative care | ||
| 1993 | The Oxford Textbook of Palliative Medicine: "The study and management of patients with active, progressive, far-advanced disease for whom the prognosis is limited and the focus of care is the quality of life." | Lacks essential aspects, such as support provided to families, as well as specificity about timing | ||
| 2004 |
| First definition to reflect integration of palliative care earlier into the disease continuum | ||
| 2007 | WHO (revision): "An approach that improves the quality of life of patients and their families facing the problem associated with life-threatening illness, through the prevention and relief of suffering by means of early identification and impeccable assessment and treatment of pain and other problems, physical, psychosocial, and spiritual." | Improvement over original WHO definition, but expansion of palliative care throughout the continuum of care not explicit | ||
| 2009 | American Society of Clinical Oncology: "Palliative cancer care is the integration into cancer care of therapies to address the multiple issues that cause suffering for patients and their families and have an impact on the quality of their lives. Palliative cancer care aims to give patients and their families the capacity to realize their full potential, when their cancer is curable as well as when the end of life is near." | Defines palliative care for patients with cancer, but definition can be applied to palliative care in all settings | ||
| 2013 | National Consensus Project: "Palliative care means patient and family-centered care that optimizes quality of life by anticipating, preventing, and treating suffering. Palliative care throughout the continuum of illness involves addressing physical, intellectual, emotional, social, and spiritual needs and to facilitate patient autonomy, access to information, and choice." | Characterization of palliative care in the United States, as defined by the U.S. Department of Health and Human Services and the National Quality Forum |
As the definition of palliative care has evolved, end-of-life care has become one aspect of palliative care. The time period assigned to "end of life" has not been defined, with the phrase being used to describe an individual's last months, weeks, days, or hours [10,11]. Designating a specific time period as the "end of life" is further challenged by disease trajectories that differ depending on the underlying life-limiting disease, a problem discussed in detail later in this course.
Since the establishment of the first hospice in the United States in 1974, many initiatives have been undertaken to enhance the quality of care given at the end of life. The lack of progress in relieving end-of-life suffering was highlighted with the publication of findings from the Study to Understand Prognoses and Preferences for Outcomes and Risks of Treatment (SUPPORT) [12,13]. The results of this landmark study indicated that in-hospital deaths were characterized by prolonged suffering, uncontrolled pain, and caregiver hardship. In response, the Institute of Medicine (IOM) commissioned a report on the quality of care at the end of life, and the authors of this report, Approaching Death: Improving Care at the End of Life, noted that too many patients "suffer needlessly" at the end of life and emphasized the need for better training of healthcare professionals and reform of outdated laws that inhibited the use of pain-relieving drugs [2]. A subsequent IOM report pointed out the need for enhanced pediatric palliative care [14]. Several initiatives have been developed to address the deficiencies in the quality of palliative care; to optimize the use of hospice; to help the lay public better understand the meaning of palliative care and hospice and their benefits; and to enhance the knowledge, skills, and attitudes of healthcare professionals. Five organizations—the American Academy of Hospice and Palliative Medicine (AAHPM), the Center to Advance Palliative Care (CAPC), the Hospice and Palliative Nurses Association, the Last Acts Partnership, and the National Hospice and Palliative Care Organization (NHPCO)—joined forces in the National Consensus Project for Quality Palliative Care Consortium and published clinical practice guidelines to help reduce the variation in palliative care programs and enhance continuity of care across healthcare settings [6]. The National Quality Forum (NQF) built on these guidelines when it proposed a national framework for palliative and hospice care [15].
Other efforts included the first core curriculum in hospice and palliative care, created by the AAHPM; the development of the Education in Palliative and End-of-Life Care (EPEC) Project (https://www.bioethics.northwestern.edu/programs/epec); and the subsequent development of the EPEC-Oncology (EPEC-O) curriculum and the End-of-Life Nursing Education Consortium Project (https://www.aacnnursing.org/ELNEC).
Because palliative care focuses on the physical and psychosocial needs of the patient and his or her family, the patient's and family's perspectives are vital considerations in developing high-quality palliative care programs. An early survey of patients with life-limiting diseases identified five priorities for palliative care: receiving adequate treatment for pain and other symptoms, avoiding inappropriate prolongation of life, obtaining a sense of control, relieving burden, and strengthening relationships with loved ones [16]. In another study, a spectrum of individuals involved with end-of-life care (physicians, nurses, social workers, chaplains, hospice volunteers, patients, and recently bereaved family members) echoed these findings, with the following factors being noted as integral to a "good death:" pain and symptom management, clear decision making, preparation for death, completion, contributing to others, and affirmation of the whole person [17].
The priorities set by patients and healthcare professionals were considered carefully in the structuring of clinical practice guidelines for high-quality palliative care developed by the National Consensus Project (NCP) for Quality Palliative Care. These guidelines are organized according to eight domains [6]:
Structure and processes of care
Physical aspects
Psychological and psychiatric aspects
Social aspects
Spiritual, religious, and existential aspects
Cultural aspects
Care of the patient nearing the end of life
Ethical and legal aspects
In its publication, the NQF sets forth 39 guidelines based on these eight domains (Table 2) [6].
GUIDELINES FOR PALLIATIVE AND HOSPICE CARE
|
Palliative care service is rendered through several different models, including hospital-based inpatient programs, outpatient clinics (based in hospitals or private practices), and combined consultation services and inpatient programs. Hospice programs may provide a consultative service but generally assume direct responsibility for end-of-life palliative care rendered at home, hospital, or other hospice resident facility [15]. The Joint Commission began offering an advanced certification program for palliative care in September 2011 [18]. In an effort to enhance access to end-of-life care, models of care are being adapted for a variety of specific settings, such as rural communities, correctional facilities, long-term care facilities, children's hospitals, and intensive care units [19,20,21,22,23,24].
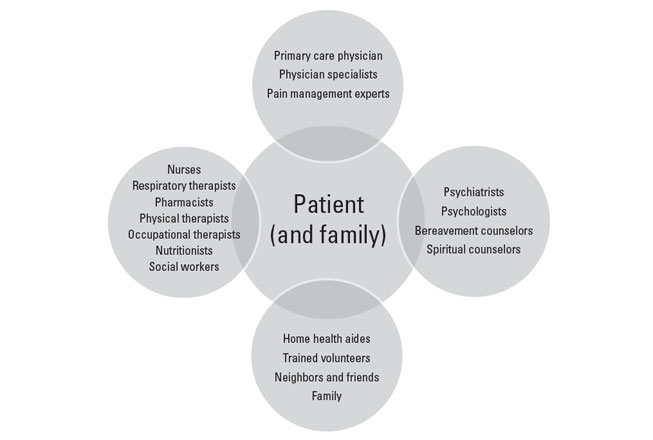
The delivery of comprehensive palliative care relies on a team of skilled providers with experience and training in the principles of palliative care (Figure 2). The team may be organized around a primary care clinician or a palliative care specialist who functions as consultant or principal provider [15,25,26,27]. Palliative care interventions have been shown to significantly improve patient outcomes, although the data are stronger for patients with cancer than for life-limiting diseases overall [28,29]. This is illustrated by results of a randomized controlled trial of early palliative care provided as an adjunct to standard oncologic care for patients with metastatic non-small cell lung cancer. In this study, involving 151 subjects enrolled from a single academic practice, patients in the intervention group were seen by a palliative care clinician regularly (once or more per month) for 12 weeks; in comparison to the group receiving only standard care, the intervention (palliative care) group had a measurably better quality of life, lower rate of depression, and improved survival by 2.7 months [30].
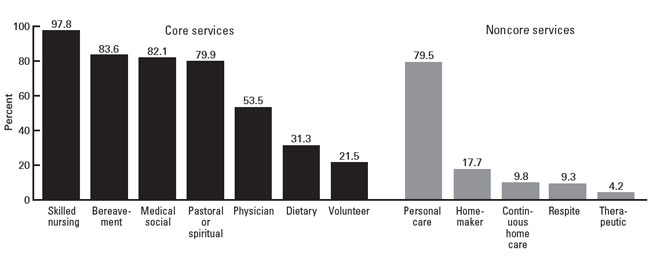
The composition of a hospice care team is essentially the same as for a standard palliative care team. The primary service provided during hospice care is skilled nursing care and management of distressing symptoms, followed by bereavement services and medical social services (Figure 3) [31]. Clinical specialists (e.g., oncologists, cardiologists, pulmonologists) also become members of a palliative care team when they are involved with the care of their patients during the end of life. Family physicians and general internists typically provide primary palliative care; this level of care requires skill in core palliative care competencies (such as basic symptom assessment and management and knowledge of psychosocial and community services) [6,8].
The composition of the healthcare team and the roles of its members may differ across palliative care settings, and roles and responsibilities should be clear and well documented to help members work effectively as a team. Team members' roles should also be communicated to the patient and the family.
The primary care physician is usually responsible for referral to palliative care through hospice when the patient has a non-cancer diagnosis. In general, the primary care physician becomes the attending physician, assuming primary responsibility for the patient [32,33]. The primary care physician should be prepared to relinquish some autonomy in order to work effectively with the interdisciplinary team [32]. Home-based hospice care is organized around a team that includes the attending physician, registered nurse, social worker, and counselor. These team members are necessary for Medicare reimbursement [34]. The attending physician collaborates with other members of the hospice team to manage symptoms and fulfills other basic obligations, such as admission orders, medication prescriptions and refills, certification of hospice eligibility, and signing of the death certificate [33].
High-quality palliative care also requires special expertise in honest, compassionate communication. In addition to enhancing the patient's and family's experience, these skills help to establish trust and overcome barriers to adequate care and relief of symptoms. Several communication tasks are especially important: conveying accurate prognostic information while maintaining hope, eliciting information about symptoms, decision making about curative and palliative treatments, handling emotions, and dealing with requests from patients and families who have unrealistic goals [35,36,37]. The challenges of communicating effectively are discussed later in this course.
Despite the increasing use of hospice, palliative care and hospice are underutilized services. The NHPCO statistics show the share of Medicare decedents who used hospice increased from 44.0% in 2010 to 51.6% in 2018; decreased to 47.3% in 2021, because of the COVID-19 pandemic; then increased to 49.1% in 2022 [1]. Hospice use varies according to several demographic factors. Patients treated in hospice are primarily women, although the gap has been closing, with 54.3% of the hospice population being female [1]. Studies show that White individuals are more likely to use hospice than are individuals in minority populations [38,39,40,41]. However, from 2018 to 2022, NHPCO data show that hospice utilization by Medicare decedents increased among all race/ethnicity groups surveyed. In 2022, 51.6% of White, 38.3% of Hispanic, 38.1% of Asian American, 37.4% of Black, and 37.1% of North American Native Medicare decedents were enrolled in hospice [1].
The lower rates of hospice use in minority populations have been attributed to many factors, including beliefs about health care, death, and end-of-life care; lack of awareness of hospice services; mistrust of the healthcare system; cultural differences in healthcare decision making and in disclosure of illness to the patient; lack of insurance; lack of healthcare professionals' cultural competency; lower referral rates by health care professionals; and the hospice caregiver requirement [40,42,43,44].
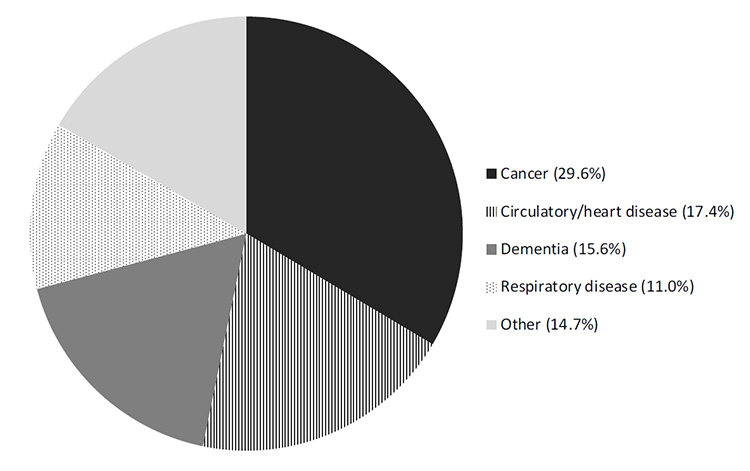
Cancer and human immunodeficiency virus (HIV)/AIDS were once the predominant diseases in hospice and palliative care programs, but as treatments for these diseases have improved, the number of individuals with the diseases in hospice programs has decreased while the number of individuals with chronic, progressive diseases has increased. In 2021, Alzheimer dementia/nervous system disorders/organic psychosis (25%), cancer (23%), and cardiac/circulatory system diseases (22%) were the three most common diagnoses (by ICD-10 code) in the hospice population, accounting for nearly three-quarters of all hospice beneficiary diagnoses (Figure 4) [1].
Most of the studies designed to determine the benefits of palliative care/hospice at the end of life have centered on patients with cancer. However, an increasing number of researchers are focusing on palliative care interventions for patients with other life-limiting diseases. The field of palliative care/hospice research has grown considerably in the past decade, but reliable meta-analyses of palliative care studies have been limited because of variations in methodology and in the focus and extent of services [45]. Increasingly, studies are confirming the benefits of palliative care/hospice in terms of quality of life, satisfaction with care, and end-of-life outcomes, as well as cost-effectiveness.
A systematic review indicated weak evidence of benefit for palliative care/hospice. The results did demonstrate significant benefit of specialized palliative care interventions in four of 13 studies in which quality of life was assessed and in one of 14 studies in which symptom management was assessed [29]. However, the authors of the review noted that most of the studies lacked the statistical power to provide conclusive results, and the quality-of-life measures evaluated were not specific for patients at the end of life [29]. Other research has shown that palliative care intervention was associated with significantly better quality of life and greater patient and/or family caregiver satisfaction [45,46,47]. Data to support benefit in reducing patients' physical and psychological symptoms have been lacking [45]. Such symptoms were significantly improved when patients received care delivered by palliative care specialists [28].
Surveys of patients' family members also demonstrate the value of palliative care. The Family Assessment of Treatment at the End of Life (FATE) survey was developed to evaluate family members' perceptions of their loved one's end-of-life care in the Veterans Administration (VA) healthcare system. FATE consists of nine domains: well-being and dignity, information and communication, respect for treatment preferences, emotional and spiritual support, management of symptoms, choice of inpatient facility, care around the time of death, access to VA services, and access to VA benefits after the patient's death. Using the assessment tool, researchers found that palliative care and hospice services were associated with significantly higher overall scores compared with usual care [48].
In addition to the benefits realized by patients, palliative care is beneficial for patients' family members as well. According to a survey of bereaved family members, a significantly higher proportion of respondents had their emotional or spiritual needs met when the patient received palliative care (compared with "usual care") [49]. Palliative care was also seen to improve family member coping skills and the ability to manage the inevitable tasks associated with terminal illness; that is, more family members knew what to expect when the patient was dying, felt competent to participate in the care of the dying person, and felt confident in knowing what to do when the patient died [49]. Other studies have shown benefit for caregivers through positive effects on caregiver burden, anxiety, satisfaction, and the ability to "move on" more easily after the patient's death [46,50].
The most surprising finding is the apparent survival advantage conferred by palliative and hospice care. One study showed that hospice care extended survival for many patients within a population of 4,493 patients with one of five types of cancer (lung, breast, prostate, pancreatic, or colorectal cancer) or heart failure [51]. For the population as a whole, survival was a mean of 29 days longer for patients who had hospice care than for those who did not. With respect to the specific diseases, heart failure was associated with the greatest increase in survival (81 days), followed by lung cancer (39 days), colorectal cancer (33 days), and pancreatic cancer (21 days) [51]. There was no survival benefit for patients with breast or prostate cancer. In a study of patients with metastatic non-small cell lung cancer, patients who received early palliative care (within three weeks after enrollment in the study) lived significantly longer than those who received standard oncologic care only (11.6 months vs. 8.9 months) [30]. In the same study, the quality of life and symptoms of depression were also significantly better for the cohort of patients who received early palliative care. Similarly, a retrospective study found a slight survival advantage to hospice care among older individuals (>65 years) with advanced lung cancer [52]. These observations prompted the American Society of Clinical Oncology (ASCO) to publish a Provisional Clinical Opinion in which it states that concurrent palliative care and standard oncologic care should be offered to people with metastatic non-small cell lung cancer at the time of initial diagnosis [53]. The ASCO Opinion also notes that although the evidence of survival benefit is not as strong for other types of cancer, the same approach should be considered for any patient with metastatic cancer and/or high symptom burden [53]. The 2013 American College of Chest Physicians (ACCP) guideline for the diagnosis and management of lung cancer also recommends that "palliative care combined with standard oncology care be introduced early in the treatment course" for patients with late-stage (i.e., stage IV) lung cancer and/or a high symptom burden [54].
The cost of care at the end of life is a controversial issue because of the disproportionate costs incurred for care within the last two years of life and the wide variation in costs related to the aggressiveness of care across healthcare facilities [55]. The simple act of discussing end-of-life issues can help patients and families better understand options, leading to reduced costs. In a study of 603 patients with advanced cancer, costs in the last week of life were approximately $1,000 lower for patients who had end-of-life discussions with their healthcare providers compared with patients who did not have such conversations [56].
Several studies have documented the cost-effectiveness of hospice care. A meta-analysis published in 1996 showed that hospice care reduced healthcare costs by as much as 40% during the last month of life and 17% over the last six months [57]. A later study demonstrated little difference in costs at the end of life, with the exception of costs for patients with cancer, which were 13% to 20% lower for those who had received hospice care than for those who had not [58]. In a study of 298 patients with end-stage organ failure diseases, in-home hospice care significantly reduced healthcare costs by decreasing the number of hospitalizations and emergency department visits [46]. The strongest evidence of cost savings is found in a 2007 study in which hospice use reduced Medicare costs during the last year of life by an average of $2,309 per hospice user [59]. As was found earlier, the cost savings were greater for patients with cancer than for those with other diagnoses [59]. The greatest cost reduction (about $7,000) was associated with a primary diagnosis of cancer and length of stay of 58 to 103 days [59]. The maximum cost savings was much lower (approximately $3,500) for other life-limiting diagnoses but with a similar length of stay (50 to 108 days) [59].
Palliative care consultations also reduce costs. A review of data for Medicaid beneficiaries (with a variety of life-limiting diagnoses) at four hospitals in New York showed that hospital costs were an average of $6,900 lower during a given admission for patients who received palliative care than for those who received usual care [60]. The reduction in costs was greater ($7,563) for patients who died in the hospital compared with those who were discharged alive [60].
Despite the many benefits of palliative care and hospice, referrals are usually not timely and often are not made at all [61,62,63,64,65,66]. Many challenges contribute to the low rate of optimum end-of-life care.
Among the most important barriers to the optimum use of palliative care at the end of life are the lack of well-trained healthcare professionals; reimbursement policies; difficulty in determining accurate prognoses; and attitudes of patients, families, and clinicians.
Medical school and residency training programs emphasize disease recognition, diagnostic assessment, and treatment and management strategies that have restorative power, prolong life, and prevent death. The role of palliative care traditionally has not been sufficiently addressed [67]. Students who have participated in mandatory courses in palliative medicine have noted that they are better prepared to care for dying patients [68]. Efforts to enhance education have resulted in the development of more than 100 primary care residency programs that offer palliative medicine as part of the curriculum and 72 postgraduate medical fellowship programs in palliative care [69,70]. In addition, hospital-based palliative care programs have integrated the eight NCP domains into graduate courses and residencies for physicians and registered nurses, and certifications in palliative care have become available for physicians, nurses, and social workers [6]. Between 1996 and 2006, more than 2,100 physicians obtained certification in hospice and palliative medicine from the American Board of Hospice and Palliative Medicine [71]. As of January 2016, there were nearly 6,400 active certified hospice and palliative care physicians in the United States [72]. In 2006, subspecialty certification in hospice and palliative medicine was established for 10 Boards within the American Board of Medical Specialties. The first exam was held in 2008, and 1,274 physicians earned certification in hospice and palliative medicine. Since then, the number of physicians who have earned certification though the American Board of Medical Specialties has increased fivefold, with physicians in internal medicine and family medicine accounting for 85% of the total (Table 3) [73].
NUMBER OF PHYSICIANS CERTIFIED IN SUBSPECIALTY OF HOSPICE AND PALLIATIVE MEDICINE, 2014–2023
| American Board Specialty | No. of Physicians |
|---|---|
| Internal medicine | 4,167 |
| Family medicine | 1,573 |
| Pediatrics | 268 |
| Anesthesiology | 100 |
| Emergency medicine | 247 |
| Psychiatry and neurology | 119 |
| Surgery | 70 |
| Radiology | 60 |
| Obstetrics and gynecology | 71 |
| Physical medicine and rehabilitation | 29 |
| Total | 6,604 |
Initiatives to enhance the knowledge and skills of nurses have included graduate nursing programs in palliative care, instructional resources for nursing educators, communication skills training for nurses, and educational programs for home care professionals, as well national certifications [6,74]. More than 18,000 nurses are Board-certified in hospice and palliative nursing [75].
Medicare reimbursement for hospice care became available when the Medicare Hospice Benefit was established in 1982, and reimbursement through private health insurances soon followed [34]. Reimbursement for hospice enabled more people with life-limiting disease to receive palliative care at home and in hospice units: the number of hospices in the United States has increased steadily, from 158 Medicare-certified hospices in 1985 to 4,639 in 2018 [1]. Despite the positive impact of the Medicare Hospice Benefit, fewer than half of eligible Medicare beneficiaries use hospice care and most only for a short period of time. This is because Medicare beneficiaries are required to forgo Medicare payment for care related to their terminal condition in order to receive access to Medicare hospice services (Table 4) [34,85]. The eligibility requirements of the benefit explicitly state that the focus of hospice "is on caring, not on curing," and in order to receive reimbursement for hospice services, patients must sign a statement that they will forego curative treatment [34]. This requirement frightens some patients or their families, who subsequently view hospice as "giving up." Furthermore, the restriction does not account for palliative treatments that serve the dual purpose of alleviating symptoms while prolonging life. For example, therapeutic regimens and measures designed to optimally treat heart failure are the same as those used for palliative care of patients with heart failure [76]. At present, there are no Medicare regulations that specify which treatments are considered palliative, and this lack of clarity has led to variation in what treatments individual hospice programs offer. Hospice care may be denied to patients receiving palliative chemotherapy or radiotherapy, and this may result in many people not choosing hospice. Although oncology experts have noted that radiotherapy is an important component of palliative care for many people with metastatic cancer, only 3% of people receiving hospice care receive radiation therapy; expense and the need to transport patients were the primary barriers [77,78,79]. Other palliative interventions, such as chemotherapy, blood transfusions, total parenteral nutrition, and intravenous medications, may not be economically feasible for small hospice units but may be possible at larger ones [80,81,82].
MEDICARE HOSPICE BENEFIT
| Variables | Criteria | |||||
|---|---|---|---|---|---|---|
| Benefits (covered services) |
| |||||
| Nonreimbursable services |
| |||||
| Period of care | Two 90-day periods, followed by unlimited number of 60-day periods | |||||
| Restrictions |
|
Many have suggested that the hospice model should change to allow for integration of disease-directed therapy [83,84]. The Affordable Care Act of 2010 stipulates that the Centers for Medicare & Medicaid Services (CMS) implement a three-year demonstration project to evaluate concurrent hospice care and disease-directed treatment [84]. This project represents a significant change to the eligibility criteria and, while the change has the potential to improve access to hospice care, careful assessment of the effect of concurrent treatment on use of hospice as well as on quality of life, quality of care, survival, and costs is needed [84]. Phase 2 of the project, the Medicare Care Choices Model (MCCM), became a six-year study (2016–2021) to assess whether offering Medicare beneficiaries the option to receive supportive, palliative care services through hospice providers without forgoing Medicare payments for treatment of their terminal conditions would improve beneficiaries' quality of life, increase their satisfaction with care, and reduce Medicare expenditures. In all, 89 of141 (63%) Medicare-certified hospices participated in MCCM; however, only 44 (31%) participated for all six years [85].
Of 7,253 Medicare beneficiaries who enrolled in the MCCM program, all qualified for hospice and met other eligibility criteria, including having cancer, heart failure, chronic pulmonary disease, or HIV/AIDS [85]. Enrollees received supportive and palliative care services through MCCM while continuing to receive Medicare coverage for disease-directed treatment of their terminal condition. Specific MCCM-directed services included assessment of health and health-related social needs, care coordination and case management, access to healthcare professionals, person- and family-centered care planning, shared decision-making, and management of symptoms. Length of enrollment varied (median: two months) and 89% of enrollees died before the end of the MCCM program. Surveyed MCCM enrollees and caregivers reported high levels of satisfaction with their quality of life, shared decisions, and receiving care consistent with individual wishes. MCCM enrollees had 12% fewer outpatient emergency department visits, 26% fewer inpatient admissions, and lower net Medicare expenditures when compared to a matched group of non-participants [85]. Deceased enrollees were less likely than comparison beneficiaries to receive aggressive life-prolonging treatment in the last 30 days of life and spent more days at home before death.
The Medicare Hospice Benefit criterion of a life expectancy of six months or less has also affected the timeliness of referral to hospice because of the aforementioned challenges in predicting prognosis. Many hospices were accused of fraud and were assessed financial penalties when government review found documentation of patients who received hospice care for longer than six months. As a result, many clinicians delayed hospice referral because of their lack of confidence in their ability to predict survival within six months. However, the six-month regulation has been revised, and a penalty is no longer assessed if a patient lives beyond six months if the disease runs its normal course [34].
Unfortunately, reimbursement for end-of-life care discussions is not as straightforward as for hospice care. An effort to establish government reimbursement for discussions of end-of-life care options, including hospice care and advance directives, sparked a political storm that led to the removal of the proposed reimbursement from the healthcare reform bill of 2011. However, beginning in January 2016, the CMS introduced two Current Procedural Terminology (CPT) reimbursement codes for advance care planning visits [86,87]. Despite a national increase in advance care planning claims, the overall claims rate remains low. Two-thirds of hospice and palliative medicine specialists did not use the new CPT codes in 2017, despite working with seriously ill patients [87].
To make appropriate referrals to hospice, clinicians must be able to determine accurate prognoses, at least within the six-month timeframe required for reimbursement. However, prognostication is a complex issue and is a primary barrier to hospice use [88,89,90,91,92,93,94,95]. Studies have found that physicians typically overestimate survival, and one study found that physicians overestimate prognosis both in determining it and in communicating it to the patient [93,96,97]. The difficulty in determining the risk of death within a specific time period not only affects the ability of clinicians to make appropriate referrals to hospice but also impedes the ability of patients and families to make necessary end-of-life decisions, with many patients not fully understanding the severity and progressive nature of the disease [98].
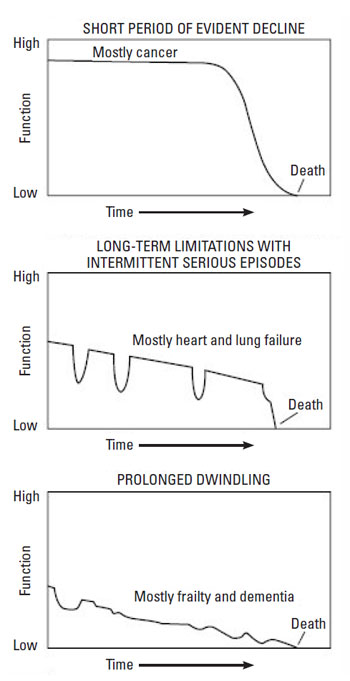
Several factors contribute to physicians' difficulty in prognostication, including a desire to meet the patient's needs (for a cure or prolongation of life) and a lack of reliable prognostic models [81,97,99]. Perhaps the most important factor contributing to prognostic difficulty is the variations in disease trajectories, which have been characterized as a short period of evident decline, long-term limitations with intermittent serious episodes, and a prolonged decline (Figure 5) [9,32,100].
How difficult it is to determine a prognosis depends on the disease trajectory. Determining a prognosis in the cancer setting was once clear-cut because of the short period of evident decline, but advances in cancer therapies have made it more difficult to estimate a prognosis. Studies have shown rates of accurate prognosis of 20%, with survival usually overestimated, up to a factor of five [93,96]. The unpredictable course of organ-failure diseases, with its long-term limitations and acute exacerbations has always made prognostication difficult [62,89,101,102]. In a survey of cardiologists, geriatricians, and internists/family practitioners, approximately 16% of respondents said they could predict death from heart failure "most of the time" or "always" [89]. Predicting survival for people with the third type of trajectory (prolonged decline) is extremely difficult because of the wide variation in progressive decline. The prognosis for dementia can range from 2 to 15 years, and the end-stage may last for 2 years or more [103,104].
To help facilitate more timely referrals to hospice, the NHPCO established guidelines for determining the need for hospice care, and these guidelines were adopted by the Health Care Finance Administration to determine eligibility for Medicare hospice benefits [76]. Other prognostic models have been developed, such as the SUPPORT model, the Palliative Prognostic (PaP) Score, and the Palliative Prognostic Index (PPI) [12,105,106,107]. Most were developed for use in the cancer setting and for hospitalized patients, and their value beyond those settings has not been validated [81,95]. In addition, the PaP and the PIP will identify most patients who are likely to die within weeks but are much less reliable for patients who have 6 to 12 months to live [95]. A systematic review showed that the NHPCO guidelines, as well as other generic and disease-specific prognostic models, were not adequately specific or sensitive to estimate survival of at least six months for older individuals with nonmalignant life-limiting disease, especially heart failure, COPD, and end-stage liver disease [99].
Most prognostic tools for organ-failure diseases are used to estimate the risk of dying and to select patients for treatment, not to determine when end-of-life care should be initiated. Several models have been established to determine prognosis for heart failure; the one used most often is the Seattle Heart Failure model, which represents the most comprehensive set of prognostic indicators to provide survival data for one, two, and five years [108,109]. Newer evidence-based recommendations for estimating survival in advanced cancer have been published, as has a nomogram; however, use of the nomogram for hospice referral is limited, as it estimates survival at 15, 30, and 60 days [81,110].
For estimating prognosis in advanced dementia—a condition with the most challenging disease trajectory—the Advanced Dementia Prognostic Tool (ADEPT) has been shown to be better than the NHPCO guidelines in identifying nursing home residents with advanced dementia at high risk of dying in six months [111]. However, the ability of ADEPT to identify these patients is modest [111]. Lastly, the Patient-Reported Outcome Mortality Prediction Tool (PROMPT) was developed to estimate six-month mortality for community-dwelling individuals 65 years or older with self-reported declining health over the past year; the model shows promise for making appropriate hospice referrals, but the model needs validation [112].
In addition to the low reliability of these models, another problem is that the clinician's prediction of survival remains integral, as it is one element in prognostic models, sometimes representing as much as half of a final score [110]. Other variables include performance status, laboratory data, and quality of life scales.
Researchers continue to evaluate prognostic variables to establish criteria for prognosis, especially disease-specific criteria. In its guidelines for palliative care, the Institute for Clinical Systems Improvement (ICSI) distinguished between the clinical indicators that should prompt palliative care discussions and those that should prompt hospice referral (Table 5) [113]. According to the ICSI, "all hospice is palliative care, but not all palliative care is hospice" [113].
COMPARISON BETWEEN PALLIATIVE CARE AND HOSPICE
| Condition | Palliative Carea | Hospiceb | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Cancer |
| Any patient with metastatic or inoperable cancer | |||||||||
| Heart disease |
|
| |||||||||
| Pulmonary disease |
|
| |||||||||
| Dementia |
|
| |||||||||
| Liver disease |
|
| |||||||||
| Renal disease |
|
| |||||||||
| Neurologic disease |
|
| |||||||||
| |||||||||||
This difficulty in determining prognosis can have a negative impact on the appropriate timing of hospice referral and the degree of benefit to be derived. Although the use of hospice has increased over the past decades, the timing of referral has not changed significantly since the mid-1980s [114]. The average length of hospice care is much lower than the six months allowed by the Medicare benefit; in 2022, the average length was 95.3 days, and the median duration (a more accurate reflection because it is not influenced by outliers) was 18 days [1]. In addition, approximately 25% of patients died (or were discharged) within only five days [1]. Studies have indicated that the benefits of hospice increase as the duration of care increases, and such services as bereavement counseling, palliative care, and respite for caregivers is best when hospice care is provided for four to eight weeks, a longer period of time than the median stay [59,115].
Longer durations of hospice services are also linked to family members' perceptions of the quality of care. According to the findings of 106,514 surveys from 631 hospices in the United States, 11% of family members thought their loved one was referred "too late" to hospice; this perception was associated with more unmet needs, higher reported concerns, and lower satisfaction [116].
In contrast to the restrictions on access to hospice, there are no restrictions on access to palliative care. Referrals for palliative care should be made on the basis of actual or anticipated needs at any time during the disease continuum; referrals should not be made on the basis of prognostic models [81,99]. Referrals for specialist palliative care should be made when treatment goals change from curative to palliative [117,118]. A consensus report from the Center to Advance Palliative Care provides guidance for identifying patients with a life-limiting illness who are at high risk of unmet palliative care needs [118]. The report includes criteria for referral for palliative care assessment at the time of hospital admission and during each hospital day (Table 6) [118]. Experts in nonmalignant life-limiting diseases are calling for earlier palliative care consultation. Such consultation before implantation of a left ventricular assist device as destination therapy is recommended, as it has been shown to improve the quality of care and advance care planning [119,120]. Guidelines for renal and respiratory diseases note that all patients with these diseases should be offered palliative care services, and the integration of palliative care specialists into liver transplantation teams has been suggested [121,122,123].
CRITERIA FOR PALLIATIVE CARE ASSESSMENT AT THE TIME OF HOSPITAL ADMISSION AND DURING HOSPITAL STAY
| At Time of Hospital Admission | ||||||||||
| Primary criteriaa |
| |||||||||
| Secondary criteriab |
| |||||||||
| During Hospital Stay | ||||||||||
| Primary criteriaa |
| |||||||||
| Secondary criteriab |
| |||||||||
| ||||||||||
Physicians have reported that they delay discussions of palliative care and hospice because they fear the reaction of the patient and/or family [32,33]. Negative reactions are grounded in a lack of accurate knowledge about palliative care and hospice. According to two polls conducted in 2011 (800 adults in one poll and 1,000 adults in the other), 70% to 92% of respondents were not "too" or "at all" familiar with the term palliative care [124,125].
Enhancing the public's knowledge can improve access to palliative care: the 2011 polls showed that once palliative care was appropriately defined, 92% said they were likely (63% "very likely" and 29% "somewhat likely") to consider palliative care for a loved one who had a serious illness and 96% said that it was important for palliative (and end-of-life) care to be a top priority for the healthcare system [124,125].
Hospice is a more familiar concept to the general population. One of the polls showed that 86% of respondents were familiar with the term hospice care, and other studies have indicated that approximately half of patients with a life-limiting illness know what hospice is [125,126]. Although people may be familiar with the term, many believe several myths about hospice; for example, that hospice is only for old people, is only for people with cancer, is for people who do not need a high level of care, is used when there is no hope, and is expensive [127].
Several other factors contribute to negative feelings about hospice [80,88,128]:
Denial or lack of awareness about the severity of the illness
Not wanting to "give up"
Fear of abandonment by the family physician
Perception that the patient will not receive adequate medical services
Interpretation of hospice referral as a cost-savings measure
When initiating a discussion about palliative care and hospice, clinicians should always first ask the patient if he or she has heard of either term and, if so, to describe his or her experience and knowledge [129]. Guidelines on communicating in the end-of-life setting note that clinicians must "clarify and correct misconceptions" about palliative care, especially emphasizing that such care is not limited to people who are imminently dying [117]. Clinicians should also address the factors that act as barriers to hospice by explaining that the goal of hospice is to die naturally—in the patient's own time, not sooner—and by ensuring that patients and families are fully informed about the prognosis, understand that the physician will be available for care, and know that routine care will continue [98,130].
Clinicians also need to evaluate their own attitudes about the use of curative therapies and hospice. Their interpretation of quality of life, a focus on longer survival rather than better quality of life, a fear of failure, and religious and cultural beliefs may influence their decision making about treatment options for patients near the end of life [131].
Communicating effectively about palliative care and hospice requires basic patient-physician communication skills as well as skills specific to the end-of-life setting. The importance of effective patient-clinician communication across all healthcare settings has received heightened attention over the past several years, as studies have shown a direct relationship between enhanced communication and better patient decision making, patient satisfaction, adherence to treatment, health-related quality of life, and survival [35,67].
Among the most important factors for effective communication across all healthcare settings are knowledge of the language preference of the patient and family; an awareness of the patient's and family's health literacy levels; and an understanding of and respect for the patient's and family's cultural values, beliefs, and practices (referred to as cultural competency) [132,133,134]. These issues are significant, given the growing percentages of racial/ethnic populations. According to U.S. Census Bureau data from 2019, more than 67.8 million Americans speak a language other than English in the home, with more than 16.1 million of them (5.2% of the population) reporting that they speak English less than "very well" [135]. Clinicians should ask their patients what language is spoken at home and what language they prefer for their medical care information, as some patients prefer their native language even though they have said they can understand and discuss medical information in English [136]. When the healthcare professional and the patient speak different languages, a professional interpreter should be used. Studies have demonstrated that the use of professional interpreters rather than "ad hoc" interpreters (untrained staff members, family members, friends) facilitates a broader understanding and leads to better outcomes [137,138]. Using a family member as a translator confuses the role of that member in the family, may involve confidentiality issues, and may lead to a modified message to protect the patient. In addition, individuals with limited English language skills have indicated a preference for professional interpreters rather than family members [139]. Professional interpreters have recommended that clinicians can further enhance the quality of care by meeting with interpreters before discussions of bad news and by explicitly discussing with the interpreter whether strict interpretation or cultural brokering is expected [140].
Knowledge of the family's health literacy is important for achieving treatment goals and good outcomes, yet most individuals lack adequate health literacy. Studies have indicated that as many as 26% of patients have inadequate health literacy, which means they lack the ability to understand health information and make informed health decisions; an additional 20% have marginal health literacy [141,142,143]. Health literacy varies widely according to race/ethnicity, level of education, and gender, and clinicians are often unaware of the literacy level of their patients and family [134,144].
Several instruments are available to test the health literacy level, and they vary in the amount of time needed to administer and the reliability in identifying low literacy. Among the most recent tools is the Newest Vital Sign (NVS), an instrument named to promote the assessment of health literacy as part of the overall routine patient evaluation [145]. The NVS takes fewer than three minutes to administer, has correlated well with more extensive literacy tests, and has performed moderately well at identifying limited literacy [134,144]. Two questions have also been found to perform moderately well in identifying patients with inadequate or marginal literacy: "How confident are you in filling out medical forms by yourself?" and "How often do you have someone help you read health information?" [134]. Clinicians should adapt their discussions and educational resources to the patient's and family's identified health literacy level and degree of language proficiency and should also provide culturally appropriate and translated educational materials when possible.
Cultural competency is essential for addressing healthcare disparities among minority groups [132]. Clinicians should ask the patient about his or her cultural beliefs, especially those related to health and dying, and should be sensitive to those beliefs [146]. In addition, information sharing and the role of decision maker vary across cultures, and the healthcare team must understand the family dynamics with respect to decision making [117]. Clinicians should not make assumptions about the preferences of the patient or family on the basis of cultural beliefs. Even within a single culture or ethnicity, the level of information desired, preferences for treatment, role of other family members in decision making, and goals of care differ among patients and families [40,117]. Clinicians should ask their patients about these issues, as well as other family and social factors and religious or spiritual views [40].
Patients and families have noted that communication about end-of-life care is one of the most important skills for clinicians to have [147]. Experts in end-of-life communication note that physicians have an obligation to discuss medical, psychosocial, and spiritual needs with seriously ill patients in a timely and sensitive manner [148]. In addition, communication guidelines developed by an Australian and New Zealand Expert Advisory Group recommend "all patients with advanced progressive life-limiting illnesses be given the opportunity to discuss prognosis…and end-of-life issues" [117]. At what point in the trajectory of serious illness such conversations should commence is not clear. Studies show that most older adults (older than 65 years of age) prefer to begin a discussion of life expectancy/end-of-life issues with their physician at about six months before anticipated end of life, rather than waiting until weeks or days before [528].
Although the topic is emotionally and intellectually overwhelming for patients and families, they want information. In a systematic review (46 studies), Parker et al. found that patients with advanced life-limiting illnesses and their families have a high level of information needs at all stages of disease [149]. That study and others have shown that the end-of-life issues of most importance to patients are [62,149]:
Disease process
Prognosis for survival for quality of life
Likely symptoms and how they will be managed
Treatment options and how they will affect quality and duration of life
What dying might be like
Advance care planning
Most patients want some discussion of end-of-life issues (including hospice care) at the time a life-limiting illness is diagnosed or shortly thereafter [62,149].
Although many physicians say they avoid discussing end-of-life issues because they are afraid the conversation will destroy the patient's hope, the discussion actually offers many benefits: it makes patients fully informed and thus better able to make decisions about treatment options and care goals; provides patients with an opportunity to achieve closure on life and family issues; allows patients to handle practical matters; and enables patients to carry out advance care planning [35,81,148,150]. As such, the discussion empowers patients, giving them a sense of control over choices [148,150]. Patients who discuss end-of-life issues and goals of care with their clinician also are more likely to receive care that is consistent with their preferences, to enroll in hospice, to complete advance directives, and are less likely to be intubated or to die in an intensive care unit [151,152].
Despite these benefits, studies have consistently shown that few clinicians and patients discuss end-of-life issues or discuss them in a timely manner. Overall, about 25% to 33% of physicians have noted that they did not discuss hospice or end-of-life care with their patients who have life-limiting diseases [128]. In a multiregional study of more than 1,500 people with stage IV lung cancer, 47% had not discussed hospice within four to seven months after diagnosis [153]. Discussions are particularly lacking among people with nonmalignant life-limiting diseases, with 66% to more than 90% of patients or clinicians reporting that they had not discussed end-of-life issues [62,126,154,155].
Even among clinicians who discuss end-of-life care with their patients, the timing is not optimal. Approximately 24% of physicians have noted that they provide hospice information at the time of diagnosis, the point at which this discussion is recommended [128,156]. In a national survey of clinicians caring for people with cancer, most respondents said they would wait until treatment options had been exhausted or symptoms had occurred before discussing end-of-life issues, and many said they would have the discussion only if the patient or family raised the issue [157].
Patients and clinicians should talk about end-of-life issues early to avoid discussing the topic during the stress of exacerbated disease or imminent death. The topic can then be framed as a component of care for all patients with a life-limiting illness [62,117]. According to published guidelines and expert recommendations, end-of-life issues should be discussed when the clinician would not be surprised if the patient died within six months to one year [6,117,148]. As other markers, an end-of-life discussion is generally recommended in the presence of moderate or severe COPD, during evaluation for liver transplantation, and in the presence of stage 4 or 5 chronic kidney disease or end-stage renal disease [62,121,123]. The 2009 ACCF/AHA guideline for the diagnosis and management of heart failure noted that end-of-life care options should be discussed when "severe symptoms in patients with refractory end-stage heart failure persist despite application of all recommended therapies;" the 2013 guideline for the management of heart failure is less clear about the timing of such a discussion [158,159]. The ACCP recommends discussing end-of-life care options when caring for patients with advanced lung cancer [54].
Other indications that should prompt a conversation about end-of-life care are a discussion of prognosis or of a treatment option with a low likelihood of success, a change in the patient's condition, patient and/or family requests or expectations that are inconsistent with the clinician's judgment, recent hospitalizations, and patient and/or family questions about hospice or palliative care [117,148].
Several patient-related and clinician-related factors contribute to the low rate of end-of-life discussions or their untimeliness. Most patients will not raise the issue for many reasons: they believe the physician should raise the topic without prompting, they do not want to take up clinical time with the conversation, they prefer to focus on living rather than death, and they are uncertain about continuity of care and fear abandonment [62,117,148,150]. Clinician-related factors include [81,147,148,160,161]:
Lack of time for discussion and/or to address patient's emotional needs
Uncertainty about prognosis
Fear about the patient's reaction (anger, despair, fear)
Lack of awareness and inability to elicit the concerns of patients and their families regarding prognosis
Lack of strategies to cope with own emotions and those of patient and family
Feeling of hopelessness or inadequacy about the lack of curative therapies (perceived as "giving up")
Perhaps the greatest barrier to end-of-life care discussions is clinicians' lack of confidence in their ability to talk about end-of-life issues, and research has confirmed a low rate of effective communication skills among clinicians, especially with respect to delivering "bad news" [62,81,155,162].
The Australian/New Zealand communication guideline provides several evidence-based recommendations for discussing end-of-life issues, and other experts have offered practical guidance to help clinicians discuss bad news and end-of-life care more effectively [117,163,164,165]. These guidelines and expert recommendations emphasize communication behaviors that patients and families have noted to be most important, such as expression of empathy, acknowledgment and support of emotions, honesty, willingness to listen more than talk, and encouragement of questions [81,117,123,147,149,164].
The most commonly recommended communication approach is SPIKES, a six-step protocol that was developed for delivering bad news in the oncology setting and can be used in other settings [163,164]:
Setting (context and listening skills)
Patient's perception of condition and seriousness
Invitation from patient to give information
Knowledge—explaining medical facts
Explore emotions and empathize as patient responds
Strategy and summary
In establishing the setting, the clinician should ask the patient if he or she wishes to have a family member present for the conversation and should ensure that the discussion takes place in privacy [62,164]. The clinician should also introduce himself or herself to the patient and any others present. With SPIKES, the setting also involves listening skills—the use of open-ended questions, clarification of points, and avoidance of distractions [164].
A 2024 clinical practice feature authored by palliative care experts provides practical guidance to clinicians on navigating and communicating about serious illness and end of life [529]. These experts suggest that rather than a single conversation, the task and the goals of communication over end-of-life issues can be achieved more effectively through a series of conversations conducted over a span of time, focusing on the patient's evolving ability to cognitively and emotionally integrate the likely course and expected outcome of the illness [529]. This approach gives the patient time to integrate prognostic information, adjust emotionally to the impact of disease progression, and then, with growing discernment, express personal preferences for end-of-life care. The tendency of patients to oscillate between expressions of hopefulness and more realistic expectations should be considered a normal and expected part of the process. Patients require time and support to process their hopes and fears, to grieve, and to build coping skills required for living with a terminal illness. By partnering with the patient, demonstrating empathy, and engaging in a continuum of conversation over weeks to months, the clinician (in concert with other members of the care team) can better discern what is most important to the patient and incorporate these goals and values into decisions about therapy, including care at the end of life [529].
Bad news—even when delivered clearly and compassionately—can affect the ability of patients and family members to understand and retain information. To minimize misinterpretation, clinicians should use simple (jargon-free) language and open-ended questions and ask follow-up questions that include the patient's own words [117,164]. Clinicians should also check often to make sure the patient and/or family understands, as research has shown that clinicians tend to overestimate their patients' understanding of end-of-life issues [166]. The discussion should focus on the importance of relieving symptoms and enhancing the quality of life, to avoid having the patient and/or family think that the clinician is "giving up" or abandoning the patient [40,117]. Clinicians should also provide educational resources in a variety of formats (print, Web-based, video, etc.) to address different learning styles.
It was once thought that the ability to communicate effectively was innate and thus could not be taught [164]. However, multiday communication skills training programs have enhanced the skills and behaviors of beginning and experienced physicians and nurses. These programs have improved clinicians' use of more focused questions and open questions, expression of empathy, and appropriate responses to cues [167,168]. Patient-related interventions have also helped to enhance end-of-life discussions. A structured list of questions and the use of individualized feedback forms regarding end-of-life preferences have led more patients to ask their physicians about end-of-life care [169,170].
Most patients say that they want to know their prognosis, and most clinicians believe that patients and families should be told the truth about the prognosis [122,126,150]. However, discussions of prognosis are lacking among clinicians and patients with life-limiting diseases. Across studies and surveys, fewer than half of patients have had a truthful discussion of prognosis [81,108,150]. Many physicians have said they discuss prognosis only when asked by the patient or family [81].
In discussing prognosis, clinicians tend to be overly optimistic, and, although most clinicians believe that they should be truthful, they sometimes withhold the truth, often at the request of a family member [160]. Honesty about the prognosis, with acknowledgment of inherent uncertainty, is needed because patients who are aware of their prognosis are more likely to choose hospice rather than aggressive treatment and to carry out advance directives [31,81,171]. Conversely, patients who are not fully aware of their prognosis tend to overestimate their life expectancy, which can influence decision making about treatment options [129].
As with other end-of-life issues, the prognosis should be discussed when the clinician would not be surprised if the patient died within six months to one year [6,117,148]. For patients with cancer, it is recommended that the prognosis be discussed within one month after a new diagnosis of advanced cancer is made [161]. A guideline from the Renal Physicians Association notes that prognosis should be fully discussed with all patients who have stage 4 or 5 chronic kidney disease or end-stage renal disease [121]. A discussion about prognosis is also recommended before the initiation of such treatments as implantation of a left ventricular assist device, dialysis, and ventilator support [122,150,172,173,174].
Clinicians should carefully prepare for the discussion of prognosis by reviewing the patient's medical record and talking to other healthcare professionals involved in the care of the patient [117]. Because there is variation among patients with regard to their desire for information, clinicians should follow the "ask-tell-ask" approach: ask the patient if he or she is willing to discuss prognosis; if yes, discuss the prognosis and then ask the patient to confirm his or her understanding [62,164]. When discussing prognosis, quantitative estimates are more understandable for patients and family than qualitative ones (such as "poor"), and general timeframes for survival should be given [62,81,164,175]. In addition, clinicians should emphasize that prognosis is determined by looking at large groups of patients and that it is harder to predict survival for an individual [62,121,129,161]. The discussion of prognosis is often not documented in the patient's record but should be [117].
Treatment options and goals of care are other topics that are often avoided in the end-of-life setting. A discussion of the survival benefit of palliative chemotherapy is frequently vague or absent from discussions of treatment options for patients with cancer [176]. In another example, approximately 60% to 95% of physicians involved with the care of patients with heart failure have two or fewer conversations about deactivation of implantable cardioverter defibrillators, and the discussions are usually within the last few days of life [89,177].
Deciding when curative therapy should end is difficult because of the advances made in treatment and life-prolonging technology and the unpredictable course of disease, especially for organ-failure diseases. These factors have led many patients, as well as some clinicians, to have unrealistic expectations for survival [30,178]. Unrealistic expectations are a major contributor to an increased use of aggressive treatment at the end of life. Among more than 900 patients with cancer, those who thought they would live for at least six months were more likely to choose curative therapy than "comfort care" compared with patients who thought there was at least a 10% chance they would not survive for six months [179].
Many studies have demonstrated high rates of aggressive treatment within the last months to weeks of life, with increased rates of hospital admissions, stays in an intensive care unit, use of medical resources, and use of chemotherapy. Goodman et al. found that patients with severe chronic disease near the end of life spent a disproportionate number of days in an intensive care unit and received care from multiple physicians; more than half of the patients saw 10 or more physicians within the last six months of life [55]. Similarly, Sheffield et al. found high rates of admission to the intensive care unit among nearly 23,000 patients with pancreatic cancer, and Unroe et al. found that 80% of more than 229,000 people with heart failure were hospitalized in the last six months of life [180,181]. In the cancer setting, several researchers have reported increased rates of chemotherapy in the last two to four weeks of life [180,182,183]. However, studies to evaluate the benefit of high-intensity treatment near the end of life have consistently found that such treatment offers no survival benefit, decreases the quality of life, and delays the use of hospice [55,80,184,185].
Before discussing treatment options, the clinician should talk to the patient to gauge his or her level of understanding of the disease and prognosis and to explore the quality-of-life factors that are most important [186]. The clinician should frame the conversation to focus on active interventions rather than the end of curative therapy; should focus on the overall care goals; and should discuss options within the context of these goals (that is, does the patient wish to enroll in hospice, enroll in a phase I trial, or be present at a family event?) [81,117]. The discussion should include an explanation of the likelihood of achieving the patient's goals with each option and a comparison of the risks, benefits, and costs of each option, noting the overall lack of benefit of aggressive treatment [187,188]. It is also important to allow the patient and family enough time to express emotion and concerns and to ask questions [117,164,189]. Because frequent exacerbations in organ-failure diseases are usually predictive of a more rapid decline, hospitalizations for disease exacerbation should prompt discussions about changes in prognosis and treatment goals and advance care planning [101,190,191]. Admission to the hospital or intensive care unit should also prompt a discussion of goals and preferences with patients with cancer; this conversation should be documented within 48 hours after admission [161]. The ACCP recommends a discussion of the pros and cons of life-sustaining treatment when caring for patients with advanced lung cancer [54].
When the patient, family, and/or healthcare team do not agree on the benefit/utility of interventions, the clinician should consider consulting with social workers or pastoral care services to help with conflict resolution [187]. In addition, the clinician should explain to patients that the likelihood of insurance coverage for a treatment is low if it is not medically indicated [188].
Clinical guidelines have begun to address the use of aggressive treatment at the end of life. The ACCF/AHA guideline on the management of heart failure notes that it is not appropriate to carry out aggressive procedures in the last several months of life if they do not contribute to recovery or improve quality of life (including intubation and implantation of a cardiac defibrillator) [108]. In addition, discussion of device deactivation for patients with refractory heart failure is recommended [159]. The Renal Physicians Association recommends forgoing dialysis for patients with chronic kidney disease or end-stage renal disease who have "very poor prognosis" [121]. The increased use of chemotherapy near the end of life has led oncology experts to recommend more judicious use of chemotherapy. Oncologists have called for the discontinuation of chemotherapy when the chance of success is minimal, such as when disease progresses after three consecutive regimens [178,192].
Early discussion of preferences for life-sustaining measures is especially important. It is estimated that roughly 75% of patients will be unable to participate in some or all of the decisions pertaining to their care at the end of life [193,194]. Documentation of preferences helps to inform decision making by the physician and the patient's health care proxy (surrogate decision maker). Clinicians should encourage their patients to designate a healthcare proxy early in the course of a life-limiting disease [62,82,122]. Patients should be urged to clarify their wishes with their chosen health proxy, as a proxy often inaccurately predicts a patient's wishes or may have values that conflict with those of the patient [194].
Advance directives, designation of a healthcare proxy, do-not-resuscitate (DNR) orders, and living wills were developed as a way to ensure that patients received care that was consistent with their preferences and goals. Advance directives offer many benefits; they have been associated with a lower likelihood of in-hospital deaths, an increased use of hospice, and a significant reduction in costs [195]. Although early studies showed that advance directives did not always translate into patients receiving their preferred level of care, later studies have demonstrated that most patients with advance directives do receive care consistent with their preferences, especially if they want limited care (rather than "all possible" care) [194,196].
The American College of Physicians recommends that clinicians ensure that patients with "serious illness" engage in advance care planning, including the completion of advance directives [47]. Clinicians must emphasize the value of advance directives because most patients have not completed them. An estimated 20% of the population have written advance directives, with higher rates among the older population and nursing home residents and lower rates among minority populations and those with nonmalignant life-limiting diseases (compared with people with cancer) [197,198,199,200,201]. Other guidelines recommend that advance care planning be done early in the course of disease, to help avoid potential compromise of decision-making capacity near the end of life [62,108,121,122].
In preparing for a discussion about advance directives, clinicians should ask the patient if he or she wishes to have other family members present during the conversation. This is especially important for patients of some cultural backgrounds, as healthcare decisions are the responsibility of family members in many cultures [200]. Increased efforts should be aimed at obtaining advance directives from patients of minority races/ethnicities. Although the rate of advance directives is higher in the gay and lesbian community than in the general population, clinicians should emphasize the importance of these documents to gay and lesbian patients to ensure that the patient's wishes are carried out and to avoid legal consequences for the patient's partner [202].
DNR orders and living wills have limitations and have been open to interpretation, which has led to the development of medical order forms based on patients' preferences. Developed at the Oregon Health & Science University, the Physicians Orders for Life-Sustaining Treatment (POLST) program is designed to ensure that a patient's preferences regarding cardiopulmonary resuscitation, scope of treatment, artificial nutrition by tube, and use of antibiotics (in some states) can be followed, regardless of where the patient receives care [203]. Nearly all states have an endorsed POLST program or one in development [203]. A POLST does not replace a traditional advance directive, and when available, an advance directive should accompany the POLST form [203]. Early studies have demonstrated that the use of POLST has led to higher rates of meeting patients' preferences [204,205].
Legal issues related to advance directives and POLSTs vary according to state, and clinicians should be familiar with the law in the state in which they practice [197].
The NCP consortium published an update of its Clinical Practice Guidelines for Quality Palliative Care in 2018, a copy of which is available online [6]. The guidelines are applicable for both specialty and primary palliative care and are organized in reference to the same eight domains used in past editions. New themes emphasized in each domain include comprehensive assessment, family caregiver support and education, care coordination, and culturally inclusive care [6]. The ICSI also provides guidelines for palliative care, including an algorithm for overall care, with details on the management of several specific symptoms [113]. Other general guidelines for palliative care have been developed by the International Association for Hospice and Palliative Care, now in its third edition [206].
Despite these resources, there is limited guidance on the treatment of specific symptoms in disease settings other than cancer. As a way to heighten awareness of the need for improved palliative care across disease settings, researchers began to document the prevalence of symptoms among groups of patients as well as compare the prevalence and severity of symptoms with those found among patients with cancer. Studies have documented that the symptom burden at the end of life for patients with life-limiting diseases is often as high as—or higher than—that for patients with cancer, and the most common symptoms are similar across disease settings (Table 7) [122,201,207,208,209,210,211].
MOST COMMON SYMPTOMS AT THE END OF LIFE ACROSS LIFE-LIMITING DISEASE SETTINGS
| Overall |
| |||||
| Cancer |
| |||||
| Heart failure |
| |||||
| COPD |
| |||||
| Renal disease |
| |||||
| End-stage liver disease |
| |||||
| HIV/AIDS |
|
In the wake of such studies, the American College of Physicians published a clinical practice guideline on palliative care interventions for three symptoms with the overall strongest evidence—pain, dyspnea, and depression—and evidence-based guidelines and recommendations for palliative care have been developed for respiratory diseases, heart failure, and end-stage renal disease [47,108,121,122,212,213,214]. These guidelines represent an important step toward enhancing palliative care, but more work is needed in many disease settings to address all aspects of palliative care. For one, definitions in palliative and supportive care are not standardized and remain a significant barrier to improvement [215].
Among patients with life-limiting illness who receive palliative care consultation, physical symptoms are cited as causing the greatest distress [216]. Patients usually have multiple symptoms, and a mean of nine to 11 symptoms per patient has been reported [207,208,209,217]. The presence of multiple symptoms can create challenges in identifying causes, as many symptoms are intricately linked with others, including symptoms in the psychosocial domain.
Several tools have been developed to assess factors in the end-of-life experience, including five tools to evaluate physical symptoms (three of which are used to assess pain), four to assess quality of life, and six to assess functional status [218]. However, a systematic review of 99 tools in these three domains plus six others (emotional and cognitive symptoms, advance care planning, continuity of care, spirituality, grief and bereavement, satisfaction and quality of care, and caregiver well-being) showed that data on the reliability and validity were lacking for most of the tools [219]. Assessment of symptoms should include comprehensive documentation of the patient's history and findings on physical examination and should be carried out at regular intervals [6]. To help ensure that patients' physical distress is alleviated, when clinicians ask patients about the presence and severity of symptoms, they should also ask which symptom is most troublesome, as patients do not often specifically state this [220].
Although asking open-ended questions about symptoms is helpful, systematic assessment of symptoms is also necessary. A study of patients in a palliative medicine program demonstrated that significantly more symptoms were identified on systematic assessment than through open-ended questioning (2,075 symptoms compared with 325) [221]. The symptoms that went unreported were not inconsequential; of those symptoms not initially volunteered by the patient, 69% were rated as "severe" and 79% were described as "distressing" [221]. Studies have demonstrated that patients are often reluctant to report worsening symptoms because of fear that they indicate progressive disease. Clinicians should describe potential symptoms to help patients and family understand which symptoms can be expected and when it is appropriate to notify a member of the healthcare team. It is important for the healthcare team to acknowledge the patient's symptoms as real and to take prompt actions to relieve them adequately. The patient's comfort should take precedence over the exact cause of the symptom. Diagnostic studies to determine the cause of symptoms should be undertaken only if the results will substantially help in directing effective treatment. The risks, benefits, costs, and options for treating an underlying cause should be discussed with the patient and family and considered within the context of the patient's culture, belief system, and expectations.
An important contribution of palliative care is the commitment to explore sources of suffering other than merely the physical aspects. Serious illness inevitably leads to an array of thoughts, feelings, fears about the future, and an erosion of capacity for work and other activities that give life meaning and purpose. Thus, in addition to pharmacologic treatment of physical symptoms, nonpharmacologic strategies are needed to augment therapy and to address the sensory, cognitive, affective, and functional components of illness [67]. The healthcare team should talk to the patient and family about priorities for pharmacologic versus nonpharmacologic treatments. Although data are limited on some nonpharmacologic interventions, many patients have benefited from these approaches. As research expands in the field of palliative care, other innovative strategies are being scientifically evaluated, and results are sometimes conflicting. Nonpharmacologic measures should be carried out in conjunction with pharmacologic management before medications fail to provide relief, as interventions, especially cognitive/behavioral techniques, are more effective when symptoms are acute and/or mild.
Once the patient's needs have been assessed, the palliative care team should work with the patient (and family) to develop priorities and goals of care [113]. Continual reassessment of symptoms and periodic review and documentation of the patient's goals and care plan are necessary to ensure that his or her needs are met [113]. It may be helpful for patients or a family member to keep a pain or symptom diary to note which measures have or have not provided relief and the duration of relief. This information will help clinicians determine the efficacy of specific therapeutic options and modify the treatment plan as necessary.
The discussion of interventions that follows focuses on the care of adults. Palliative care for children is addressed later in this course.
Unrelieved pain is the greatest fear among people with a life-limiting disease, and the need for an increased understanding of effective pain management is well-documented [222]. Although experts have noted that 75% to 90% of end-of-life pain can be managed effectively, rates of pain are high, even among people receiving palliative care [47,126,187,207,209,217,222,223,224,225].
The inadequate management of pain is the result of several factors related to both patients and clinicians. In a survey of oncologists, patient reluctance to take opioids or to report pain were two of the most important barriers to effective pain relief [226]. This reluctance is related to a variety of attitudes and beliefs [222,226]:
Fear of addiction to opioids
Worry that if pain is treated early, there will be no options for treatment of future pain
Anxiety about unpleasant side effects from pain medications
Fear that increasing pain means that the disease is getting worse
Desire to be a "good" patient
Concern about the high cost of medications
Education and open communication are the keys to overcoming these barriers. Every member of the healthcare team should reinforce accurate information about pain management with patients and families. The clinician should initiate conversations about pain management, especially regarding the use of opioids, as few patients will raise the issue themselves or even express their concerns unless they are specifically asked [227]. It is important to acknowledge patients' fears individually and provide information to help them differentiate fact from fiction. For example, when discussing opioids with a patient who fears addiction, the clinician should explain that the risk of addiction is low [222]. It is also helpful to note the difference between addiction and physical dependence.
There are several other ways clinicians can allay patients' fears about pain medication:
Assure patients that the availability of pain relievers cannot be exhausted; there will always be medications if pain becomes more severe.
Acknowledge that side effects may occur but emphasize that they can be managed promptly and safely and that some side effects will abate over time.
Explain that pain and severity of disease are not necessarily related.
Encouraging patients to be honest about pain and other symptoms is also vital. Clinicians should ensure that patients understand that pain is multidimensional and emphasize the importance of talking to a member of the healthcare team about possible causes of pain, such as emotional or spiritual distress. The healthcare team and patient should explore psychosocial and cultural factors that may affect self-reporting of pain, such as concern about the cost of medication.
Clinicians' attitudes, beliefs, and experiences also influence pain management, with addiction, tolerance, side effects, and regulations being the most important concerns [222,223,226,228,229,230]. A lack of appropriate education and training in the assessment and management of pain has been noted to be a substantial contributor to ineffective pain management [226,228,230,231]. As a result, many clinicians, especially primary care physicians, do not feel confident about their ability to manage pain in their patients [226,228].
Clinicians require a clear understanding of available medications to relieve pain, including appropriate dosing, safety profiles, and side effects. If necessary, clinicians should consult with pain specialists to develop an effective approach.
Legal and Ethical Issues Related to the Treatment of Pain
Fear of license suspension for inappropriate prescribing of controlled substances is also prevalent, and a better understanding of pain medication will enable physicians to prescribe accurately, alleviating concern about regulatory oversight. Physicians must balance a fine line; on one side, strict federal regulations regarding the prescription of schedule II opioids (morphine, oxycodone, methadone, hydromorphone) raise fear of Drug Enforcement Administration investigation, criminal charges, and civil lawsuits [222,232]. Careful documentation on the patient's medical record regarding the rationale for opioid treatment is essential [232]. On the other side, clinicians must adhere to the American Medical Association's Code of Ethics, which states that failure to treat pain is unethical. The code states, in part: "Physicians have an obligation to relieve pain and suffering and to promote the dignity and autonomy of dying patients in their care. This includes providing effective palliative treatment even though it may foreseeably hasten death" [233]. In addition, the American Medical Association Statement on End-of-Life Care requires that physicians "reassure the patient and/or surrogate that all other medically appropriate care will be provided, including aggressive palliative care and appropriate symptom management, if that is what the patient wishes" [234].
Physicians should consider the legal ramifications of inadequate pain management and understand the liability risks associated with both inadequate treatment and treatment in excess. The undertreatment of pain carries a risk of malpractice liability, and this risk is set to increase as the general population becomes better educated about the availability of effective approaches to pain management at the end of life. Establishing malpractice requires evidence of breach of duty and proof of injury and damages. Before the development of various guidelines for pain management, it was difficult to establish a breach of duty, as this principle is defined by nonadherence to the standard of care in a designated specialty. With such standards now in existence, expert medical testimony can be used to demonstrate that a practitioner did not meet established standards of care for pain management. Another change in the analysis of malpractice liability involves injury and damages. Because pain management can be considered as separate from disease treatment and because untreated pain can lead to long-term physical and emotional damage, claims can be made for pain and suffering alone, without wrongful death or some other harm to the patient [235].
The proper storage and disposal of prescription pain medications should also be considered. Taking steps to ensure that medications are stored and destroyed securely and safely can help prevent unintended overdose and substance abuse. In 2010, the U.S. Senate passed the Secure and Responsible Drug Disposal Act, which amended the Controlled Substances Act to permit the take-back disposal of medications by authorized persons (rather than the patient with the prescription) [236]. As such, healthcare professionals may be required to dispose of drugs returned by patients in addition to drug samples that have expired or are not being dispensed. For best practice guidelines on the disposal of medications by patients or healthcare professionals, please visit the Drug Enforcement Administration Office of Diversion Control at https://www.deadiversion.usdoj.gov/drug_disposal/drug-disposal.html [237].
Patients with History of Substance Abuse
The population of people with a history of substance abuse presents challenges to the effective use of pain medication, with issues related to trust, the appropriate use of pain medications, interactions between illicit drugs and treatment, and compliance with treatment. The issues differ depending on whether substance abuse is a current or past behavior.
With active substance abusers, it is difficult to know if patients' self-reports of pain are valid or are drug-seeking behaviors. It has been recommended that, as with other patients at the end of life, self-reports of pain should be believed [67,227]. A multidisciplinary approach, involving15 psychiatric professionals, addiction specialists, and, perhaps, a pain specialist, is necessary. To decrease the potential for the patient to seek illicit drugs for pain, an appropriate pain management plan should be implemented, and the patient should be reassured that pain can be managed effectively [67,227]. When planning treatment, the patient's tolerance should be considered; higher doses may be needed initially, and doses can be reduced once acute pain is under control. Long-acting pain medications are preferred for active substance abusers, and the use of nonopioids and co-analgesics can help minimize the use of opioids. Setting limits as well as realistic goals is essential and requires establishing trust and rapport with the patient and caregivers.
Establishing trust is also essential for patients with former substance abuse behavior, who often must be encouraged to adhere to a pain management program because of their fears of addiction. Involving the patient's drug counselor is beneficial, and other psychological clinicians may be helpful in assuring the patient that pain can be relieved without addiction. Recurrence of addiction is low, especially among people with cancer, but monitoring for signs of renewed abuse should be ongoing [227].
Patients who are following a methadone maintenance program may also fear effective pain management as a risk for recurrent abuse. Two approaches may be followed for these patients: they may receive an increased dose of methadone as the pain reliever or they may be given other opioids along with the same methadone dose, with the dose of the opioid titrated for effective pain relief [67,227]. Again, involvement of the drug counselor is important.
The prevalence of pain at the end of life has been reported to range from 8% to 96%, occurring at higher rates among people with cancer than among adults with other life-limiting diseases [211,238].
Pain can be caused by a multitude of factors and is usually multidimensional, with pain frequently being exacerbated by other physical symptoms and by psychosocial factors, such as anxiety or depression [223].
Pain should be assessed routinely, and frequent assessment has become the standard of care [223]. Pain is a subjective experience, and multidimensional in nature, and although patients' self-reporting of pain does not always correlate with objective functional measures, the patient's self-report of pain is the most reliable indicator [239,240]. Research has shown that pain is underestimated by healthcare professionals and overestimated by family members [223,241]. Therefore, it is essential to obtain a pain history directly from the patient, when possible, as a first step toward determining the cause of the pain and selecting appropriate treatment strategies. When the patient is unable to communicate verbally, other strategies should be used to determine the characteristics of the pain, as will be discussed.
Questions should be asked to elicit descriptions of the pain characteristics, including its location, distribution, quality, temporal aspect, and intensity. In addition, the patient should be asked about aggravating or alleviating factors. Pain is often felt in more than one area, and physicians should attempt to discern if the pain is focal, multifocal, or generalized. Focal or multifocal pain usually indicates an underlying tissue injury or lesion, whereas generalized pain could be associated with damage to the central nervous system. Pain can also be referred, usually an indicator of visceral pain.
The quality of the pain refers to the sensation experienced by the patient, and it often suggests the pathophysiology of the pain [223]. Pain that is well localized and described as aching, throbbing, sharp, or pressure-like is most likely somatic nociceptive pain. This type of pain is usually related to damage to bones and soft tissues. Diffuse pain that is described as squeezing, cramping, or gnawing is usually visceral nociceptive pain. Pain that is described as burning, tingling, shooting, or shock-like is neuropathic pain, which is generally a result of a lesion affecting the nervous system.
Temporal aspects of pain refer to its onset: acute, chronic, or "breakthrough." A recent onset characterizes acute pain, and there are accompanying signs of generalized hyperactivity of the sympathetic nervous system (diaphoresis and increased blood pressure and heart rate). Acute pain usually has an identifiable, precipitating cause, and appropriate treatment with analgesic agents will relieve the pain. When acute pain develops over several days with increasing intensity, it is said to be subacute. Episodic, or intermittent, pain occurs during defined periods of time, on a regular or irregular basis. Chronic pain is defined as pain that persists for at least three months beyond the usual course of an acute illness or injury. Such pain is not accompanied by overt pain behaviors (grimacing, moaning) or evidence of sympathetic hyperactivity.
"Breakthrough" is the term used to describe transitory exacerbations of severe pain over a baseline of moderate pain [242]. Breakthrough pain can be incident pain or pain that is precipitated by a voluntary act (such as movement or coughing) or can occur without a precipitating event. Breakthrough pain occurs in as many as 90% of people with cancer or in hospice settings and is often a consequence of inadequate pain management [222].
Documentation of pain intensity is key, as several treatment decisions depend on the intensity of the pain. For example, severe, intense pain requires urgent relief, which affects the choice of drug and the route of administration [4,223]. The numeric rating scale is the tool used most often to assess pain; with this tool, patients rate pain on a scale of 0 to 10 [223]. Visual analogue scales (patients rate pain on a line from 0 to 10) and verbal rating scales, which enable the patient to describe the pain as "mild," "moderate," or "severe," have also been found to be effective. Some patients, however, may have difficulty rating pain using even the simple scales. In an unpublished study involving 11 adults with cancer, the Wong-Baker FACES scale, developed for use in the pediatric setting, was found to be the easiest to use among three pain assessment tools that include faces to assess pain [243].
Functional assessment is important. The healthcare team should observe the patient to see how pain limits movements and should ask the patient or family how the pain interferes with normal activities. Determining functional limitations can help enhance patient compliance in reporting pain and adhering to pain-relieving measures, as clinicians can discuss compliance in terms of achieving established functional goals [227]. The Memorial Pain Assessment Card can be used to evaluate both the severity of pain and the effect of pain on function [223,244].
Physical examination can be valuable in determining an underlying cause of pain. Examination of painful areas can detect evidence of trauma, skin breakdown, or changes in osseous structures. Auscultation can detect abnormal breath or bowel sounds; percussion can detect fluid accumulation; and palpation can reveal tenderness. A neurologic examination should also be carried out to evaluate sensory and/or motor loss and changes in reflexes. During the examination, the clinician should watch closely for nonverbal cues that suggest pain, such as moaning, grimacing, and protective movements. These cues are especially important when examining patients who are unable to verbally communicate about pain.
Strong evidence supports pain management approaches for people with cancer, but the evidence base for management of pain in people with other life-limiting diseases is weak [47,54,108,187,212,214]. Effective pain management involves a multidimensional approach involving pharmacologic and nonpharmacologic interventions that are individualized to the patient's specific situation [223].
Pharmacologic Interventions
The WHO analgesic ladder, introduced in 1986 and disseminated worldwide, remains recognized as a useful educational tool but not as a strict protocol for the treatment of pain. It is intended to be used only as a general guide to pain management [245]. The three-step analgesic ladder designates the type of analgesic agent based on the severity of pain (Figure 6) [245]. Step 1 of the WHO ladder involves the use of nonopioid analgesics, with or without an adjuvant (co-analgesic) agent, for mild pain (pain that is rated 1 to 3 on a 10-point scale). Step 2 treatment, recommended for moderate pain (score of 4 to 6), calls for a weak opioid, which may be used in combination with a step 1 nonopioid analgesic for unrelieved pain. Step 3 treatment is reserved for severe pain (score of 7 to 10) or pain that persists after Step 2 treatment. Strong opioids are the optimum choice of drug at Step 3. At any step, nonopioids and/or adjuvant drugs may be helpful. Some consider this model to be outdated and/or simplistic, but most agree that it remains foundational. It can be modified or revised, as needed, to apply more accurately to different patient populations.
The WHO ladder is also accompanied by five guiding principles [245]:
Reduce pain to levels that allow an acceptable quality of life.
Global assessment of the patient should guide treatment, recognizing that individuals experience and express pain differently.
The safety of patients, carers, healthcare providers, communities, and society must be assured.
A pain management plan includes pharmacologic treatments and may include psychosocial and spiritual care.
Analgesics, including opioids, must be accessible: both available and affordable.
The pharmacologic treatment of pain involves selecting the right drug(s) at the right dose, frequency, and route, and managing side effects [223]. A decision pathway was developed for use in the cancer setting and can be applied to other settings (Figure 7) [223].
Nonopioid analgesics, such as aspirin, acetaminophen (Tylenol), and nonsteroidal anti-inflammatory drugs (NSAIDs), are primarily used for mild pain (Step 1 of the WHO ladder) and may also be helpful as co-analgesics at Steps 2 and 3. Acetaminophen is among the safest of analgesic agents, but it has essentially no anti-inflammatory effect. Toxicity is a concern at high doses, and the maximum recommended dose is 3–4 g per day [223]. Acetaminophen should be avoided or given at lower doses in people with a history of alcohol abuse or renal or hepatic insufficiency [223].
NSAIDs are most effective for pain associated with inflammation. Among the commonly used NSAIDs are ibuprofen (Motrin, Advil), naproxen (Aleve, Naprosyn), and indomethacin (Indocin). There are several classes of NSAIDs, and the response differs among patients; trials of drugs for an individual patient may be necessary to determine which drug is most effective [67]. NSAIDs inhibit platelet aggregation, increasing the risk of bleeding, and also can damage the mucosal lining of the stomach, leading to gastrointestinal bleeding. There is a ceiling effect to the nonopioid analgesics; that is, there is a dose beyond which there is no further analgesic effect. In addition, many side effects of nonopioids can be severe and may limit their use or dosing.
Moderate pain (Step 2) has often been treated with analgesic agents that are combinations of acetaminophen and an opioid, such as codeine, oxycodone, or hydrocodone. However, it is now recommended that these combination drugs be avoided, as limits on the maximum dose of acetaminophen limits the use of a combination drug [206,223]. Individual drugs in combination is preferred, allowing for increases in the dose of the opioid without increasing the dose of the co-analgesic.
Strong opioids are used for severe pain (Step 3). Guidelines suggest that the most appropriate opioid dose is the dose required to relieve the patient's pain throughout the dosing interval without causing unmanageable side effects [187,206,246]. Morphine, buprenorphine, oxycodone, hydromorphone, fentanyl, and methadone are the most widely used Step 3 opioids in the United States. Unlike nonopioids, opioids do not have a ceiling effect, and the dose can be titrated until pain is relieved or side effects become unmanageable. For an opioid-naïve patient or a patient who has been receiving low doses of a weak opioid, the initial dose of a Step 3 opioid should be low, and, if pain persists, the dose may be titrated up daily until pain is controlled. Opioid-naïve patients are those who are not receiving opioid analgesic daily and therefore have not developed significant tolerance. Opioid-tolerant patients are those who have been taking an opioid analgesic daily for at least one week. The FDA identifies tolerance as receiving at least 60 mg of morphine daily, 30 mg of oral oxycodone daily, 8 mg of oral hydromorphone daily, or an equianalgesic dose of another opioid for one week or longer [187]. Typical starting doses for patients who are opioid-naïve have been noted, but these doses should be used only as a guide, and the initial dose, as well as titrated dosing, should be done on an individual basis (Table 8).
OPIOIDS FOR THE MANAGEMENT OF PAIN IN ADULTSa
| Drug | Typical Starting Doseb | Onset of Action | Duration of Action | ||
|---|---|---|---|---|---|
| Codeine | 15–60 mg | 30 to 60 minutes | 4 to 6 hours | ||
| Hydrocodone | 2.5–10 mg | 10 to 20 minutes | 4 to 8 hours | ||
| Morphine, immediate release | 15–30 mg | 15 to 30 minutes or 5 to 10 minutes | 3 to 6 hours | ||
| Oxycodone, immediate release | 5–10 mg | 10 to 30 minutes | 3 to 4 hours | ||
| Oxymorphone, sustained release | 10 mg | 5 to 10 minutes | 8 to 12 hours | ||
| Hydromorphone | 2–4 mg | 15 to 30 minutes | 4 to 5 hours | ||
| Methadone | 5–10 mg | 30 to 60 minutes | 4 to 6 hours | ||
| Tapentadol | 50–100 mg | <60 minutes | 4 to 6 hours | ||
| Tapentadol, extended release | 50–100 mg | — | — | ||
| Fentanyl (buccal tablet) | 100–200 mcg | 5 to 15 minutes | 2 to 4 hours | ||
| Fentanyl (transdermal patch) | 25 mcg/hour (worn for 3 days) | 12 to 18 hours | 48 to 72 hours | ||
| Buprenorphine (transdermal patch) | 5–10 mcg/hour (worn for 7 days) | — | — | ||
| |||||
The most serious potential adverse effect following initiation of opioids for treatment of pain is oversedation followed by respiratory depression. To mitigate this risk, clinicians should discuss the role of naloxone administration by caregivers in the event of sedation/respiratory depression and make naloxone available as indicated or as required by local regulations [187]. When initiating morphine, or any opioid agent for treatment of moderate/severe pain, the prescribing clinician should consider lower starting dose titration in frail or older patients and in any patient with renal insufficiency (reduced creatinine clearance).
More than one route of opioid administration will be needed by many patients during end-of-life care, but in general, opioids should be given orally, as this route is the most convenient and least expensive. The transdermal route is preferred to the parenteral route, although dosing with a transdermal patch is less flexible and so may not be appropriate for patients with unstable pain [223]. Intramuscular injections should be avoided because injections are painful, drug absorption is unreliable, and the time to peak concentration is long [223].
Morphine is considered to be the first-line treatment for a Step 3 opioid [206]. Morphine is available in both immediate-release and sustained-release forms, and the latter form can enhance patient compliance. The sustained-release tablets should not be cut, crushed, or chewed, as this counteracts the sustained-release properties. Morphine should be avoided in patients with severe renal failure [214].
Buprenorphine (Butrans) has the general structure of morphine but differs from it in several ways [250]. The transdermal formulation of the drug was approved in 2010 for moderate-to-severe chronic pain in patients requiring an around-the-clock opioid for an extended period [223]. It may be used for people with renal impairment but is contraindicated in patients who have substantial respiratory depression [247,250].
The sustained-release form of oxycodone (OxyContin) has been shown to be as safe and effective as morphine for cancer-related pain, and it may be associated with less common side effects, especially hallucinations and delirium [251]. Oxycodone is also available in an immediate-release form (Roxicodone). Oxycodone should be used in people with advanced chronic kidney disease only if alternative options are not available [214]. If the drug must be used, the intervals between doses should be increased, and the patient should be monitored closely [214].
Hydromorphone and fentanyl are the most potent opioids; neither drug should be given to an opioid-naïve patient. Hydromorphone, which is four times as potent as morphine, is available in immediate- and extended-release forms [252]. Fentanyl is the strongest opioid (approximately 80 times the potency of morphine) and is available as a transdermal drug-delivery system (Duragesic; Ionsys), buccal film (Onsolis), tablet (Fentora), nasal spray (Lazanda), sublingual spray (Subsys), sublingual tablet (Abstral), and lozenge (Actiq) [247,253]. Fentanyl preparations have a more rapid onset than other opioids given nonparenterally [223]. Because of its potency, fentanyl must be used with extreme care, as deaths have been associated with its use. Physicians must emphasize to patients and their families the importance of following prescribing information closely, and members of the healthcare team should monitor the use of the drug. Fentanyl, administered subcutaneously, is the recommended choice for patients with advanced chronic kidney disease [214].
The use of methadone to relieve pain has increased substantially over the past few years, moving from a second-line or third-line drug to a first-line medication for severe pain in people with life-limiting diseases [254]. A systematic review showed that methadone had efficacy similar to that of morphine. However, the authors' conclusions were based on low-quality evidence. Other opioids (e.g., morphine, fentanyl) are easier to manage but may be more expensive than methadone in many economies [255]. Physicians must be well educated about the pharmacologic properties of methadone, as the risk for serious adverse events, including death, is high when the drug is not administered appropriately [255,256]. If the dose of methadone is increased too rapidly or administered too frequently, toxic accumulation of the drug can cause respiratory depression and death. Because of the unique nature of methadone, and its long and variable half-life, extreme care must be taken when titrating the drug, and frequent and careful evaluation of the patient is required. Practitioners are advised to consult with a pain or palliative care specialist if they are unfamiliar with methadone prescribing or if individual patient considerations necessitate rapid switching to or from methadone [187].
Meperidine (Demerol) should not be used in the palliative care setting because of limited efficacy and potential for severe toxicity. Agonist-antagonist opioids (nalbuphine [Nubain], butorphanol [Stadol], and pentazocine [Talwin]) are not recommended for use with pure opioids, as they compete with them, leading to possible withdrawal symptoms.
Tapentadol (Nucynta) is a short-acting opioid approved for moderate to severe pain in adults; an extended-release formulation (Nucynta ER) was approved in 2011 for moderate-to-severe chronic pain when an around-the-clock opioid is needed [257]. The drug is associated with a lower incidence of adverse effects than other opioids, and it has been shown to be highly effective for chronic pain conditions but has not been extensively studied in cancer-related pain or the palliative care setting [258]. A 2014 study of 123 patients that had previously received long-term analgesia for cancer-related pain showed tapentadol significantly reduced pain scores and was generally well tolerated; concomitant use of pain medications was also reduced [259].
The most appropriate option for breakthrough pain is an immediate-release opioid taken in addition to the around-the-clock regimen [223]. The fentanyl buccal tablet has been shown to be effective and safe for relieving breakthrough pain in people who are opioid tolerant [187,260,261]. Between January 2011 and January 2012, three forms of fentanyl were approved for breakthrough pain in people with cancer: fentanyl sublingual tablet (Abstral), fentanyl nasal spray (Lazanda), and fentanyl sublingual spray (Subsys). Abstral and Lazanda have since been discontinued [247,252]. As of 2021, the fentanyl lozenge (Actiq) and buccal tablet (Fentora) are also approved for breakthrough cancer pain [252]. For each formula, the initial dose may be repeated once if pain is not relieved adequately after 30 minutes. Patients should wait at least two hours before using the sublingual tablet, buccal film, or the nasal spray for another breakthrough pain episode; the interval is four hours for the sublingual spray, lozenge, or buccal tablet [247,252].
When pain responds poorly to escalated doses of an opioid, other approaches should be considered, including alternative routes of administration, use of alternate opioids (termed opioid rotation or opioid switching), use of adjuvant analgesics, and nonpharmacologic approaches. A process for opioid switching has been established (Figure 8); the first step is to calculate the equianalgesic dose of the new drug (Table 9) [187,206,223]. Additional care is needed when switching to methadone, and conversion ratios have been established (Table 10) [187]. Evidence suggests that the traditionally recommended equianalgesic doses for the fentanyl transdermal patch are subtherapeutic for patients with chronic cancer-related pain, and more aggressive approaches may be warranted (Table 11) [187,223,262].
DOSE CONVERSION RATIOS FOR METHADONE
| Oral Morphine | Conversion Ratio (Morphine:Oral Methadone) |
|---|---|
| 30–90 mg | 4:1 |
| 91–300 mg | 8:1 |
| >300 mg | 12:1 |
| 100 mcg/hour | 800 mg |
| The oral conversion ratio of methadone varies. Practitioners are advised to consult with a pain or palliative care specialist if they are unfamiliar with methadone prescribing. | |
Another approach that has been used for pain management in the cancer setting is combination opioid therapy, or the concurrent use of two strong opioids. The effectiveness of this approach has been evaluated in only two studies, and the combination was morphine and oxycodone or morphine with fentanyl or methadone [263]. The evidence to support a recommendation of combination opioid therapy is weak, and the side effects most likely outweigh the benefit [263].
Opioids are associated with many side effects, the most notable of which is constipation, occurring in nearly 100% of patients. The universality of this side effect mandates that once extended treatment with an opioid begins, prophylactic treatment with laxatives must also be initiated. Tolerance to other side effects, such as nausea and sedation, usually develops within three to seven days. Some patients may state that they are "allergic" to an opioid. It is important for the physician to explore what the patient experienced when the drug was taken in the past, as many patients misinterpret side effects as an allergy. True allergy to an opioid is rare [223]. Opioid rotation may also be done to reduce adverse events.
When opioids are prescribed, careful documentation of the patient's history, examinations, treatments, progress, and plan of care are especially important from a legal perspective. This documentation must provide evidence that the patient is functionally better off with the medication than without [67]. In addition, physicians must note evidence of any dysfunction or abuse.
Adjuvant agents are often used in conjunction with opioids and are usually considered after the use of opioids has been optimized [67]. The primary indication for these drugs is adjunctive because they can provide relief in specific situations, especially neuropathic pain. Examples of adjuvant drugs are tricyclic antidepressants, anticonvulsants, muscle relaxants, and corticosteroids (Table 12) [187,223]. A systematic review found that there was limited evidence to support the use of selective serotonin reuptake inhibitors (SSRIs) for neuropathic pain, but one serotonin-norepinephrine reuptake inhibitor, venlafaxine (Effexor), was found to be effective [264].
ORAL ADJUVANT ANALGESICS
| Drug Class | Drug | Typical Starting Dose | Usual Effective Dose | |||
|---|---|---|---|---|---|---|
| Anticonvulsants | Gabapentin | 100–300 mg once daily | 300–1,200 mg (2 or 3 divided doses) | |||
| Pregabalin | 25–75 mg twice daily | 75–200 mg (3 divided doses) | ||||
| Carbamazepine | 50–100 mg twice daily | 300–600 mg twice daily | ||||
| Topiramate | 25–50 mg daily | 50–200 mg twice daily | ||||
| Oxcarbazepine | 150–300 mg twice daily | 150–600 mg twice daily | ||||
| Tiagabine | 4 mg at bedtime | 4–12 mg twice daily | ||||
| Tricyclic antidepressants |
| 10–25 mg at bedtime | 50–150 mg at bedtime | |||
| Serotonin-norepinephrine reuptake inhibitors | Venlafaxine | 37.5 mg daily | 150–350 mg daily | |||
| Skeletal muscle relaxants | Baclofen | 5 mg twice daily | 10–20 mg 2 or 3 times daily | |||
| Cyclobenzaprine | 5 mg 3 times daily | 10–20 mg 3 times daily | ||||
| Metaxalone | 400 mg 3 times daily | Not defined | ||||
| Corticosteroids | Dexamethasone | 1–2 mg | Not defined |
Nonpharmacologic Interventions
Several nonpharmacologic approaches are therapeutic complements to pain-relieving medication, lessening the need for higher doses and perhaps minimizing side effects. These interventions can help decrease pain or distress that may be contributing to the pain sensation. Approaches include palliative radiotherapy, complementary/alternative methods, manipulative and body-based methods, and cognitive/behavioral techniques. The choice of a specific nonpharmacologic intervention is based on the patient's preference, which, in turn, is usually based on a successful experience in the past.
Palliative radiotherapy is effective for managing cancer-related pain, especially bone metastases [47,265,266]. Bone metastases are the most frequent cause of cancer-related pain; 50% to 75% of patients with bone metastases will have pain and impaired mobility [265]. External-beam radiotherapy is the mainstay of treatment for pain related to bone metastases. At least some response occurs in 70% to 80% of patients, and the median duration of pain relief has been reported to be 11 to 24 weeks [265]. It takes one to four weeks for optimal therapeutic results [265,266].
However, palliative radiotherapy has become a controversial issue. Although the benefits of palliative radiotherapy are well documented and most hospice and oncology professionals believe that palliative radiotherapy is important, this treatment approach is offered at approximately 24% of Medicare-certified freestanding hospices, with less than 3% of hospice patients being treated [77,78,79]. As previously noted, reimbursement issues present a primary barrier to the use of palliative radiotherapy [77,78,79]. Among other barriers are short life expectancy, transportation issues, patient inconvenience, and lack of knowledge about the benefits of palliative radiotherapy in the primary care community [77,78,266,267].
One study found that more than half (54%) of people use complementary/alternative medicine therapies at the end of life [268]. The most commonly used therapies are massage, music, relaxation techniques, and acupuncture [268,269,270,271,272].
Massage, which can be broadly defined as stroking, compression, or percussion, has led to significant and immediate improvement in pain in the hospice setting [273]. Both massage and vibration are primarily effective for muscle spasms related to tension or nerve injury, and massage can be carried out with simultaneous application of heat or cold. Massage may be harmful for patients with coagulation abnormalities or thrombophlebitis [227].
Focused relaxation and breathing can help decrease pain by easing muscle tension. Progressive muscle relaxation, in which patients follow a sequence of tensing and relaxing muscle groups, has enabled patients to feel more in control and to experience less pain and can also help provide distraction from pain. [227]. This technique should be avoided if the muscle tensing will be too painful.
Acupuncture typically provides pain relief 15 to 40 minutes after stimulation. Relief seems to be related to the release of endorphins and a susceptibility to hypnosis [227]. The efficacy of acupuncture for relieving pain has not been proven, as study samples have been small. However, acupuncture has been found to be of some benefit for cancer-related pain when the therapy is given in conjunction with analgesic therapy [274].
Other nonpharmacologic interventions that have been helpful for some patients but lack a strong evidence base include manipulative and body-based methods (such as application of cold or heat, and positioning), yoga, distraction, and music or art therapy. The application of cold and heat are particularly useful for localized pain and have been found to be effective for cancer-related pain caused by bone metastases or nerve involvement, as well as for prevention of breakthrough incident pain [227]. Alternating application of heat and cold can be soothing for some patients, and it is often combined with other nonpharmacologic interventions.
Cold can be applied through wraps, gel packs, ice bags, and menthol. It provides relief for pain related to skeletal muscle spasms induced by nerve injury and inflamed joints. Cold application should not be used for patients with peripheral vascular disease. Heat can be applied as dry (heating pad) or moist (hot wrap, tub of water) and should be applied for no more than 20 minutes at a time, to avoid burning the skin. Heat should not be applied to areas of decreased sensation or with inadequate vascular supply, or for patients with bleeding disorders.
Changing the patient's position in the bed or chair may help relieve pain and also helps minimize complications such as decubitus ulcers, contractures, and frozen joints. Members of the healthcare team as well as family members and other informal caregivers can help reposition the patient for comfort and also perform range-of-motion exercises. Physical and occupational therapists can recommend materials, such as cushions, pillows, mattresses, splints, or support devices.
Hatha yoga is the branch of yoga most often used in the medical context, and it has been shown to provide pain relief for patients who have osteoarthritis and carpal tunnel syndrome but it has not been studied in patients at the end of life. Yoga may help relieve pain indirectly in some patients through its effects on reducing anxiety, increasing strength and flexibility, and enhancing breathing [275]. Yoga also helps patients feel a sense of control.
Methods to provide distraction from pain come in a wide variety of methods, including reciting poetry, meditating with a calm phrase, watching television or movies, playing cards, visiting with friends, or participating in crafts.
Music therapy and art therapy are also becoming more widely used as nonpharmacologic options for pain management. Listening to music has been shown to decrease the intensity of pain and reduce the amount of opioids needed, but the magnitude of the benefit was small [276]. Research suggests that art therapy contributes to a patient's sense of well-being [277]. Creating art helps patients and families to explore thoughts and fears during the end of life. An art therapist can help the creators reflect on the implications of the art work. Art therapy is especially helpful for patients who have difficulty expressing feelings with words, for physical or emotional reasons.
Fatigue is a subjective feeling of tiredness, weariness, and lack of energy. Fatigue is often accompanied by a feeling of weakness (asthenia), which can be either generalized or localized. The National Comprehensive Cancer Network (NCCN) defines fatigue as "a distressing, persistent, subjective sense of physical, emotional, and/or cognitive tiredness or exhaustion…that is not proportional to recent activity and interferes with usual functioning" [278]. Fatigue associated with life-limiting diseases is further characterized by the disproportionate relationship to recent activity and the lack of recovery following additional sleep [279]. Persistent fatigue has a significant impact on the quality of life by negatively affecting functional status, interfering with normal activities, and contributing to emotional distress [278]. Fatigue may also cause distress for a patient's family members, who may interpret this symptom as a sign of the patient "giving up." As is the case with pain, fatigue is underreported, underdiagnosed, and undertreated [279]. Studies have indicated that approximately half of patients do not report fatigue to their healthcare team, and the primary reasons were that they did not think effective treatments were available and their physicians did not offer interventions [280].
Fatigue is often part of a cluster of symptoms that may also include pain, depression, sleep disturbances, and anxiety/depression, especially at the end of life [278,281,282,283,284]. Analysis of 25 symptoms among 922 patients with advanced cancer demonstrated seven clusters. One of those clusters, referred to as the fatigue/anorexia-cachexia cluster, was composed of easy fatigue, weakness, lack of energy, anorexia, early satiety, weight loss, dry mouth, and taste changes [285]. Fatigue has often been reported to be the symptom that causes patients the most distress [286].
A sense of fatigue and weakness is one of the most common symptoms near the end of life, and patients often consider this symptom to be more troublesome than pain [287,288]. The prevalence of fatigue has been reported to range from 12% to 97% of patients with life-limiting diseases, and the prevalence is fairly consistent across disease settings [211,279].
Among the most common contributors to fatigue in people with advanced life-limiting diseases are medications, anemia, dehydration, direct tumor effects on energy consumption and supply, infection, metabolic disturbances, fluid and electrolyte imbalance, dyspnea, sleep apnea, depression, and loss of skeletal muscle due to cachexia [108,278,279].
Ensuring adequate management of symptoms related to fatigue may help in preventing the condition. Clinicians should advise the patient to conserve energy as much as possible, to follow a normal sleep cycle, and to engage in aerobic exercise [108,278,279,286].
Assessing fatigue can be a challenge, but as with pain, the patient's report of how he or she is feeling is the gold standard in the assessment. For patients who speak a language other than English, questions about fatigue should include such words and phrases as "tired," "weak," and "lack of energy," as the word "fatigue" may translate differently in some languages [279]. Several tools are available to assess fatigue, but because it usually occurs in a cluster of symptoms, many of these tools are multidimensional instruments, often involving several questions, which can be impractical [279,284]. In assessing patients for fatigue, the clinician should ask such questions as "Do you feel unusually tired or weak?" or "How tired/weak are you?" [279].
An easy-to-use instrument is the Brief Fatigue Inventory, which includes nine items that ask the patient to rate the severity of fatigue on a scale of 0 (no fatigue) to 10 ("as bad as you can imagine") [289]. The patient is asked to consider the current level of fatigue as well as fatigue experienced within the past 24 hours and to indicate the degree to which fatigue has interfered with activities, mood, walking ability, relations with other people, and enjoyment of life.
Assessment should also include a physical examination to detect an underlying cause of fatigue, a focused history-taking, and laboratory tests, as appropriate, to rule out suspected causes (Figure 9) [279].
Little evidence is available to support guidelines for the management of fatigue during the end of life. Most of the research on nonpharmacologic and pharmacologic treatment options has been conducted with subjects receiving active cancer treatment or long-term follow-up care after cancer treatment. Fatigue in the palliative care setting is addressed specifically by the European Association for Palliative Care (EAPC) (all settings) and the NCCN (cancer setting) and is noted in guidelines for palliative care for advanced heart failure [108,187,279]. In addition, the Agency for Healthcare Research and Quality has addressed fatigue in the cancer setting, and systematic reviews have been done to help determine effective pharmacologic and nonpharmacologic interventions [281,290,291,292,293]. Management of fatigue should include treatment of an underlying cause, if one can be identified, but symptomatic relief should also be provided (Figure 10) [108,187,279].
When medications are the underlying cause of the fatigue, nonessential medications should be discontinued, and changing medications or the time of dosing may reduce tiredness during the day. Appropriate management of infection, cachexia, depression, and insomnia may also help reduce fatigue [279,287]. The patient's life expectancy and preferences should be considered before carrying out treatment of an underlying cause [279]. Fatigue may provide a protective effect for patients in the last days or hours of life [279]. As such, the patient may be more comfortable without aggressive treatment of fatigue during that period [279].
The treatment of anemia as an underlying cause of fatigue (and other symptoms) is a complex issue. Many studies have provided evidence to recommend the use of erythropoiesis-stimulating agents (erythropoietin [Epogen], darbepoetin [Procrit]) for anemia in people with cancer, HIV/AIDS, chronic kidney disease, and heart failure because of benefit in increasing the hemoglobin level, improving exercise tolerance, reducing symptoms, and decreasing the need for blood transfusions [279; 290; 294; 295; 296]. However, safety concerns led the U.S. Food and Drug Administration (FDA) to require a boxed warning on the label of erythropoiesis-stimulating agents regarding the increased risk of several adverse events (death, myocardial infarction, stroke, venous thromboembolism, thrombosis of vascular access, and tumor progression or recurrence) among people with chronic kidney disease or cancer [297]. The FDA recommends using the lowest dose sufficient to avoid red blood cell transfusion [297]. Recommendations for these agents in these populations have been withdrawn or revised [87; 291; 298; 299]. A 2010 systematic review and meta-analysis (11 studies, 794 subjects) demonstrated benefit of erythropoiesis-stimulating agents among people with heart failure and mild anemia (>10 g/dL) with no increase in adverse events [296].
Most patients will try to manage fatigue by resting and/or sleeping more often, and many healthcare professionals will also recommend this strategy. However, additional rest and/or sleep usually does not restore energy in patients who have fatigue related to a life-limiting disease; continued lack of exercise may even promote fatigue [279]. Regular aerobic exercise and strength training has been found to alleviate fatigue, although much of the research in this area has been conducted with cancer survivors [284]. For example, a meta-analysis (28 studies, 2,083 subjects) demonstrated a significant effect of exercise in the treatment of fatigue during and after cancer treatment [293]. An update to this review and meta-analysis supported the benefit of aerobic exercise for individuals with cancer-related fatigue and recommended further research to determine the optimal type, intensity, and timing of an exercise intervention [300]. Some small studies of fatigue have been done in the palliative care setting, and exercise was found to be beneficial [301,302,303].
Although an exercise program is recommended, decreasing activity to conserve energy is also encouraged [108,187,279]. Clinicians should talk to the patient and family about the importance of the patient conserving energy by adjusting daily activities to correspond to times of peak energy, setting priorities for activities, following a normal wake-sleep cycle, and using assistive devices, and delegating less important tasks [187,279]. Encouraging adequate nutrition, stress reduction through meditation or relaxation techniques, and engagement in enjoyable activities can help restore energy [187,279]. Counseling about setting realistic goals for activities and function may also help patients and family members adapt to new daily routines.
Pharmacologic treatment of fatigue should be undertaken only after potential causes of fatigue have been ruled out [187,279]. The EAPC and the ASCO note that methylphenidate (Ritalin) and modafinil (Provigil) may reduce fatigue [279,284]. The NCCN does not recommend modafinil due to limited evidence of benefit and recommends that methylphenidate be used cautiously and should be considered only after other causes of fatigue have been ruled out [278]. The recommendations from the EAPC and the ASCO are based on systematic reviews showing a significant effect of methylphenidate for the treatment of fatigue in people with cancer or HIV/AIDS or for opioid-induced sedation [279,290,291,292,304]. An optimal dose of methylphenidate has not been defined, but an initial dose of 5–10 mg (given in the morning) has been used, with the dose titrated to 40–60 mg per day (given once in the morning and once at midday) [279]. Among the side effects are nervousness, jitteriness, agitation, arrhythmia, and tachycardia [279]. The initial recommended dose of modafinil is 200 mg per day [279]. Major side effects have included agitation, nervousness, sleep disturbances, nausea, and diarrhea. Since the publication of these recommendations, researchers conducting a systematic review concluded that the evidence was insufficient to recommend a specific drug for the treatment of fatigue in the palliative care setting [292]. The ASCO notes that evidence for their use is weak; others argue that an improper (too low) dose and short study duration leads to suboptimal effect in trials and that individual response to central nervous system stimulants is highly variable [284,305].
Corticosteroids (prednisone and dexamethasone) have been used frequently to treat fatigue in the palliative care setting, but no research on their effectiveness is available [292]. These agents have provided short-term relief of fatigue and improved quality of life among people with cancer, but because of the toxicity associated with long-term use, they should be considered only at the end life or to alleviate fatigue for a well-defined goal (such as allowing the patient to attend a special event) [187,279].
Dyspnea is a subjective sense of breathlessness (extreme shortness of breath, the subjective awareness that "breathing is not working") and ranges from breathlessness on exertion to persistent, distressing breathlessness at rest or for longer periods of time. Patients may describe dyspnea as "smothering," "suffocating," or "drowning." Dyspnea can have a substantial impact on a patient's quality of life by restricting the patient's activities as well as causing distress for both patients and their families.
The prevalence of dyspnea among adults with life-limiting disease ranges from 10% to 95%, with the highest rates among people with COPD, lung cancer, and heart failure, especially in the last week of life [54,207,209,211,213,306,307].
Physical causes of dyspnea vary according to the life-limiting disease and/or comorbid conditions and include pleural effusion, airway obstruction, pulmonary embolism, pericardial effusion, and asthma [54]. Progressive dyspnea is a common feature of end-stage, diffuse metastatic carcinoma of the lung. Pain and psychological conditions such as anxiety and depression may augment the severity or prolong the duration of dyspnea [54,213].
Measures to reduce anxiety can help to prevent dyspnea or reduce its severity. In addition, patients with heart failure or lung diseases should be advised to conserve energy.
Practice guidelines recommend that clinicians regularly assess dyspnea in patients receiving end-of-life care [47,54,213]. Intercurrent, reversable causes of dyspnea include pleural/pericardial effusion and pulmonary embolism. Assessment should involve asking the patient to note the severity and/or distress related to dyspnea, as objective testing, such as respiratory rate, arterial blood gas levels, and pulse oximetry, do not always correlate with a patient's experience of shortness of breath [213]. Tools for patient-reported dyspnea include a modified Borg scale, a visual analog scale, or a numerical scale [213,308]. In addition to asking about the severity of breathlessness, the clinician should ask about other symptoms, especially concurrent chest pain, and about the activities that cause dyspnea. Patients with dyspnea often modify their activities to avoid dyspnea, so the clinician should ask the patient if he or she has changed or stopped any activities because of dyspnea [54]. Because of the link between psychological factors and dyspnea, the clinician should also evaluate the patient's psychosocial status.
Physical assessment of the patient should include evaluation of breath sounds, heart rate, respiratory rate, jugular pressure, and functional status. Select imaging studies, such as chest x-ray, chest CT, and echocardiogram, may identify a suspected, treatable cause of dyspnea [54,122].
The American College of Physicians, the American Thoracic Society, the Canadian Thoracic Society (endorsed by the ACCP), and the NCCN have developed evidence-based guidelines for the management of dyspnea [47,54,122,213,309,310]. In addition, evidence-based recommendations for managing dyspnea in people with advanced heart failure are available [108]. A stepwise approach to managing dyspnea should be taken, with the first step being treatment of the underlying cause, if one can be identified [54]. Nonpharmacologic interventions should be used first; if the response is inadequate, pharmacologic interventions may be added.
Supplemental oxygen is commonly used to treat dyspnea. Strong evidence supports the use of oxygen and pulmonary rehabilitation for dyspnea, and supplemental oxygen may provide relief of dyspnea for people with advanced lung or heart disease who have hypoxemia at rest or with minimal activity [47,54,212,213,309,310]. However, data suggest that oxygen offers no benefit to patients who do not have hypoxemia [108].
A variety of nonpharmacologic interventions have been suggested in several practice guidelines, although the evidence base varies (Table 13) [122,213,309,310]. In a systematic review of nonpharmacologic interventions and an update of that review for dyspnea in people with advanced malignant and nonmalignant diseases, there was strong evidence for chest wall vibration and neuroelectrical muscle stimulation and moderate evidence for walking aids and breathing training [311,312]. The updated review found low strength of evidence for acupuncture/acupressure, no evidence for the use of music, and insufficient evidence to recommend the use of a fan, music, relaxation, counseling and support, and psychotherapy [311,312]. A subsequent small randomized controlled trial demonstrated that a handheld fan directed at the face reduced breathlessness [313].
NONPHARMACOLOGIC INTERVENTIONS FOR DYSPNEA RECOMMENDED IN PRACTICE GUIDELINES
|
Opioids represent the primary recommended pharmacologic intervention for intractable dyspnea in people with advanced cancer and lung disease [47,213,309]. A systematic review and meta-analysis (18 randomized controlled trials) demonstrated a significant positive effect of opioids on breathlessness [315]. Guidelines recommend that oral or parenteral opioids be considered for all patients with severe and unrelieved dyspnea; nebulized opioids have not had an effect when compared with placebo [47,212,213,309]. Oral morphine is the most commonly prescribed opioid, but other opioids, such as diamorphine, dihydrocodeine, fentanyl, hydromorphone, and oxycodone, may be used [213]. The dose should be selected and titrated according to such factors as renal, hepatic, and pulmonary function and past use of opioids [213]. An oral dose of morphine of 2.5–10 mg every four hours as needed (1–5 mg intravenously) has been recommended for opioid-naïve patients [122]. Although respiratory depression is a side effect associated with opioids, especially morphine, this effect has not been found with doses used to relieve dyspnea [122,316]. Evidence-based recommendations for palliative care for people with heart failure note that diuretics represent the cornerstone of treatment of dyspnea [108]. Nitrates may also provide relief, and inotropes may be appropriate in select patients [108]. The recommendations also include the use of low-dose opioids [108].
Anxiolytics are often a recommended option for relief of breathlessness because of the association between anxiety and dyspnea. The NCCN guidelines suggest considering benzodiazepines when opioids and other nonpharmacologic measures have failed to control dyspnea [310]. However, there is little evidence that anxiolytic agents are effective for managing dyspnea associated with end-stage disease. A systematic review published in 2010 (seven studies, 200 subjects) showed that benzodiazepines had no beneficial effect on breathlessness in people with advanced cancer or COPD [317]. An update of the review included one additional study, but it did not alter the authors' original conclusion that benzodiazepines have no beneficial effect on breathlessness in these patient populations [318]. Bronchodilators and systemic corticosteroids may be helpful in relieving dyspnea in people with lung cancer and underlying obstructive airway disease [314]. Reducing excessive secretions with nonpharmacologic interventions and anti-secretory agents is often beneficial [310]. In addition, analgesics may help relieve dyspnea associated with pain.
Constipation can be defined as a reduced frequency of bowel movements and an increased stool consistency. In defining constipation in people with life-limiting disease, measurable symptoms, as well as the person's perception of constipation and the level of discomfort, are factors [319,320]. The condition may be accompanied by cramps and abdominal bloating, as well as by discomfort caused by straining and rectal pressure. The patient who complains of "constipation" should be encouraged to elaborate so that the full nature and extent of the difficulty, including associated symptoms, can be defined for that individual [319].
The prevalence of constipation among adults with life-limiting disease ranges from 8% to 70%, and constipation occurs in almost all patients taking opioids [211,227,307]. The prevalence of constipation in palliative care settings is even higher, at 30% to 90% [321].
Opioids are the primary factor in constipation in the palliative care setting, and many other prescribed drugs can contribute to constipation, including tricyclic antidepressants, antacids, antiepileptic drugs, anticholinergic agents, and antihypertensives [319]. Additional factors that may contribute to constipation are diverticuli, inflammatory bowel disease, metabolic conditions (hypercalcemia, hypokalemia, hypothyroidism, uremia), cerebral tumors, dehydration, and radiation fibrosis [319]. For patients with cancer, constipation may be directly due to tumor involvement that causes intestinal obstruction. A diet low in fiber and decreased physical activity also increase the likelihood of constipation.
Prevention of constipation is key, as prophylaxis is more effective than treatment after constipation has been identified. As such, all treatment guidelines strongly recommend that a prophylactic bowel regimen be initiated when treatment with opioids (or other constipation-causing drugs) begins [310,319,320,321]. The recommended prophylaxis is an osmotic and/or a stimulant laxative [310,319,320]. Many nonpharmacologic approaches are recommended, and patients should be encouraged to plan a diet with adequate fiber, to increase fluid intake, and to engage in physical activity, as appropriate [310,319,320,321]. Family members should be asked to help the patient comply with these measures. Ensuring that the patient has sufficient privacy and comfort with toileting is also recommended [319,320,321].
Issues of personal privacy often lead to a reluctance of patients to discuss constipation, so clinicians and other healthcare professionals must initiate the discussion and talk honestly about what to expect and measures to prevent and manage the symptom. The assessment tools used most often are the Bristol Stool Form Scale and the Constipation Assessment Scale [319,320]. Assessment should include a review of the list of medications, a history of bowel habits, and abdominal and rectal examination. In addition to checking the list of prescribed medications to determine if constipation is a side effect, the physician should ask the patient about over-the-counter drugs and herbal remedies, as constipation can be a consequence of aluminum-containing antacids, ibuprofen, iron supplements, antidiarrhea drugs, antihistamines, mulberry, and flax. A detailed history of bowel habits helps to establish what is considered normal for the individual patient. The patient should be asked about frequency of stool, the appearance and consistency of stools, use of bowel medications, and previous occurrence of constipation. In general, physical examination of the abdomen for tenderness, distention, and bowel sounds can rule out intestinal obstruction as the cause of constipation. A rectal examination can identify the presence of stool, fecal impaction, or tumor. Imaging of the abdomen (by plain x-ray or computerized tomography) may be appropriate to confirm the presence of obstruction. Consideration of the patient's prognosis and preferences for care should be factored into a decision to carry out diagnostic testing. As with assessment of all symptoms, constipation should be reassessed frequently; assessment at least every three days is recommended [320].
The goal of treatment should be relief of symptoms related to constipation and re-establishment of bowel habits to the patient's comfort and satisfaction; some recommend a goal of one nonforced bowel movement every one to two days, or at least three times per week [310,320,321]. Systematic reviews have demonstrated that data are insufficient to support one laxative or combination of laxatives over others [319,322,323,324].
Many laxatives are FDA approved for occasional constipation, and much of the evidence on their efficacy has come from studies of chronic constipation, not patients with life-limiting disease. In its guidelines for the management of chronic constipation, the American College of Gastroenterology notes the following [323]:
Polyethylene glycol (PEG) and lactulose (both osmotic) improve stool frequency and stool consistency.
Data are insufficient to make a recommendation about the efficacy of stool softeners (docusate [Colace or Surfak]); stimulant laxatives (senna [Senokot, Ex-Lax] or bisacodyl [Dulcolax, Correctol]); milk of magnesia; herbal supplements (aloe); lubricants (mineral oil); or combination laxatives (psyllium plus senna).
The results of a systematic review of studies in the palliative care setting also demonstrated insufficient data for recommendations because of a lack of direct comparisons of laxatives [322]. An update to this review includes evidence that subcutaneous methylnaltrexone is effective in inducing laxation in palliative care in patients with opioid-induced constipation where conventional laxatives have failed [324]. Researchers have concluded that the choice of a laxative should be made on an individual basis, with considerations of patient preferences and the side-effect profile [319,322]. For all patients, oral formulations are recommended over rectal suppositories [319,320]. Rectal suppositories and/or enemas should be used with caution in patients receiving chemotherapy due to the increased risk of the rectal route of administration in the setting of cytopenia [310].
European and Canadian consensus groups and the NCCN have developed practice guidelines for constipation in the palliative care setting on the basis of the available data and expert opinion (Figure 11) [310,319,320]. First-line recommended treatment is a stimulant laxative plus a stool softener (PEG or lactulose) [310,319,322]. A small study of senna with and without docusate for hospitalized patients with cancer showed no significant benefit to the addition of docusate; docusate is specifically not recommended in the Canadian consensus recommendations [320,325]. If constipation persists, other options are bisacodyl, magnesium hydroxide, or sorbitol [310]. Methylnaltrexone (Relistor) was approved by the FDA in 2008 for the treatment of opioid-induced constipation [326]. A systematic review indicated that the subcutaneous drug is effective in the palliative care setting, and is especially useful for patients with constipation refractory to conventional laxatives [324]. In 2014, the FDA approved naloxegol, an oral agent for the management of opioid-associated constipation [327]. However, this drug's approval is limited to patients with chronic non-cancer pain. Practice recommendations note that methylnaltrexone or naloxegol should be considered for patients taking opioids after failure of other laxatives [310,319,320]. Withdrawal of opioids should never be a strategy to manage constipation.
Nonpharmacologic interventions are important adjuncts to laxatives, and the interventions used as prophylaxis are recommended for ongoing management [319,320].
Nausea may occur alone or with vomiting, a neuromuscular reflex. Nausea and vomiting can exacerbate pain and contribute to insomnia, fatigue and weakness, and anorexia. It can also limit activities and cause distress for the patient and family. Nausea is the result of stimulation of one of several pathways: the chemoreceptor trigger zone (located in the medulla), the cortex of the brain, the vestibulocochlear nerve, or the gastrointestinal tract [67].
Nausea alone affects approximately 6% to 68% of adults with life-limiting disease, and vomiting affects 40% [211]. The rate of nausea and vomiting is highest among patients with cancer [211].
The potential causes of nausea and vomiting near the end of life vary according to life-limiting disease [206,214,246,328,329]:
Medications (chemotherapy agents, opioids, antidepressants, antibiotics)
Radiation therapy (especially to the abdomen or lumbosacral spine)
History of peptic ulcer disease or gastroesophageal reflux
Delayed gastric emptying
Primary or metastatic brain tumor
Gastrointestinal tract obstruction
Constipation
Renal failure
Hepatic failure
Pancreatitis
Hypercalcemia
High serum levels of dioxin or anticonvulsants
The causes also differ according to the pathway stimulated (Table 14) [328,329]. Most often the cause is multifactorial, but sometimes no cause can be determined.
CAUSES OF NAUSEA AND VOMITING ACCORDING TO PATHWAY STIMULATED AND CLASS OF ANTIEMETICS
| Pathway Stimulated | Causes | Class of Antiemetics |
|---|---|---|
| Chemoreceptor trigger zone | Metabolic disorders (hypercalcemia, hyponatremia, hepatic/renal failure) | Dopamine antagonists |
| Opioids | Prokinetic agent, dopamine antagonists | |
| Malignant bowel obstruction | Prokinetic agent, dopamine antagonists, corticosteroids | |
| Cortex of brain | Increased intracranial pressure, anxiety, five senses | Corticosteroids, anxiolytics |
| Peripheral pathways (gastrointestinal tract) | Gastroparesis | Prokinetic agent |
| Vestibular system | Motion | Muscarinic acetylcholine receptor, antihistamine |
The prevention of nausea and vomiting has focused on prophylactic treatment for patients receiving chemotherapy or radiation therapy for cancer. Although most patients at the end of life do not receive anticancer treatment, chemotherapy may be given as part of palliative care. ASCO classifies chemotherapy drugs according to their emetogenic potential: high (>90% incidence of emesis without an antiemetic), moderate (30% to 90% incidence), low (10% to 30% incidence), and minimal (<10% incidence) [330]. According to ASCO guidelines, a 5-hydroxytryptamine type 3 (5-HT3) antagonist, dexamethasone (Decadron), and a neurokinin 1 (NK1) receptor antagonist (such as aprepitant [Emend]) should be used as prophylaxis for a highly emetic chemotherapy agent or combination (such as an anthracycline and cyclophosphamide) [330]. Palonosetron (Aloxi), in combination with dexamethasone or netupitant, is recommended for chemotherapy agents with moderate emetic risk, and dexamethasone is recommended before the first dose of chemotherapy with a low emetic risk. A 5-mg dose of olanzapine has been shown to be safe and effective when used in combination with a 5-HT3 receptor antagonist, an NK1 receptor antagonist, and dexamethasone in patients with high emetic risk [330]. For nausea and vomiting not related to chemotherapy, treatment with regular dosing of an antiemetic will help prevent subsequent episodes of the symptoms.
A detailed history, physical examination, and review of the medication list are essential for planning effective management of nausea and vomiting. In talking with the patient, the clinician should ensure that the patient is actually experiencing nausea, as patients have used the term nausea to describe other feelings, such as pain, distention, abdominal discomfort, and early satiety [67,331]. The clinician should ask about the onset of the nausea, how frequently it occurs, if there are precipitating factors, and if there is a relationship to food intake. It may be helpful to ask the patient to rate the intensity of nausea on a scale similar to a pain scale (a 10-point numerical scale). Because the cause of nausea and vomiting is often multifactorial, a multidimensional assessment is beneficial, with particular attention paid to such other symptoms as pain, appetite, fatigue, depression, and anxiety. The physical examination should include evaluation for signs of cachexia or malnutrition, assessment of the abdomen for evidence of bowel obstruction, increased bowel sounds, and abdominal distention. A plain x-ray of the abdomen (e.g., kidney, ureters, bladder) may distinguish constipation with stool seen in the bowel from malignant bowel obstruction [331]. In addition, a neurologic examination should be done to determine if there are signs of increased intracranial pressure, papilledema, or autonomic insufficiency [67,331]. Diagnostic testing may include laboratory studies to rule out metabolic disorders, renal impairment, or liver failure, or radiographs of the abdomen to determine if there is obstruction.
Nausea and vomiting assessment often leads to no clear etiology or several possible causes [331]. Nausea is often not reported; patients should be asked if they have experienced nausea even if they have not vomited [246].
Evidence-based guidelines for the management of nausea and vomiting unrelated to chemotherapy and radiation are lacking [332]. In addition, most studies of these symptoms and recommendations are related to the cancer setting. In general, experts have recommended that antiemetics be selected on the basis of the emetic pathway and the etiology of the nausea and/or vomiting, but systematic reviews have found that the evidence for recommendations is weak to moderate at best [206,328,329,332,333,334]. One systematic review found no evidence that the choice of antiemetic according to etiology or multiple antiemetics was better than a single antiemetic [332].
Several classes of pharmacologic agents can be used to manage nausea and vomiting; the main classes used in the end-of-life setting are prokinetic agents, dopamine receptor antagonists, antihistamines, anticholinergics, 5-HT3 receptors, and corticosteroids (Table 15) [328,329,334]. A first antiemetic should be scheduled and titrated to efficacy, maximum recommended dose, or dose-limiting side effects. If a first drug does not adequately control nausea and vomiting, a second (and perhaps subsequent agents) with different receptor binding can be added in a stepwise manner [331]. Oral antiemetics are recommended unless the patient is vomiting or has symptomatic gastric stasis. Drugs that block several receptors (e.g., olanzapine) may be advantageous if the nausea and vomiting seems refractory [331].
PHARMACOLOGIC MANAGEMENT OF NAUSEA AND VOMITING
| Drug Class | Drug | Typical Starting Dose and Frequency |
|---|---|---|
| Prokinetic agents | Metoclopramide | 10–20 mg PO/IV/SC, every 6 to 8 hours |
| Dopamine antagonists | Haloperidol | 0.5–1.5 mg PO/IV/SC every 6 to 8 hours |
| Prochlorperazine | 5–10 mg PO every 6 hours | |
| Chlorpromazine | 10–25 mg PO/IV every 4 to 6 hours | |
| Olanzapine | 5–10 mg PO daily | |
| Levomepromazine | 6.25–25 mg SC twice daily | |
| Antihistamines | Promethazine | 25 mg PO 4 to 6 hours |
| Anticholinergics | Hyoscine hydrobromide | 0.1–0.4 mcg PO/IV/SC every 4 hours |
| 5-hydroxytryptamine type 3 receptor antagonists | Ondansetron | 4–8 mg PO/IV 1 or 2 times daily |
| Granisetron | 1 mg twice daily | |
| Dolasetron | 200 mg daily | |
| Palonosetron | 0.25 mg IV daily | |
| Mirtazapine | 15–45 mg PO, every night | |
| Corticosteroids | Dexamethasone | 4–8 mg daily |
| PO = orally, IV = intravenously, SC = subcutaneously. | ||
The prokinetic agent metoclopramide (Reglan) has been recommended as a first-line treatment because of its central and peripheral actions and its effectiveness for many chemical and undetermined causes of nausea [206,246,328,331]. The drug should be used with caution in patients with heart failure, diabetes, and kidney or liver disease; the dose should be reduced by 50% for older patients and those with moderate-to-severe renal impairment [329,331]. Chronic use of prokinetic agents and dopamine receptor antagonists may be associated with the development of tardive dyskinesia, especially in frail, elderly patients [187]. Octreotide (Sandostatin), dexamethasone, and hyoscine hydrobromide (Scopolamine) are recommended for bowel obstruction [92,328,329,331,332]. Ondansetron (Zofran) has been suggested for chronic nausea, but in September 2011, the FDA issued a safety announcement about the drug, noting that it may increase the risk of QT prolongation on electrocardiogram. [329,335]. In 2012, the FDA updated the safety information specifically for the 32-mg IV dose of the drug, and the manufacturer subsequently announced changes to the drug label removing this dose [336]. Haloperidol (Haldol) is recommended for uremia-induced nausea in people with end-stage chronic kidney disease [214]. Dexamethasone is used for nausea and vomiting related to increased intracranial pressure and, although the evidence is limited, it is also used as second-line treatment for intractable nausea and vomiting and as an adjuvant antiemetic [246,328,329]. Olanzapine (Zyprexa), an atypical antipsychotic, has also been effective for nausea that has been resistant to other traditional antiemetics, as well as for opioid-induced nausea [337]. A benzodiazepine (such as lorazepam [Ativan]) may be of benefit if anxiety is thought to be contributing to nausea or vomiting [329].
In addition to pharmacologic management of nausea and vomiting, other supportive approaches include maintenance of oral hygiene, regular baths to reduce unpleasant odors, and small meals at regular intervals [206,246]. Cold foods may be better tolerated than hot foods because of decreased smells.
The symptoms of anorexia and cachexia often occur in tandem. While anorexia encompasses decreased appetite and food intake, cachexia is defined as physical wasting with loss of skeletal and visceral muscle mass accompanied by asthenia and autonomic failure. The two conditions are often linked by the term "anorexia-cachexia syndrome," but the exact relationship between the two conditions is unclear [338]. For example, decreased food intake may lead to weight loss, but the body wasting of cachexia is not solely the result of decreased intake [339]. "Wasting" is often used as a synonym for cachexia, but wasting indicates weight loss due to inadequate nutritional intake, whereas cachexia refers to a loss of lean body mass resulting metabolic derangement rather than nutritional deficiency [340]. Complications of cachexia include asthenia (weakness), hypoalbuminemia, emaciation, and immune system impairment [310].
Cachexia is associated with a poor prognosis in many life-limiting diseases. In fact, unintentional, progressive weight loss of more than 10% of body weight over the past six months, with an albumin level less than 2.5 mg/dL is a prognostic indicator for hospice referral [76]. Despite this relationship between cachexia and poor prognosis, the condition is under-recognized and underdiagnosed [341].
Cachexia has also been challenging to define. The lack of an operational definition led to a consensus conference at which a definition was crafted [339]. This definition joins others for disease-specific cachexia (Table 16). The diagnosis and management of anorexia/cachexia has been studied the most in the settings of cancer and HIV infection.
DEFINITIONS AND DIAGNOSTIC CRITERIA FOR CACHEXIA
| Condition | Definition and/or Diagnostic Criteria | ||||||
|---|---|---|---|---|---|---|---|
| All patients with chronic disease |
| ||||||
| Cancer cachexia | A multifactorial syndrome defined by an ongoing loss of skeletal muscle mass (with or without loss of fat mass) that cannot be fully reversed by conventional nutritional support and leads to progressive functional impairment. Its pathophysiology is characterized by a negative protein and energy balance driven by a variable combination of reduced food intake and abnormal metabolism. | ||||||
| Cardiac cachexia | 6% non-edematous, nonvoluntary weight loss over 6 months | ||||||
| HIV-associated wasting |
At least one of the following:
|
Anorexia occurs in 21% to 92% of adults with life-limiting disease, with the highest rates found among patients with cancer [207,211,307]. Cachexia has been reported in 16% to 57%, again with the highest rates found among people with cancer [341].
Across life-limiting diseases, anorexia may develop secondary to several other symptoms, such as fatigue, constipation, xerostomia, dysphagia, mucositis, and nausea. Endocrine disorders as well as psychological, social, and spiritual distress can diminish the desire to eat [187,345]. Changes in taste sensations (leading to food aversions), altered sense of smell, and early satiety have been common among people with cancer and anorexia [345,346].
Studies have shown that multiple factors contribute to cachexia. Abnormal metabolism is thought to lead to a negative protein and energy balance, with subsequent loss of muscle mass [201,339,342,343]. Inflammation, increased neurohormonal activity, insulin resistance, and increased muscle protein breakdown are often associated with cachexia [339,343,347]. The role these factors play in the development of cachexia may differ according to the underlying chronic condition.
Preventive measures for anorexia include effective management of symptoms that are known to have a potential impact on the desire and/or ability to eat. No appropriate measures to prevent cachexia are available.
Guidelines for assessing anorexia and cachexia have been developed for the cancer and HIV settings [310,348]. According to NCCN guidelines, assessment of anorexia and cachexia in patients with cancer include the following [310]:
Determination of the rate and severity of weight loss
Examination of the oral cavity (the mucous membranes, teeth, gingiva, and lips)
Review of the medications list for drugs that interfere with intake
Evaluation of symptoms that have the potential to interfere with eating and drinking
Evaluation for endocrine abnormalities that may be an underlying cause
Assessment of social and economic factors
The guidelines for the assessment of HIV-related wasting recommend the following [348]:
Thorough and complete history and physical examination, with specific questions related to the patient's nutritional status, caloric intake, appetite, and gastrointestinal and physiologic functioning
Measurements of body composition (considering the following factors: age, height, weight, ideal body weight, body cell mass (by bioelectrical impedance analysis), and body mass index
Laboratory tests (plasma HIV RNA, CD4 cell count, free and total serum testosterone, and serum albumin and thyroid function (if clinically warranted)
Psychosocial evaluation
Dietary assessment
Few evidence-based guidelines for the treatment of anorexia and cachexia are available, primarily because of the lack of studies on these under-recognized conditions and the still-emerging understanding of the causes of cachexia. The first step in managing anorexia is to treat symptoms that interfere with appetite and/or the ability to eat. In addition, nonpharmacologic interventions should be directed at improving enjoyment of food, increasing the sense of well-being, and enhancing a sense of normalcy in daily activities. The patient should be encouraged to try favorite foods, to eat small frequent meals, and to drink high-calorie nutritional supplements [310,347,349,350]. Other interventions include an exercise program, consultation with a nutritionist, swallowing evaluation, and psychiatric consultation (if it is determined that the patient has an eating disorder) [310]. For people with end-stage liver disease and an inadequate caloric intake, protein restriction (to prevent hepatic encephalopathy) should be avoided [201].
Two drugs are FDA approved as appetite stimulants for anorexia associated with life-limiting disease (Table 17). Megestrol acetate is FDA approved for the treatment of anorexia, cachexia, or unexplained weight loss in patients with AIDS [351]. It has become the most widely used drug for these indications for people with other life-limiting diseases, and a meta-analysis of data from studies (involving people with a variety of life-limiting illnesses) demonstrated that megestrol acetate was beneficial, especially with respect to improving appetite and weight gain in people with cancer [351]. Meta-analysis showed a benefit of megestrol acetate compared with placebo, particularly with regard to appetite improvement and weight gain in cancer, AIDS, and other underlying conditions. There was insufficient information to define the optimal dose, but higher doses were more related to weight improvement than lower doses. Side effects (e.g., edema, thromboembolic phenomena) and deaths were more frequent in patients treated with megestrol acetate compared with placebo [351]. Today, use of megestrol is limited due to the increased risk for thromboembolism. Dronabinol (Marinol), an oral cannabinoid, is FDA approved for anorexia associated with weight loss in people with AIDS [326]. Because of its effects, dronabinol should be used with caution for people with cardiac disorders, depression, or a history of substance abuse; people taking concomitant sedatives or hypnotics; and older individuals [326].
PHARMACOLOGIC MANAGEMENT OF ANOREXIA AND CACHEXIA
| Drug | Dose Range | Findings | FDA Approval |
|---|---|---|---|
| Megestrol acetate | 200–600 mg/day | Increased appetite, food intake, and weight | For the treatment of anorexia, cachexia, or unexplained weight loss in patients with AIDS |
| Dronabinol | 2.5–20 mg, twice daily (before lunch and dinner) | Stimulated appetite and improved body weight | For anorexia associated with weight loss in people with AIDS |
| Metoclopramide | 10 mg, 3 times daily | Enhanced appetite in people with early satiety | For nausea and vomiting |
| Recombinant human growth hormone | 0.1 mg/kg SC at bedtime (max: 6 mg) | Increased lean body mass and improved physical endurance and quality of life among people with HIV-related cachexia | For HIV-related wasting or cachexia (with concomitant antiretroviral therapy) |
| Oxandrolone (anabolic steroid) | 5–20 mg/day | Increased body weight and lean body mass in cachexia related to HIV and COPD | Adjunctive therapy to promote weight gain after weight loss following extensive surgery, chronic infection, or severe trauma and for some patients without a definitive pathophysiologic cause of weight loss |
| Ghrelin | Not defined | Increased lean body mass in people with end-stage renal disease, COPD, and heart failure | Not approved |
| AIDS = acquired immune deficiency syndrome, COPD = chronic obstructive pulmonary disease, HIV = human immunodeficiency virus, SC = subcutaneous. | |||
In addition to appetite stimulants, metoclopramide, a drug approved for treatment of nausea and vomiting, is recommended for anorexia related to early satiety in people with cancer [310,349].
The treatment of cachexia is more challenging because its pathophysiology is poorly understood and because treatments may differ according to the life-limiting disease. According to the guidelines for cachexia related to cancer and HIV infection, management includes improving nutritional intake, treating disease-related causes of cachexia, treating anorexia, and addressing psychosocial or lifestyle issues [310,348].
Currently, there is no one treatment or combination of treatments that is effective for all patients with cachexia [350]. Increasing oral intake alone is not sufficient, and reversal of wasting may not always be possible; the goal should be to prevent or delay further wasting and functional decline [310,348,350]. As noted, the use of megestrol acetate is effective in increasing weight, but increased nutrition and weight are not sufficient to effectively manage cachexia, and more research is needed to identify agents to increase body mass and to define a multimodal strategy to stop and/or reverse wasting. These strategies may differ according to the underlying chronic disease.
Studies have indicated that recombinant human growth hormone (rhGH) significantly increases lean body mass and improved physical endurance and quality of life in people with HIV [352,353]. In addition, rhGH has shown benefit in cachexia related to pulmonary and cardiac disease [354]. Recombinant somatropin (Serostim) is approved for the treatment of people with HIV with wasting or cachexia; concomitant antiretroviral therapy is necessary [252]. The drug is contraindicated in active neoplasia [252].
The anabolic steroid oxandrolone (Oxandrin) is FDA approved as adjunctive therapy to promote weight gain after weight loss following extensive surgery, chronic infection, or severe trauma and for some patients without a definitive pathophysiologic cause of weight loss [252]. The drug has shown benefit in increasing body weight and lean body mass in cachexia related to HIV and COPD [355,356]. The drug is safe and well tolerated, but more studies are needed to determine its risk-benefit ratio before it can be used more widely [357].
Ghrelin has been evaluated for the treatment of cachexia, and its anti-inflammatory properties may address the proposed role of inflammation in the development of cachexia [358]. The results of small studies have demonstrated that ghrelin increases lean body mass in people with end-stage renal disease, COPD, and heart failure [354]. A 2018 systematic review found insufficient evidence to either support or refute the use of ghrelin for the treatment of cachexia [359]. Again, more research is needed before this agent can become part of clinical practice.
For people with a limited life expectancy (weeks to days), the clinician should provide education and emotional support to the patient, family, and/or caregiver regarding the natural history of anorexia and cachexia, and what to expect with disease progression. This can alleviate distress that sometimes leads to well-meaning but futile attempts to pressure or coerce the patient into increased feedings. It may be helpful to discuss with patient and family the following points in reference to end-of-life feeding [310]:
Absence of hunger and thirst and the wish to suspend the effort required for feeding are part of the disease process itself, to be expected near the end of life.
Nutritional support eventually will not maintain weight nor reverse weight loss.
There are risks associated with artificial nutrition and hydration (e.g., fluid overload, infection, hastened death); intravenous feedings rarely improve outcomes.
Symptoms like dry mouth should be treated with local measures.
Discontinuing previously initiated enteral/parenteral nutrition near the end of life is appropriate, ethically permissible, and may improve some symptoms.
Diarrhea is characterized by the frequent passage of loose, watery stools, usually defined as more than three unformed stools within a 24-hour period [360]. Diarrhea is most often acute, lasting for a few days; diarrhea is chronic when it persists for more than three weeks [360]. Left unchecked, diarrhea can result in dehydration, electrolyte imbalance, and fatigue.
The prevalence of diarrhea among adults with life-limiting disease varies widely, ranging from 3% to 90%, with the highest rates reported among people with HIV infection or AIDS [211].
The most frequent cause of diarrhea in patients receiving palliative care is overuse of laxatives and leakage around a fecal impaction [360]. Other common causes include infectious enteritis if acute onset or fever, and impact of underlying disease in people with HIV/AIDS or metastatic colorectal cancer. Diarrhea is also a side effect of many drugs, including antihypertensives, antacids containing magnesium, some NSAIDs, potassium supplements, quinidine, thiazide diuretics, retroviral agents, prokinetic agents (metoclopramide), and antibiotics [310,360].
A detailed history is the cornerstone of assessing patients for diarrhea. The condition is distressful, yet embarrassing, and direct questions should be asked because the patient may not be forthcoming about the symptom. The clinician should ask the patient about the onset of diarrhea, dietary habits, food intolerances, timing of diarrhea in relation to eating, and medications [360,361]. The patient should also describe bowel movements in terms of frequency, color, and consistency. If possible, a stool specimen should be evaluated.
If infectious diarrhea is suspected, a stool sample for culture and toxin assay should be evaluated to identify the causative organism [361,362]. Screening (stool antigen assay) for Clostridioides difficile enterocolitis should always be considered if diarrhea is indolent, unremitting, or recurrent, even if a history of recent antibiotic use is not obvious, as the screening test is simple and the treatment definitive.
The American Gastroenterological Association developed guidelines for the treatment of chronic disease in the general clinical setting, but no specific guidelines are available for the management of diarrhea in palliative care [362].
Treatment of an underlying condition is the optimal approach to managing diarrhea. The clinician should review the medication list and discontinue or reduce the dose of any medication that may be the cause [360,361].
Nonpharmacologic approaches to managing diarrhea include avoiding gas-forming and bulky foods, hot spices, fats, alcohol, and milk until diarrhea is controlled. The patient should be encouraged to drink plenty of fluids to avoid dehydration; beverages with added electrolytes, such as sports drinks, can help maintain proper electrolyte balance.
Pharmacologic management includes the use of bulk-forming agents, adsorbents, and opioids [361]. Kaolin and pectin (Kaopectate), available over the counter, is a combination of adsorbent and bulk-forming agents. However, it provides modest relief and it may take up to 48 hours to be effective [361]. Loperamide (Imodium) is the drug of choice for diarrhea because its side effect profile is better than that for codeine or diphenoxylate (Lomotil) [361]. The initial dose of loperamide is 4 mg, with an additional 2 mg after each loose stool [361]. The package insert for loperamide notes that the maximum daily dose in a 24-hour period is 16 mg, but doses of up to 54 mg a day have been used as part of palliative care with few adverse events [361]. Octreotide has been effective for profuse secretory diarrhea associated with HIV infection and can be used to treat refractory diarrhea [361]. The use of octreotide for diarrhea in the palliative setting is usually off-label, as the drug is FDA approved for the treatment of diarrhea and flushing associated with metastatic carcinoid tumors [247]. Octreotide is administered as a continuous subcutaneous infusion at a rate of 10–80 mcg/hr until improvement of symptoms [361]. Infectious diarrhea should be treated with an appropriate antibiotic. A systematic review found probiotic agents to be of benefit in the management of acute infectious diarrhea [363]. An update to that review could not confirm whether probiotic agents reduce the duration of diarrhea [364].
As defined, insomnia refers to a variety of sleep disturbances, including difficulty falling asleep and difficulty staying asleep (insufficient amount of sleep or frequent awakenings), that results in impaired function during the day [365]. The most frequent type of insomnia among people at the end of life is difficulty staying asleep, primarily because of pain [366]. A lack of sufficient sleep affects the quality of life by contributing to daytime fatigue and weakness, exacerbating pain, and increasing the potential for depression. Family members also become distressed when the patient is unable to sleep, which, in turn, may increase the burden on caregivers.
Insomnia is common among the general population, and rates reported for adults with life-limiting disease are even higher, ranging from 9% to 83% [201,207,211,367]. The highest rates have been found among patients with end-stage renal disease [211].
The primary difference between insomnia in the general population and in people with life-limiting diseases is that insomnia in the latter group is usually secondary to the life-limiting disease or its symptoms [366]. Overall, uncontrolled pain is the most common contributor to the inability to sleep well [366,367]. Other common physical symptoms such as dyspnea, nocturnal hypoxia, nausea and vomiting, pruritus, and hot flashes are also causes of insomnia. Restless legs syndrome may be a substantial contributor to the disruption of sleep among persons with end-stage renal disease [210,310,368,369].
In addition, many psychological conditions associated with a life-limiting disease can cause insomnia; depression, anxiety, delirium, spiritual distress, and grief can make it difficult to fall or remain asleep [366]. Insomnia is a side effect of many drugs, most notably corticosteroids, antidepressants, decongestants, opioids, and some antiemetics [310,365,370]. Patients also may have difficulty sleeping because of disruptions in the normal sleep-wake cycle that result from inactivity and napping during the day. Lastly, stimulants, such as caffeine, and alcohol may keep patients from falling asleep easily.
Adequate relief of pain and other symptoms is the mainstay of preventing insomnia. The most effective preventive measure is limiting the amount of time in bed during the day and restricting the amount of daytime sleep [366]. Encouraging patients to increase activity during the day, as tolerated; to adhere to a regular schedule with limited naps; and to avoid caffeine and alcohol in the afternoon and evening can help lead to more healthy sleep patterns.
Few patients with life-limiting diseases report insomnia, and few clinicians pursue sleep symptoms in their patients [366]. Clinicians should obtain a sleep history from all patients, following guidelines developed by the American Academy of Sleep (Table 18) [365]. The Epworth Sleepiness Scale has been recommended as an assessment tool [310,371].
QUESTIONS TO OBTAIN A SLEEP HISTORY
|
Clinicians should evaluate patients physically as well as psychologically for signs and symptoms that have been identified as contributors to sleep disturbances.
The American Academy of Sleep has developed an evidence-based guideline for the evaluation and management of chronic insomnia in adults and a practice parameter for the psychological and behavioral treatment of insomnia, but neither offers specific guidelines for managing insomnia at the end of life [365,372]. Nonpharmacologic interventions should be implemented first, with pharmacologic therapy added to the treatment plan if these interventions are not effective [366]. Optimizing sleep habits can be useful, especially if they are begun early in the course of the disease.
The nonpharmacologic approaches used to prevent insomnia are also the primary management strategies. Among the recommended behavioral strategies are the following [365,372]:
Stimulus control therapy: Training the patient to reassociate the bed and bedroom with sleep and to re-establish a consistent sleep-wake cycle
Relaxation training: Progressive muscle relaxation and reducing thoughts that interfere with sleep
Sleep restriction: Limiting the time spent in bed to time spent sleeping
Cognitive behavioral therapy has also been reported to be effective when used in combination with behavioral interventions [365,372]. No nonpharmacologic strategy has been found to be superior to another [372]. These interventions are effective and recommended for older individuals and can also be effective for people with life-limiting disease when strategies are individualized according to the patient [366,372].
Several drugs have been approved by the FDA for the treatment of insomnia; the classes of these drugs are sedative-hypnotics and benzodiazepines (Table 19). In addition, antidepressants and antihistamines are often used for insomnia, but this use is off-label.
PHARMACOLOGIC MANAGEMENT OF INSOMNIA
| Drug | Typical Dosea | Comments |
|---|---|---|
| Sedative-Hypnotics (FDA approved for insomnia) | ||
| Zolpidem | 5–20 mg | Useful for sleep-onset insomnia; lower dose should be used for older or debilitated individuals or those with impaired hepatic function |
| Zaleplon | 5–20 mg | Useful for sleep-onset insomnia; lower dose should be used for older or debilitated individuals, patients with impaired hepatic function, and patients taking cimetidine |
| Eszopiclone | 1–3 mg | Has favorable side-effect profile in older individuals, though a lower dose should be used for debilitated individuals; FDA approved for long-term use |
| Benzodiazepines (FDA approved for insomnia) | ||
| Flurazepam | 15–30 mg | Lower dose should be used for female, older, or debilitated individuals; long-acting effect increases risk of daytime drowsiness |
| Estazolam | 0.5–2 mg | Lower dose should be used for older or debilitated individuals |
| Temazepam | 7.5–30 mg | Lower dose should be used for older or debilitated individuals |
| Triazolam | 0.125–0.25 mg | Lower dose should be used for older or debilitated individuals |
| Quazepam | 7.5–15 mg | — |
| Melatonin Receptor Agonists (FDA approved for insomnia) | ||
| Ramelteon | 8 mg | Useful for sleep-onset insomnia; FDA approved for long-term use |
| Orexin Receptor Agonists (FDA approved for insomnia) | ||
| Suvorexant | 10–20 mg | Adjust dose with concomitant use of CYP3A inhibitors |
| Antidepressants (Not FDA approved for insomnia) | ||
| Trazodone | 50–150 mg | — |
| Amitriptyline | 10–100 mg | — |
| Antidepressants (FDA approved for insomnia) | ||
| Doxepin | 3–6 mg | Useful for difficulty with sleep maintenance |
| Nonprescription (FDA approved for occasional insomnia) | ||
| Diphenhydramine | 25–50 mg | For occasional use only |
| aDoses are given as guidelines; actual doses should be determined on an individual basis. | ||
Among sedative-hypnotics, zolpidem (Ambien) is a short- to intermediate-acting drug used primarily for sleep-onset insomnia [365,373]. Zolpidem is recommended by the NCCN for insomnia as part of palliative care for people with cancer [310]. Another sedative-hypnotic, eszopiclone (Lunesta), is intermediate-acting and is one of only three insomnia medications approved by the FDA for long-term use [373].
There is a limited number of studies regarding the use of benzodiazepines in palliative care [374]. However drugs in this class are the most commonly used drugs for the treatment of short-term insomnia in people with life-limiting disease [366]. Benzodiazepines are effective in decreasing the time needed to fall asleep as well as the likelihood of waking up during the night [366,373]. Their use should be short term, as their long-term efficacy has not been clearly defined, although this issue is not as important for patients with a limited life expectancy [366]. Lorazepam (Ativan) is a recommended drug for insomnia in people with cancer [310]. The long-acting effect of flurazepam (Dalmane) may be of benefit for some patients [366].
The antidepressant trazodone (Desyrel) is the preferred antidepressant for insomnia (although it is not FDA approved for this indication) [252,366]. It is the drug of choice among tricyclic antidepressants because of its shorter half-life and its milder anticholinergic side effects [366]. Antidepressants are especially useful for people who have anxiety or depression.
The most recently (2019) FDA-approved drug for insomnia is lemborexant (DayVigo), an orexin receptor antagonist [252]. The first approved drug of this class, suvorexant (Belsomra), received FDA approval in 2014 [252]. These agents support sleep through inhibition of orexin A and B, which are neuropeptides that promote wakefulness [252,375]. Another drug is ramelteon (Rozerem), a melatonin receptor agonist. This drug is short acting and used primarily for sleep-onset insomnia [252,373]. Ramelteon is FDA approved for long-term use [365].
For insomnia related to restless legs, a systematic review showed that dopamine agonists are effective, with cabergoline (Dostinex) and pramipexole (Mirapex) often having a greater efficacy than levodopa (L-Dopa) [376].
Barbiturates are not recommended for insomnia because of the rapid development of tolerance [366]. Two supplements promoted for sleep enhancement—melatonin and valerian—have not been shown to be effective for managing insomnia [366,377].
Several factors must be considered when treating older patients with insomnia. For example, it has been recommended that benzodiazepines be avoided in older individuals because of side effects such as increased risk for falls, confusion, and "hangover" [373]. However, these side effects must be considered in light of an individual's particular situation and weighed against the benefits [366,373]. Eszopiclone and ramelteon have been studied in older individuals and have a favorable side-effect profile for that population [373]. Lower doses are often recommended for older individuals [365].
Delirium is a disturbance of attention and awareness with reduced ability to direct, focus, sustain, or shift attention, as well as changes in cognition (e.g., disorientation, memory deficit, language impairment) [378]. Patients may seem confused or be restless, agitated, or combative. Delirium is often difficult to recognize because it shares diagnostic features with other symptoms, especially dementia and depression. As a result, delirium is often unrecognized or misdiagnosed and consequently inappropriately treated or not treated [379]. Delirium is classified into three clinical subtypes: hypoactive, hyperactive, and mixed [380]. Hypoactive delirium is characterized by lethargy, reduced awareness of surroundings, sedation, and psychomotor retardation, whereas hyperactive delirium is characterized by agitation, restlessness, hallucinations, hypervigilance, and delusions [380]. In the palliative care setting, about half of patients with delirium will have the hypoactive subtype [380,381].
Delirium can be extremely distressful for the patient and even more so for family members. The healthcare team can help alleviate family members' distress by educating them about the nature and cause of the syndrome and the potential for reversal. Encouraging them to participate in nonpharmacologic interventions may also help to provide a positive experience.
The prevalence of delirium among adults in hospice or receiving palliative care ranges from 28% to 80%, occurring most frequently among patients with cancer [382,383]. Terminal delirium is a distinct entity that occurs within the last days or hours of life, and it is estimated to occur in 80% of dying patients [384].
Many factors may cause delirium, and although the cause is usually multifactorial, often no cause is found [385]. In one comprehensive review, the primary contributor to delirium was unrelieved pain [386]. Delirium is also often caused by medications, including several that are used in the end-of-life setting, such as opioids, corticosteroids, benzodiazepines, and NSAIDs, or the sudden withdrawal from alcohol or drugs (particularly benzodiazepines) upon admittance to a hospital or hospice [310,383,384]. In addition, age, cognitive deficits, impaired vision/hearing, emotional stress, depression, and comorbidities are predisposing factors of delirium [381,384].
Because of the substantial influence of unrelieved pain, adequate pain management can help prevent delirium. Prevention strategies are directed at minimizing precipitating factors, which include a high number of medications (more than six), dehydration, decreased sensory input, psychotropic medications, and a change in environment.
The diagnosis of delirium relies on identifying its two features: cognitive impairment and deficits in attention; these features can be assessed with the Mini-Mental State Examination [384]. The Confusion Assessment Method (CAM) is considered to be the gold standard for distinguishing between delirium from other causes of altered mental status, and other tools to evaluate delirium include the Delirium Rating Scale, the Delirium Symptom Interview, and the Memorial Delirium Assessment Scale [384]. Communication with the healthcare team and family is vital in assessing the patient to help determine the onset and course of delirium as well as signs indicative of the syndrome. Some specific ways to help determine if a patient has delirium include [380]:
Ask the patient "Do you feel 100% awake?" If they do not, ask "How awake do you feel?"
Evaluate whether the patient is easily distracted.
Test registration and immediate recall.
Assess psychomotor disturbances by noting whether the patient is restless and agitated or slow and hypoactive.
Ask the patient if he or she is seeing or hearing strange things.
Ask the patient to state the days of the week or months backward, or to give a span of numbers frontward and backward.
Ask the patient open-ended questions, and listen for incoherent speech or tangential thought processes.
Clinical assessment and physical examination should also be directed at ruling out underlying causes, such as infection or metabolic abnormalities, and the medication list should be reviewed carefully [310,384].
The treatment of an underlying cause, if identified, is a key step in managing delirium. Whether delirium can be reversed depends on the cause. Delirium caused by psychotropic medications, dehydration, or hypercalcemia is more likely to be reversible than delirium caused by hypoxia, metabolic abnormalities, or nonrespiratory infections [380,387].
Several nonpharmacologic interventions have been successful in preventing and managing delirium (Table 20) [310,380,382,384]. If delirium is refractory to nonpharmacologic measures, medications may be prescribed. Level 1 evidence supports the use of haloperidol and chlorpromazine (Thorazine) (typical antipsychotics), and these drugs have the advantage of being available in formulations that allow for multiple routes of administration and of being the most cost-effective [310,380]. Several systematic reviews have been done to determine the efficacy of antipsychotics for delirium, and although each review has identified only a few well-designed trials, the results have supported the continued use of these drugs (Table 21) [380,384,388,389,390]. One of these reviews focused on patients with terminal illness; the review identified only one small study (30 subjects) eligible for analysis; haloperidol and chlorpromazine were equally effective, but the risk for cognitive impairment was slightly greater with chlorpromazine [388]. A 2020 update to this review included four studies with 399 participants, most with advanced cancer or advanced AIDS and mild- to moderate-severity delirium [391]. The reviewers found no high-quality evidence to either support or refute the use of drug therapy for delirium symptoms in terminally ill adults. Low-quality evidence indicates that risperidone or haloperidol may slightly worsen delirium symptoms compared with placebo, and moderate- to low-quality evidence indicates that these two agents may slightly increase extrapyramidal adverse events for patients with mild- to moderate-severity delirium [391]. In the other reviews, the efficacy of haloperidol was found to be similar to that of olanzapine, risperidone (Risperdal), and quetiapine (Seroquel) (atypical antipsychotics) [389,390]. In two small nonrandomized studies—one involving hospitalized patients with cancer—aripiprazole (Abilify) was safe and effective for the treatment of delirium, especially the hypoactive subtype [392,393]. Mild-to-moderate delirium can be managed with low oral doses of antipsychotics, titrating the dose to optimum relief; higher doses can be used for severe delirium [310,384]. For older patients and those with multiple comorbidities, treatment should begin with lower doses and titration should be slow [380]. Factors to consider when selecting a drug include the side-effect profile, the patient's age and baseline mental status, the time to response, and the subtype of delirium [380]. There is no recommendation regarding the use of other drug classes for delirium in palliative care (e.g., α-2 receptors agonists, cholinesterase inhibitors, melatonergic drugs, psychostimulants) [382].
NONPHARMACOLOGIC TREATMENT OPTIONS FOR DELIRIUM
|
PHARMACOLOGIC OPTIONS FOR DELIRIUM IN PALLIATIVE CARE
| Drug | Dose Range | Routes of Administration | Comments |
|---|---|---|---|
| Haloperidol | 0.5–2 mg every 2 to 12 hours | PO, IV, IM, SC | Considered to be first-line treatment. |
| Chlorpromazine | 12.5–50 mg every 4 to 6 hours | PO, IV, IM, SC, PR | Has more sedative effect than haloperidol, thus is preferred for patients with agitation. |
| Olanzapine | 2.5–5 mg every 12 to 24 hours | PO | Sedation has been a dose-limiting effect; poorer response has been associated with older age, pre-existing dementia, and hypoactive subtype. |
| Risperidone | 0.25–1 mg every 12 to 24 hours | PO | Response may be better with hypoactive subtype; orthostatic hypotension is possible adverse effect. |
| Quetiapine | 12.5–100 mg every 12 to 24 hours | PO | Sedation and orthostatic hypotension are possible adverse effects. |
| Aripiprazole | 5–30 mg every 24 hours | PO | Response may be better with hypoactive subtype. |
| Lorazepam | 0.5–2 mg every 2 to 4 hours | IV, SC | May be added to treatment with haloperidol if agitation is refractory to high doses. |
| PO = orally, IV = intravenously, IM = intramuscularly, SC = subcutaneously, PR = rectally. | |||
The goal of treatment is to reach patients' baseline mental state, not to sedate them, and patients should be reassessed frequently until this goal is met [384]. If agitation is refractory to high doses of haloperidol, the antipsychotic lorazepam may be helpful [310,384]. Encouraging supportive caregiver presence at the bedside is recommended as a useful adjunct for managing delirium [310]. The management of delirium may also include providing support to family, to help them cope with the condition [310,384]. The management of terminal delirium will be discussed later in this course.
The natural initial reaction to illness that threatens life expectancy is emotional, and patients and their families experience a wide range of emotions, including disbelief, anger, fear, and sadness. Over time, these emotions broaden; patients may feel isolated and lonely, anxious about the burden on their family, or hopeless. Patients expect, or hope, that the healthcare professional in attendance will pay attention, listen carefully, and provide comfort. Beyond personal issues raised for the patient, family members may have guilt about their own well-being, anxiety about the future, and grief about the loss of their loved one. Practical issues such as the cost of care and loss of income from the patient and/or caregiver can add substantially to the feelings of stress.
The prevalence of psychological suffering is high during the last year of life, and addressing this aspect of care is integral to the patient's overall comfort and quality of life. Anxiety and depression are the most common psychological symptoms at the end of life, yet they are among the most underdiagnosed and untreated symptoms [67,394]. Psychological suffering exacerbates pain and other symptoms, limits the patient's capacity for pleasurable activities, and causes distress for both the patient and the family [206,395].
The term "distress" has become standard to describe the psychological suffering experienced by patients with life-limiting disease. The NCCN notes that the word "distress" is more acceptable and is associated with less stigma than words such as "psychosocial" or "emotional" [396]. In its guidelines on distress management, the NCCN defines distress as existing "along a continuum, ranging from common normal feelings of vulnerability, sadness, and fears to problems that can become disabling, such as depression, anxiety, panic, social isolation, and existential and spiritual crisis" [396]. According to a study of patients in a palliative care program, the answers to the question "What bothers you most?" included [216]:
Emotional, spiritual, existential, or nonspecific distress (16%)
Relationships (15%)
Concerns about the dying process and death (15%)
Loss of function and normalcy (12%)
Patients at increased risk of distress include individuals with a history of psychiatric disorder, substance abuse, or depression/suicide attempt; with cognitive impairment or communication barriers; with severe comorbid conditions; and with spiritual/religious concerns. Other factors that predispose a patient to distress include rapidly progressing disease, unrelieved pain, and uncontrolled symptoms [206]. Those who live alone, younger individuals, and dependent children are also at increased risk [396]. Gender and sexual minority patients with life-limiting diseases often have distinct sources of suffering [67]. These patients may be disenfranchised from their families or have been subjected to social stigma, leading to fears of abandonment and isolation. In some instances, spiritual crises may be the result of guilt and shame from past behaviors. Many patients with HIV/AIDS have suffered through the loss of loved ones to the same disease, some of whom may have been part of the individual's defined family and network of social support.
As with physical symptoms, assessment of distress and the psychosocial and spiritual well-being of the patient must be ongoing, as changes occur over time [6,67]. In addition, worsening symptoms and disease progression can affect patients' coping mechanisms [227]. One study found significant correlations between the will to live and existential, psychological, and social sources of distress. In that study, hopelessness, burden to others, and dignity were the variables with the most influence [397]. Other studies have consistently shown that psychosocial suffering has a stronger association than pain with a desire to hasten death [398,399,400,401,402,403].
How a patient responds to his or her disease and care is strongly influenced by attitudes and values learned through family interactions, and social workers should evaluate the patient and family to assess psychosocial as well as practical problems and recommend and/or carry out interventions [6,396]. For many patients, the primary concern about their illness is its impact on the family. The need for palliative care raises issues regarding power, structure, and roles among the patient and his or her family [67]. The impact of a life-limiting disease and the ensuing care threatens the structure and integrity of the family, as family roles are reassigned, the rules of daily living are altered, and methods of problem-solving are revised. Families vary in their ability to adapt to such restructuring, and dysfunction can result from either limited or excessive adaptation. At one end of this spectrum, family members have difficulty breaking away from coping mechanisms, even though they are ineffective. At the other end of the spectrum, family members continually try new coping strategies to meet each crisis, resulting in chaos [67]. Both types of dysfunction can lead to increased demands on the healthcare team and can interfere with the delivery of appropriate care.
Anxiety is a feeling of fear, apprehension, and dread. The patient feels uneasy, insecure, and uncertain about the future. Often, the patient is not able to identify the source of anxiety, but it can be related to any number of physical, psychological, social, spiritual, or practical issues common during the end of life.
Severe anxiety varies widely among adults with life-limiting disease, ranging from 8% to 79%, with the highest rate among patients with cancer [211].
One of the primary causes of anxiety is inadequate pain relief. Anxiety may also be the result of a patient's overwhelming concern about his or her illness, the burden of the illness on the family, and the prospect of death. In addition, anxiety is a potential side effect of many medications, including corticosteroids, metoclopramide, theophylline, albuterol, antihypertensives, neuroleptics, psychostimulants, antiparkinsonian medications, and anticholinergics. Lastly, withdrawal from opiates, alcohol, caffeine, cannabis, and sedatives can result in anxiety, particularly in the first few days of admission [404].
Effective pain management is the best way to prevent anxiety. Also, educating the patient and the family about what to expect over the course of the illness and providing adequate psychological and spiritual support can help comfort the patient, thereby preventing anxiety.
Family members and friends may be able to provide information about the level of anxiety experienced by the patient currently and in past situations. All members of the healthcare team should evaluate the patient and the clinical record for reversible causes of anxiety, such as those caused by medications or withdrawal syndromes, and should try to distinguish anxiety from delirium, depression, or bipolar disorder [405,406].
Anxiety manifests itself through physical as well as psychological and cognitive signs and symptoms. These signs and symptoms include dyspnea, paresthesia, tachycardia, chest pain, urinary frequency, pallor, restlessness, agitation, hyperventilation, insomnia, tremors, excessive worrying, and difficulty concentrating.
Nonpharmacologic approaches are essential for managing anxiety, and the addition of pharmacologic treatment depends on the severity of the anxiety [67,407]. Effective management of pain and other distressing symptoms, such as constipation, dyspnea, and nausea, will also help to relieve anxiety. If the anxiety is thought to be caused by medications, they should be replaced by alternate drugs. Other strategies include psychological support that allows the patient to explore fears and concerns and to discuss practical issues with appropriate healthcare team members. Relaxation and guided imagery may also be of benefit [408]. A consult for psychological therapy may be needed for patients with severe anxiety.
When pharmacologic management is deemed necessary, benzodiazepines are generally preferred, and administration on an as-needed basis is usually sufficient [67]. Neuroleptics and tricyclic antidepressants may also be effective (Table 22). For all medications, the initial dose should be low and subsequently titrated to produce the desired effect within the level of tolerance. Benzodiazepines should be given with caution in older patients, as these drugs may harm memory or cause confusion and agitation in patients who have cognitive impairment [409].
PHARMACOLOGIC MANAGEMENT OF ANXIETY AND DEPRESSION
| Condition | Drug Class, Drugs | Typical Starting Oral Dosea | Titration Recommended | Maximum Daily Dose | Comments |
|---|---|---|---|---|---|
| Anxiety | Benzodiazepines | ||||
| Lorazepam | 0.5–2 mg, every 1 to 6 hours | May titrate upward | — | First choice | |
| Diazepam | 2.5–10 mg, every 3 to 6 hours | May titrate upward | — | ||
| Midazolam | 2–10 mg/day (SC) | May titrate upward | — | ||
| Clonazepam | 0.5–1.0 mg, 3 times per day | May titrate upward 4 mg | — | ||
| Neuroleptics | |||||
| Haloperidol | 0.5–4.0 mg, every 4 to 6 hours | May titrate upward | — | — | |
| Thioridazine | 10 mg, 3 times per day | May titrate upward | — | — | |
| Tricyclic Antidepressant | |||||
| Imipramine | 10–25 mg, 3 times per day | May titrate upward | — | — | |
| Depression | Selective Serotonin Reuptake Inhibitors | ||||
| Fluoxetine | 20 mg/day | Increase by 10 mg every 1 to 2 weeks | 20–60 mg | First choice when immediate onset not needed (onset at 4 to 6 weeks) | |
| Paroxetine | 10 mg/day | Increase by 10 mg every 1 week | 10–50 mg | ||
| Sertraline | 50 mg/day | Increase by 25 mg every 1 week | 50–150 mg | ||
| Escitalopram | 10 mg/day | — | 20 mg | ||
| Venlafaxine | 18.75 mg/day | Increase by 75 mg every 1 week | 75–225 mg | ||
| Tricyclic Antidepressants | |||||
| Amitriptyline | 25 mg/day | Increase by 25 mg every 1 to 2 days | 50–150 mg | Less useful because of side effects; slow onset of action (3 to 6 weeks) | |
| Nortriptyline | 25 mg/day | 50–150 mg | |||
| Desipramine | 25 mg/day | 50–150 mg | |||
| Doxepin | 25 mg/day | 50–200 mg | |||
| aDoses are given as guidelines; actual doses should be determined on an individual basis. | |||||
Depression is linked to many other symptoms, especially pain, and is a primary source of suffering. Depression in patients with life-limiting disease is a challenge to identify, as feelings of sadness, helplessness, and hopelessness are a typical reaction to the situation [206,408]. Depression is more likely when sadness and/or hopelessness is overwhelming or pervasive and is accompanied by a sense of despair [408,411]. Early diagnosis is essential for effective treatment and relief of other symptoms.
The prevalence of depression varies widely among adults with life-limiting diseases, ranging from 3% to 82%, with the highest rate among patients with HIV/AIDS and end-stage liver disease [201,211].
Unrelieved pain is one of the primary risk factors for depression. Other causes within the physical domain include metabolic disorders (hyponatremia or hypercalcemia), lesions in the brain, insomnia, or side effects of medications (corticosteroids or opioids). Many patients with heart failure have comorbidities and polypharmacy, both of which can increase the risk of depression [412,413]. Psychosocial causes include despair about progressive physical impairment and loss of independence, financial stress, family concerns, lack of social support, and spiritual distress.
Adequate management of pain, attention to psychosocial and spiritual well-being, and early referral for mental health or pastoral counseling are the best strategies to prevent depression.
The diagnosis of depression is complicated, as the usual somatic signs of depression—anorexia, sleep disturbances, weight loss, and fatigue—are often symptoms related to the underlying disease or part of the constellation of symptoms experienced by patients with life-limiting disease [227]. Because of this, assessment should focus on psychological and cognitive symptoms, such as:
Persistent dysphoria
Loss of pleasure in activities
Frequent crying
Loss of self-esteem
Sense of worthlessness
Excessive guilt
Pervasive despair
Thoughts of suicide
A diagnosis of depression requires the presence of at least five depression-related symptoms within the same two-week period, and the symptoms must represent a change from a previous level of functioning [378]. A simple screening tool that has been found to be effective is to ask the patient, "Are you depressed?" or, "Do you feel depressed most of the time?" [227,414,415]. The physician should also discuss the patient's mood and behavior with other members of the healthcare team and family to help determine a diagnosis. Patients who have thoughts of suicide must be assessed carefully. The physician should differentiate between depression and a desire to hasten death because of uncontrolled symptoms [67]. Psychological counseling should be sought, as well as measures to enhance the management of symptoms.
The effective management of depression requires a multimodal approach, incorporating supportive psychotherapy, cognitive strategies, behavioral techniques, and antidepressant medications [47]. Patients with depression should be referred to mental health services for evaluation, and resultant approaches may include formal therapy sessions with psychiatrists or psychologists or counseling from social workers or pastoral advisors. In addition, physicians can help by having discussions with the patient to enhance his or her understanding of the disease, treatments, and outcomes, and to explore expectations, fears, and goals. Behavioral interventions, such as relaxation techniques, distraction therapy, and pleasant imagery have been effective for patients with mild-to-moderate depression [47].
Strong evidence supports the use of tricyclic antidepressants or SSRIs, along with psychosocial interventions, for the management of depression in patients with cancer [47,212]. Evidence to support the use of specific pharmacologic agents to treat depression in patients with noncancer diagnoses is not as strong, but psychostimulants may also be helpful [47,67,227,416]. The choice of medication depends on the time available for treatment. The most immediate effect (within days) is achieved with a rapid-acting psychostimulant (e.g., dextroamphetamine, methylphenidate); longer times to therapeutic effect are associated with SSRIs (two to four weeks) and tricyclic antidepressants (three to six weeks).
Medical ethicists define spirituality as the ways people live in relation to transcendent questions of meaning, value, and relationship, whereas religion involves a community of beliefs and practices sharing a common orientation toward these spiritual questions [530]. Spirituality is unique to each person. It is founded in cultural, religious, and family traditions and is modified by life experiences. Spirituality is considered not to be dependent upon formal religious faith, and many surveys have shown that spirituality or religion is an integral component of people's lives [67,417]. Spirituality also plays a significant role in health and illness. Studies have shown spirituality to be the greatest factor in protecting against end-of-life distress and to have a positive effect on a patient's sense of meaning [411,418]. Thus, a spiritual assessment and spiritual care to address individual needs are essential components of the multidimensional evaluation of the patient and family [206,419].
A life-limiting disease will lead patients to ask questions that may give way to spiritual conflicts, such as "Why would God let me suffer this way?" Patients may also carry out life review in search of meaning for their illness; some may view their illness as punishment for past "sins." Left unanswered, spiritual questions and concerns lead to spiritual distress and suffering, which can cause or exacerbate pain and other physical and psychosocial symptoms. It then becomes critical for the healthcare team to facilitate pastoral services to address patients' spiritual concerns [6]. In general, the spiritual and existential concerns of patients at the end of life relate to four areas: the past, the present, the future, and religion (Table 23) [206].
SPIRITUAL AND EXISTENTIAL CONCERNS OF PATIENTS AT THE END OF LIFE
| Relation of Concern | Concerns | |||||
|---|---|---|---|---|---|---|
| Past |
| |||||
| Present |
| |||||
| Future |
| |||||
| Religion |
|
The need for spirituality at the end of life is heightened, and patients will search for meaning as a way to cope with emotional and existential suffering [420]. Spirituality helps patients cope with dying through hope. At the time of diagnosis, patients hope for cure, but over time, the object of hope changes and the patient may hope for enough time to achieve important goals, personal growth, reconciliation with loved ones, and a peaceful death [2,67].
In a landmark nursing care study conducted through a structured interview, researchers explored the meaning of hope and identified strategies used to foster hope among 30 adults facing terminal illness [421]. Hope was defined as an inner power directed toward enrichment of "being." Seven defining characteristics or strategies for fostering/maintaining hope were identified [421]:
Interpersonal connectedness: The presence of a meaningful shared relationship(s) with another person(s)
Lightheartedness: Verbal and nonverbal communication characterized by delight, joy, or playfulness
Personal attributes: Determination, courage, serenity
Attainable aims: Directing efforts at some purposeful and attainable goal, such as writing notes/letters to distant family members or friends (from the past)
Spiritual base: The presence of active spiritual beliefs and practices
Uplifting memories: Recalling positive moments and uplifting times in the past
Affirmation of worth: Having one's individuality accepted, honored, and acknowledged
Spirituality can also help a patient gain a sense of control, acceptance, and strength. As a result, greater spiritual well-being has been associated with decreased rates of anxiety and depression among people with advanced disease [207,422]. There has been a growing emphasis on the need for physicians to discuss spirituality with their patients [419,423]. A spiritual history should be obtained to elicit answers to such questions as:
Do you consider yourself spiritual or religious?
Do you have spiritual beliefs that help you cope with stress?
What importance does your faith or belief have in your life?
Are you part of a spiritual or religious community?
One recommended mnemonic for the components of a spiritual history is SPIRIT: spiritual belief system; personal spirituality; integration with a spiritual community; ritualized practices and restrictions; implications for medical care; and terminal events planning [424].
Spiritual care is an essential component of palliative care, and most palliative care teams include a chaplain or access to one for consultative purposes. However, what patients and families perceive to be spiritual care and how it should be delivered have not been well-defined [417]. Patients and families have found spiritual comfort with friends and family, clergy and other pastoral care providers, and healthcare professionals [417]. Among healthcare professionals, barriers to providing spiritual care are time; social, religious, or cultural discordance; and lack of privacy and care continuity [417]. While it is not the role of the clinician to provide spiritual care, there is an ethical obligation to give attention to expressed needs and to bear in mind that spirituality and religion are essential to many patients' identity as persons. The healthcare professional's role should be to inquire, assess, and refer as indicated [530]. Doing so demonstrates respect for the patient as a whole person and strengthens the patient-clinician relationship.
Adequate psychosocial support is also needed for the patient's family. The structure of families varies widely, and it is important to note that what constitutes a family is defined by the patient. It is essential for the healthcare team to talk to patients during the initial assessment about who provides support, with whom they wish to share information, and who should be involved in planning care and decision making [6,67]. For some patients, friends provide the support network when families are not nearby, or the patient is disenfranchised from his or her family. Social workers have a prominent role in helping these patients overcome such barriers as discrimination and legal and financial issues, as well as ensuring appropriate support for grieving partners who may be disenfranchised [425].
Family caregivers can become overwhelmed with added responsibilities. Often, the caregiver is a spouse who is older and may also have illnesses. In addition, children and teenagers are frequently forgotten, but addressing their concerns and needs is essential for their psychological well-being and appropriate grieving [67]. Young children will realize that the family structure has been disrupted. They should be encouraged to ask questions, and they usually need time to interpret answers. Adolescence is a challenging time in itself, and dealing with the illness and loss of a parent or close family member may result in aggressive behavior, isolation, or sexuality. Frequent evaluation of family members' coping strategies, moods, and behaviors can help to determine if early referral for individual counseling or family therapy is necessary. Support should be provided to ensure that the patient and family has access to resources to help with finances, that the home environment is safe, that caregivers are available, and that adequate transportation is available [310].
Family roles are also important to understand, and these roles are strongly influenced by culture. Many cultures highly value family, with strong family ties across many generations. Patients from such cultures will often have many visitors at one time. The palliative care team should accommodate such visits when possible. In addition, family hierarchy may dictate behavior of family caregivers. For example, in traditional Vietnamese families, a female member of the family is expected to stay at the bedside of the patient for comfort and support [426]. In Asian families, elders are revered and a young person cannot tell an older person what to do [427]. This may make it difficult for a healthcare professional who is younger than the patient. Patients and families who adhere to Native American cultures have unique traditions and rituals that should be respected [428].
All members of the healthcare team should become familiar with the cultural context of their patients and provide resources from within the cultural community if possible. A bilingual healthcare worker can provide an important link to a community [429].
In the last days, the goals of the healthcare team are to ensure a peaceful death for the patient and to support the family during the dying process and throughout grief and mourning. The focus for the patient is management of symptoms and emotional and spiritual ease, and the focus for the family is education to prepare them for the dying process.
During the last days, all care should be directed at comfort, and the NCCN has listed several interventions for imminently dying patients (Table 24) [310]. The physician should minimize the number of medications by reassessing the need for each one. The symptoms that occur most commonly during the last days are pain, noisy breathing, dyspnea, and delirium, and medications to manage these symptoms should be maintained or initiated [67]. In addition, medication may be required to reduce the risk of seizures. Medications should be prescribed for the least invasive route of administration (oral or buccal mucosa), but patients may lose the ability to swallow, making a subcutaneous, transdermal, or intravenous route necessary.
INTERVENTIONS FOR PATIENTS WHO ARE IMMINENTLY DYING
|
Treatment of pain should continue, and knowledge of opioid pharmacology becomes critical during the last hours of life [67,430]. The metabolites of morphine and some other opioids remain active until they are cleared through the kidneys. If urine output stops, alternative opioids, such as fentanyl or methadone, should be considered, as they have inactive metabolites [214,431].
Anticholinergic medications can eliminate the so-called "death rattle" brought on by the build-up of secretions when the gag reflex is lost or swallowing is difficult. However, it is important to note that results of clinical trials examining various pharmacologic agents for the treatment of death rattle have so far been inconclusive [432]. Despite the lack of clear evidence, pharmacologic therapies continue to be used frequently in clinical practice [430]. Specific drugs used include scopolamine, glycopyrrolate, hyoscyamine, and atropine (Table 25) [67,430,433]. Glycopyrrolate may be preferred because it is less likely to penetrate the central nervous system and with fewer adverse effects than with other antimuscarinic agents, which can worsen delirium [430]. For patients with advanced kidney disease, the dose of glycopyrrolate should be reduced 50% (because evidence indicates that the drug accumulates in renal impairment) and hyoscine butylbromide should not be used (because of a risk of excessive drowsiness or paradoxical agitation) [214]. Some evidence suggests that treatment is more effective when given earlier; however, if the patient is alert, the dryness of the mouth and throat caused by these medications can be distressful. Repositioning the patient to one side or the other or in the semiprone position may reduce the sound. Oropharyngeal suctioning is not only often ineffective but also may disturb the patient or cause further distress for the family. Therefore, it is not recommended.
TREATMENT OF EXCESSIVE RESPIRATORY SECRETIONS CAUSING "DEATH RATTLE"
| Drug | Dose | ||
|---|---|---|---|
| Scopolamine (transdermal patch) |
| ||
| Glycopyrrolate | 0.2–0.4 mg SC, repeat at 30 minutes, then every 4 to 6 hours, as needed; or 0.6–1.2 mg/day CSCI | ||
| Hyoscyamine | 0.4 mg SC, repeat at 30 minutes, then every 2 to 4 hours, as needed; or 0.6–1.2 mg/day CSCI | ||
| Atropine | 0.4–0.8 mg SC, repeat every 2 to 4 hours | ||
| CSCI = continuous subcutaneous infusion, SC = subcutaneously. | |||
Terminal delirium occurs before death in 50% to 90% of patients. It is associated with shorter survival and complicates symptom assessment, communication, and decision making. It can be extremely distressing to caregivers and healthcare professionals alike [430]. Safety measures include protecting patients from accidents or self-injury. Reorientation strategies are of little use during the final hours of life. Education and support for families witnessing a loved one's delirium are warranted [430]. There are few randomized controlled trials on the management of terminal delirium. Agents that can be used to manage delirium include haloperidol, which is frequently the first choice for its relatively quick action [206,430]. Other drugs may include olanzapine, chlorpromazine, levomepromazine, and benzodiazepines [206,430]. For terminal delirium associated with agitation, benzodiazepines, including clonazepam, midazolam, diazepam, and lorazepam may be helpful [206,227,430]. Depending on which drug is used, administration may be intravenous, subcutaneous, or rectal, and the dose can be titrated until effective.
Seizures at the end of life may be managed with high doses of benzodiazepines. Other antiepileptics such as phenytoin (administered intravenously), fosphenytoin (administered subcutaneously), or phenobarbital (60–120 mg rectally, intravenously, or intramuscularly every 10 to 20 minutes as needed) may become necessary until control is established.
A calm and peaceful environment should be maintained for the patient. Family and spiritual leaders should be allowed to carry out traditional rites and rituals associated with death.
Palliative sedation may be considered when an imminently dying patient is experiencing suffering (physical, psychological, and/or spiritual) that is refractory to the best palliative care efforts. Terminal restlessness and dyspnea have been the most common indications for palliative sedation, and thiopental and midazolam are the typical sedatives used [310,434,435]. For patients who have advanced kidney disease, midazolam is recommended, but the dose should be reduced because more unbound drug becomes available [214,310]. Before beginning palliative sedation, the clinician should consult with a psychiatrist and pastoral services (if appropriate) and talk to the patient, family members, and other members of the healthcare team about the medical, emotional, and ethical issues surrounding the decision [67,227,310,436,437]. Formal informed consent should be obtained from the patient or from the healthcare proxy.
Physician-assisted death, or hastened death, is defined as active euthanasia (direct administration of a lethal agent with a merciful intent) or assisted suicide (aiding a patient in ending his or her life at the request of the patient) [67]. The following are not considered to be physician-assisted death: carrying out a patient's wishes to refuse treatment, withdrawal of treatment, and the use of high-dose opioids with the intent to relieve pain. The American Medical Association Code of Ethics explicitly states, "Physician-assisted suicide is fundamentally incompatible with the physician's role as healer, would be difficult or impossible to control, and would pose serious societal risks" [438]. Position statements against the use of physician-assisted death have been issued by many other professional organizations, including the NHPCO and the AAHPM [439,440]. The AAHPM states that their position is one of "studied neutrality" [439]. The basis for these declarations is that appropriate hospice care is an effective choice for providing comfort to dying patients.
In 2010, in a first-of-its-kind comprehensive consensus statement, the Heart Rhythm Society in collaboration with the major cardiology, geriatrics, and palliative care societies, emphasized that deactivation of implantable cardioverter-defibrillators is neither euthanasia nor physician-assisted death [441]. The organizations urged clinicians to respect the right of patients to request deactivation.
The 2024 NCCN guidelines advise that a request for hastened death often has important meanings that should be explored, beginning with an assessment to ensure palliative care needs are being met. This may enlarge the range of useful therapeutic options and might reduce the patient's wish to die. It is recommended clinicians explore the reasons for the request for a hastened death and determine the precipitating conditions in a joint discussion with patient, family, and caregivers [310]. During discussion, issues to consider include individual values, purpose, and meaning; worries about caregiver burden and abandonment; and views of spiritual/existential suffering (with consideration of spiritual care consultation). It is important to reassess symptom management and whether there are unrecognized patient issues, such as depression, anxiety, and delirium. It may be helpful to clarify the legal/ethical distinctions among assisted death, treatment withdrawal, and aggressive symptom management [310]. Some states have enacted assisted death statutes. State laws vary, and knowledge of your local statutes is necessary.
Ongoing communication with family members is essential to ensure their well-being as their loved one dies. The healthcare team should discuss what will happen over the course of dying so the family can be better prepared for symptoms such as altered breathing patterns and sounds, terminal delirium, and unconsciousness [6,310,430]. The family should be reassured that what they may think the patient is experiencing is not the patient's actual reality.
The altered breathing patterns that are present as death is imminent are distressful for family members, as they believe that the patient is experiencing a sense of suffocation. Also distressful to family is the sound of the death rattle. The healthcare team should assure family that these signs do not indicate that the patient is suffering and explain that additional therapy will not be of benefit.
Families often misinterpret the early signs of terminal delirium as signs of uncontrollable pain. However, if pain has been adequately managed throughout the delivery of palliative care, such pain will not begin during the last hours. As the patient slips in and out of consciousness, family members may become increasingly distressed about not being able to communicate anymore with their loved one. Although it is unknown what a dying patient can hear, other experiences in medicine suggest that awareness may be greater than the ability to respond. Family members should be encouraged to continue talking with their loved one to help them attain a sense of closure.
Despite the best efforts to prepare the family, reactions are unpredictable when death occurs. The clinician should take time to answer questions from family members, including children, and perhaps provide information on the physiologic events associated with death [67]. For family members who were not present during the death, the clinician should describe the event, while reassuring them that the patient died peacefully.
Many experts believe that people can handle grief better if they spend time with a loved one immediately after death. Family members should be allowed to touch, hold, and kiss their loved one as they feel comfortable. The healthcare team should respect the needs of the family to conduct personal, cultural, or religious traditions, rites, and rituals.
Palliative care extends beyond the patient's death, with the focus shifting to support of the family during bereavement and mourning. Although the terms "grief," "mourning," and "bereavement" are often used interchangeably, their definitions are different. Grief is a normal reaction to a loss; mourning is the process by which individuals adjust to the loss; and bereavement is the period of time during which grief and mourning occur [67,442]. Psychosocial support of the family is essential throughout the duration of palliative care and can help to decrease the risks of morbidity, substance abuse, and mortality that have been found among spouses and other loved ones of patients who have died [6].
Grief comprises a range of feelings, thoughts, and behaviors that fall in the realm of the physical, emotional, and social domains [67]. Individuals may have trouble sleeping, changes in appetite, or other physical symptoms or illness. Emotions can include sadness, anxiety, guilt, and anger. Return to work, activities with friends, and taking care of family can be beneficial.
Grief counseling for the family and patient should begin when the patient is alive, with a focus on life meaning and the contributions from the patient's family. An understanding of the mediators of the grief response can help physicians and other members of the healthcare team recognize the family members who may be at increased risk for adapting poorly to the loss [443]. These mediators are:
Nature of attachment (how close and/or dependent the individual was with regard to the patient)
Mode of death (the suddenness of the death)
Historical antecedents (how the individual has handled loss in the past)
Personality variables (factors related to age, gender, ability to express feelings)
Social factors (availability of social support, involvement in ethnic and religious groups)
Changes and concurrent stressors (number of other stressors in the individual's life, coping styles)
Prolonged grief disorder was added to the DSM-5-TR in 2022, after several decades of studies that suggested many people were experiencing persistent difficulties associated with bereavement that exceeded expected social, cultural, or religious expectations [378]. It is defined as "intense yearning or longing for the deceased (often with intense sorrow and emotional pain) and preoccupation with thoughts or memories of the deceased. In children and adolescents, this preoccupation may focus on the circumstances of the death" [378]. In adults, this intense grief must still be present one year after a loss to be considered prolonged grief disorder; in children, the timeframe is six months. Additionally, the individual with prolonged grief disorder may experience significant distress or problems performing daily activities at home, work, or other important areas [378]. Clinical assessment should be carried out for individuals at risk of prolonged grief. Distinguishing between prolonged grief disorder and major depression can be challenging, as many signs and symptoms are similar. However, the characteristic symptoms of prolonged grief disorder are [378]:
Identity disruption (e.g., feeling as though part of oneself has died)
A marked sense of disbelief about the death
Avoidance of reminders that the person is dead
Intense emotional pain (e.g., anger, bitterness, sorrow)
Difficulty reintegrating (e.g., unable to engage with friends, pursue interests, plan for the future)
Emotional numbness
Feeling that life is meaningless
Intense loneliness and feeling of being detached from others
Satisfactory adaptation to loss depends on "tasks" of mourning [443]. Previous research referred to "stages" of mourning, but the term "task" is now used because the stages were not clear-cut and were not always followed in the same order. The tasks include:
Accepting the reality of the loss
Experiencing the pain of the loss
Adjusting to the environment in which the deceased is missing (external, internal, and spiritual adjustments)
Finding a way to remember the deceased while moving forward with life
After the patient's death, members of the palliative care team should encourage the family to talk about the patient, as this promotes acceptance of the death. Explaining that a wide range of emotions is normal during the mourning process can help family members understand that experiencing these emotions is a necessary aspect of grieving. Frequent contact with family members after the loved one's death can ensure that the family is adjusting to the loss. Referrals for psychosocial and spiritual interventions should be made as early as possible to optimize their efficacy.
Bereavement support should begin immediately with a handwritten condolence note from the clinician. Such notes have been found to provide comfort to the family [444,445]. The physician should emphasize the personal strengths of the family that will help them cope with the loss and should offer help with specific issues. Attendance at the patient's funeral, if possible, is also appropriate.
How bereavement services are provided through a hospice/palliative care program vary. Programs usually involve contacting the family at regular intervals to provide resources on grieving, coping strategies, professional services, and support groups [227,310]. When notes are sent, family members should be invited to contact the physician or other members of the healthcare team with questions. Notes are especially beneficial at the time of the first holidays without the patient, significant days for the family (patient's birthday, spouse's birthday), and the anniversary of the patient's death. Bereavement services should extend for at least one year after the patient's death, but a longer period may be necessary [6,227].
The needs of some patient populations present unique challenges to the delivery of high-quality palliative care. Among these populations are older patients, including those with dementia and/or debility; children and adolescents; and patients in the critical care setting.
At present, the number of residents of nursing facilities in the United States is approaching 2 million, and that number is expected to double by 2030 [1]. Older persons comprise the largest percentage of patients who receive palliative care through hospice. In 2022, 49.4% of Medicare decedents 75 to 84 years of age and 61.8% of those 85 years of age and older used hospice [1]. The majority of older individuals receive hospice care at home, but up to 25% are residents at a nursing home or residential facility at the time of death [1,446]. A study of Medicare beneficiaries dying in nursing homes showed that between 1999 and 2006, the number of hospices providing care increased from 1,850 to 2,768, and rates of nursing home hospice use more than doubled (from 14% to 33%) [447].
The care of the frail elderly in the home is burdensome, as the long disease trajectory often requires an extended need for family caregivers. In addition, the primary caregiver may be a spouse who is older than 75 years of age and may have multiple health issues. For patients in nursing facilities, care may be fragmented, and staff often lack an appropriate understanding of pharmacology, drug addiction and dependence, management of side effects, and effective nonpharmacologic therapies [448,449,450]. Also, family members often have grief symptoms before the death of the patient; the most frequent grief symptom is yearning (separation distress) [451]. Thus, early psychosocial support and bereavement services for family are important.
Older patients, especially those with end-stage organ disease, often have substantial comorbidities and take multiple medications, both of which add to the complexity of care [104,412,452]. One study of patients with heart failure found that approximately 33% had COPD, 40% had diabetes, and more than 50% had coronary heart disease or hypertension [453]. With respect to multiple medications, a study found that older patients took an average of 6.5 medications and that 29% of the patients were taking a medication that was considered to be "never appropriate" [454]. Polypharmacy increases the likelihood of drug interactions, and clinicians should review the medication list and eliminate those drugs that are not providing clear benefit [452]. Knowledge of pharmacokinetics, pharmacodynamics, and pathophysiology are needed in making decisions to stop or adjust drugs [455]. Consulting with a pharmacist can be valuable.
As with the overall population of patients at the end of life, pain management is also inadequate for older patients, with pain experienced by more than 50% of patients at home and as many as 80% of patients in nursing facilities [456,457,458]. Studies have confirmed that older patients receive less pain medication at the end of life than younger patients and that pain management is inadequate for residents of nursing facilities [459,460,461,462]. The American Geriatrics Society has issued guidelines for the management of chronic pain for older patients, and physicians and nursing facility staff should become familiar with this resource and other guidelines for pain [458]. Improvement is also needed in the treatment of patients who have psychosocial symptoms, such as depression, agitation, anxiety, and loneliness [463].
Perhaps the greatest issue is the need for better palliative care for patients with dementia [103,448,464]. The prevalence of dementia has been reported to be 40% to 50% among persons older than 80 years of age, and many persons with dementia spend the last weeks to months of life in a nursing home [465]. Underlying dementia makes it difficult to identify symptoms, especially pain and psychosocial disorders. As a result, suffering is prevalent among patients with dementia. In fact, one study showed that 93% of patients with dementia died with an intermediate or high level of suffering [466]. The assessment of pain can be particularly challenging when the patient is unable to communicate. This situation calls for a multipronged approach consisting of observation, discussion with family and caregivers, and evaluation of the response to pain medication or nonpharmacologic measures. Recommendations for assessing pain in nonverbal patients have been developed by the American Society for Pain Management Nursing [467].
As dementia progresses, behavioral disturbances become more frequent, and symptoms include hallucinations, sleep disorders, agitation, paranoia, delusions, anxiety, and combativeness. Care should be taken to differentiate these symptoms from those associated with the underlying disease or as an adverse effect of drugs. In addition, dementia can affect the prognosis of other chronic diseases, and health events or complications such as hip fracture, pneumonia, febrile episodes, or eating problems can substantially reduce the life span for patients with advanced dementia [175,459].
The understanding of advanced dementia is limited, and as noted, the uncertainty of the disease course makes it difficult for advance care planning and referral to hospice care [175,448,468,469,470]. The progressive nature of dementia adds importance to the need for advance directives, and involvement of the family in decision making is crucial [175,471]. Educational resources about palliative care and hospice can help family and patients better understand the language needed in advance directives and the benefit of hospice services [446,471].
In an effort to enhance the quality of care at the end of life for older patients, the CAPC published the report Improving Palliative Care in Nursing Homes [472]. Based on their research, the authors of this report identified four different models for integrating preferred practices for palliative and hospice care for patients in nursing homes [472]:
Palliative Care Consult Service: Palliative care services are provided by healthcare professionals as requested by the nursing home Medical Director or Director of Nursing or the patient's attending physician.
Hospice-Based Palliative Care Consult Service: Palliative care services are provided by healthcare professionals employed at a local hospice as requested by the nursing home Medical Director or Director of Nursing or the patient's attending physician.
Nursing Home Services Integrated Palliative Care: Palliative care services are provided by staff employed directly by a nursing home that incorporates one or more of the NQF's domains of care.
Hospice Care: Specialized end-of-life palliative care services are provided by contracted hospice providers to hospice-eligible residents.
Although most physicians involved in the care of children/adolescents with life-limiting diseases are likely to make referrals for palliative or hospice care, the rate of hospice use among eligible children/adolescents is lower than that among adults, estimated at less than 10% in the United States [473,474,475]. The cause of most deaths among children is cancer, and it has been proposed that referral to hospice at the time of disease relapse would enhance the quality of care for children and their families; yet, only 2.5% of referrals are made at that time [476,477]. Instead, most hospice referrals are made at the time of disease progression (44%), at the end of therapeutic options (26%), or at the time of imminent death (20%) [476]. Similarly, most palliative care referrals are made late, with 30% to 44% of pediatricians preferring a palliative care consultation when curative therapy is no longer the goal [477].
One factor contributing to inadequate palliative/hospice care referral may be availability of appropriate services. A survey of institutions participating in Children's Oncology Group clinical trials found that a palliative care team was available in 58% of institutions and hospice care in 60% [478]. Furthermore, even when available, most services were not well used by patients [478]. In addition, many healthcare professionals are inexperienced with pediatric palliative care, and the availability of sufficiently trained pediatric hospice professionals is limited [90,473,476].
Research has identified several additional barriers to palliative care at the end of life for children/adolescents, many of which differ from those in the adult setting (Table 26) [14,90,476,477]. The sense of failure or of "giving up" may be heightened among both pediatric healthcare professionals and family members because the potential death of a child goes against the natural order. Compared with pediatric oncology professionals, parents are more likely to favor the use of aggressive treatment near the end of the child's life and consider hope a more important factor in treatment decision making [479]. As with adults, integrating palliative care early in the disease continuum can help overcome conflicts in treatment goals related to uncertainty of the prognosis [90]. Although aggressive treatment should be discontinued when it is of no benefit, the Patient Protection and Affordable Care Act of 2010 now allows for disease-directed treatment to be given concurrently with hospice [480]. (A life expectancy of six months is still a criterion for eligibility.) Clinicians usually recognize the lack of a realistic chance for cure before parents do and should talk openly with parents about discontinuing aggressive treatment and directing attention to enhancing the quality of life that remains for the child [481]. Members of the palliative care team should discuss treatment goals with the family, outline choices for interventions as the end of life draws near, and establish limits of care as the health status changes [473,482,483].
BARRIERS TO EFFECTIVE PALLIATIVE CARE FOR CHILDREN
|
The involvement of the young patient in discussions about diagnosis, prognosis, and treatment goals is another important issue in the pediatric population. Members of the healthcare team should collaborate with parents to determine how much information should be shared with the child and how involved the child should be with decision making; these determinations should be based on the child's intellectual and emotional maturity [14,484]. Many parents wish to protect their child by withholding information, but studies have shown that children often recognize the seriousness of their illness and prefer open communication about their disease and prognosis [485,486]. Such open exchange of information can help to avoid the fear of the unknown and preserve the child's trust in his or her parents and/or family and caregivers [486]. Thus, as much as possible and appropriate, the child should be allowed to participate in discussions about the direction of care [484].
When parents and clinicians involve the child in discussions, the language used should be developmentally appropriate for the child and the clinician should check often to make sure the child understands. Having the child repeat the information in his or her own words is one way to assess comprehension. When the child demonstrates an understanding of the illness and the prognosis, the emphasis should be on his or her preferences for care, and the child's preferences should be given equal weight in the decision making [472,487,488]. The physician should be an advocate for the child's preferences and decision [489].
Symptom management is a key issue in the pediatric setting. One study indicated that 89% of dying children suffered "a lot" or "a great deal" from at least one symptom in their last month of life, and other end-of-life symptoms have often been intractable [481,490]. These problems are compounded by the fact that many clinicians who provide components of pediatric palliative care do not have confidence in their ability to manage end-of-life symptoms [475]. Inadequate training and the paucity of data on symptoms in children/adolescents contribute to this lack of confidence. Few studies have been done to determine the prevalence of symptoms in children/adolescents with life-limiting diseases, the studies that do exist are in the cancer setting, and evidence-based recommendations for interventions are not available.
According to reports of parents, the most common symptoms during the last month of life are similar to those among adults; fatigue (weakness) and pain have been the most frequently reported (Table 27) [481,490,491]. When evaluating fatigue in children, age is a consideration in how fatigue is discussed. Children think about fatigue as a physical sensation, and adolescents think about fatigue as either physical and/or mental tiredness [492]. Parents or other caregivers tend to report fatigue in terms of how it interferes with the child's activities [492].
As with adults, the patient's self-report of pain is the most reliable indicator, which makes assessment particularly challenging in young children [67,493]. Pain assessment must be appropriate for each child's age, developmental level, and cultural context, and assessment tools have been developed for four age groups, from infants to 18 years of age, and for nonverbal or cognitively impaired children [494,495,496]. These tools include lists of behaviors for the parents or caregivers to rate, as well as areas for parents to provide their own rating of the child's pain and to note what has previously helped to alleviate pain (Table 28). The tools for children who are 5 years of age and older include age-appropriate items such as drawings of a child's body on which the child is asked to mark with a crayon or pencil the area that hurts and different sized circles to indicate pain intensity. A variety of pain scales (e.g., self-report scale, numerical/visual analogue scale, FACES scale) and other tools (e.g., Pediatric Pain Questionnaire) for assessing and measuring pain in children are available at https://www.aboutkidshealth.ca/Article?contentid=2994&language=English[497]. The Wong-Baker FACES scale is recommended for children who are at least 3 years of age [243]. This scale has been found to be valid and reliable for Japanese, Thai, Chinese, and Black children and has been modified for use with Alaska native children [498,499,500].
BEHAVIORS TO EVALUATE IN ASSESSING PAIN IN CHILDREN AND ADOLESCENTS
| Age of Child | Behaviors | ||||||||
|---|---|---|---|---|---|---|---|---|---|
| Infants (<1 year) |
| ||||||||
| Children (1 year and older) |
|
For children who are too young to verbally express pain, clinicians and parents must rely on behavioral cues, such as frowning, a furrowed brow, a quivering chin, crying, sucking, flexing of fingers and toes, and breath-holding in infants. Behavioral indicators in older children include decreased energy level, eating, and interest in usual activities; holding or protecting part of the body; seeking comfort or closeness; and whining or groaning [494,495,496].
Pain management according to the WHO ladder has been found to be effective for children/adolescents [502,503,504,505]. The main components of the WHO strategy include [504,505]:
Using the oral form of medication whenever possible
Dosing analgesics at regular intervals
Administering analgesics based on the severity of pain assessed using a pain-intensity scale
Tailoring medication dosing to the individual patient
Monitoring the patient carefully throughout the prescription of pain medications
Acetaminophen or NSAIDs, codeine, or oxycodone is recommended for pain rated as 0–3 on a scale of 0 to 10; an acetaminophen/opioid combination, NSAIDs, oxycodone, or morphine is recommended for pain rated as 4–6; and morphine or oxycodone is recommended for pain rated as 7–10 [187]. It is important to note that codeine may not be metabolized in 35% of children, and analgesia will be ineffective in those children [187]. Pharmacokinetic data for pediatric medications are lacking, and physicians should consult pediatric specialists for appropriate dosing of medications for symptom relief. Pain medication should be complemented by age-appropriate nonpharmacologic interventions; touch, massage, stroking, and rocking are effective for infants, toddlers, and young children, and guided imagery, music and art therapy, play therapy, controlled breathing, and relaxation techniques are beneficial for older children [493,506,507].
Attention to psychosocial support for the patient, parents, and other family members is crucial in the pediatric setting. Although most parents think that psychosocial issues should be discussed with the child's physician and would find that discussion to be valuable, fewer than half of parents raise such topics [508]. Furthermore, parents report that only 15% to 20% of physicians assess the family's psychosocial issues [508]. Among the psychosocial issues common in children/adolescents and their families are ineffective family coping strategies, the patient's relationships with peers, psychological adjustment of healthy siblings, and long-term psychological adjustment for parents [484,506,509,510,511,512,513]. The palliative care team must carefully evaluate the patient and family and provide resources and appropriate referrals.
Nearly 50% of patients who die in the hospital are in the ICU for some period of time during the last three days of life [514,515]. In addition, 13% of patients admitted to the ICU with traumatic injury will die [514]. The abruptness of a traumatic injury is vastly different from the illness trajectories of life-limiting diseases, and palliative care seems incongruous in the ICU, a high-technology environment of the most aggressive life-prolonging treatments. The effective delivery of palliative care is challenged by many factors inherent in the ICU setting, including inadequate training of healthcare professionals, unrealistic expectations of patients and families, misunderstanding of lifesaving measures, and a greater need for surrogate decision making [514,516,517]. As these factors gain greater recognition, there is a growing emphasis on integrating palliative care elements into the care of patients with traumatic injury and/or patients in an ICU [122,514,516,517,518,519].
The focus on complex, lifesaving care in the ICU creates a gap in providing relief of patients' symptoms. As in all settings, symptom assessment and management should be a priority for ICU patients. It has been suggested that an interdisciplinary palliative care assessment be carried out early in an ICU stay, preferably within 24 hours after admission, with documentation of a comprehensive care plan within 72 hours after admission [517,520].
ICU patients are often young, and families expect lifesaving procedures to be effective [517]. Misunderstanding of lifesaving measures has been reported to be an obstacle to high-quality palliative care [521]. Clinicians and other members of the team should maintain open, ongoing communication about the patient's prognosis, the feasibility of recovery, and the burden of treatment. The sudden, often catastrophic events that bring patients to the ICU compound stress and grief in family members, whose psychosocial needs peak earlier than in other palliative care settings [517]. As a result, psychosocial and bereavement support for families must begin early in the course of the patient's stay in the ICU, preferably within 24 hours after the patient's admission to the ICU [517].
The abruptness of traumatic injury or catastrophic illness is also associated with the lack of preparation of advance directives for many patients. There is often no time for planning during the short end-of-life process, and approximately 95% of patients are unable to participate in their care [517]. As a consequence, surrogates must make decisions, and such decisions have been shown to correlate poorly with the preferences of patients [522,523].
The most critical decision in the ICU setting is the withdrawal of life-support technologies. Withdrawal of mechanical ventilator support should be discussed with the family or surrogate when they (or the patient) raise the issue or when the clinician believes that the ventilator is no longer meeting the patient's goals or is more burdensome than beneficial [122]. To ease the discussion for families, the clinician should review the patient's status and care goals before discussing withdrawal of support [122]. Once the decision has been made to withdraw life support, the physician should review the process with family members, clarify the decision, ensure that the patient's spiritual and cultural context are considered, and reassure the family that comfort measures will be carried out [122,517]. Withdrawal of life support should then be immediate, not carried out over hours or days, and established protocols for withdrawal of mechanical ventilation should be followed [517,524].
Recognizing the importance of palliative care in critical care settings, the Society of Critical Care Medicine developed recommendations calling for, among other improvements, [514]:
Increased competency in all aspects of palliative care, including the use of sedatives, analgesics, and non-pharmacologic approaches to manage symptoms
Improved communication with family
Better understanding of the practical and ethical aspects of withdrawing life-sustaining treatment
Development of comprehensive bereavement programs to support both families and the needs of the clinical staff
To specifically address the needs of patients' families, the American College of Critical Care Medicine and the Society of Critical Care Medicine (SCCM) have developed guidelines for family-centered care in the ICU. The SCCM guidelines followed a rigorous, evidence-based analysis representing the state of international science in family-centered care and family support for critically ill neonatal, pediatric, and adult ICU patients [525]. The perspectives of patients and family members were incorporated through initial literature review, followed by direct consultation. In support of family-centered care, guidelines recommend endorsement of a shared decision-making model, interdisciplinary family care conferencing to reduce family stress and improve consistency in communication, culturally appropriate requests for truth-telling and informed refusal be honored, spiritual support from an adviser or chaplain, including family members in staff rounds and during resuscitation efforts, open flexible visitation, and family support before, during, and after a patient's death [525]. Other considerations include assigning family navigators to improve communication throughout the ICU stay, and proactive palliative care consultation to decrease ICU and hospital stay.
Following the initial emphasis on family-centered care in the ICU setting, the use of palliative care consultation increased 113% in one study, and from 5% to 21% in another study [24,526]. Another model that integrates palliative care into the ICU improved the quality of care and led to a higher rate of formalization of advance directives, better utilization of hospice, and a decreased use of nonbeneficial life-prolonging treatments [515].
As a result of ongoing advances in medicine, the trajectory of illness for many diseases has shifted, yielding an increasing number of patients needing palliative care throughout the continuum of care and, especially, at the end of life. High-quality palliative care focuses on the physical, psychosocial, and spiritual well-being of the patient as well as the family. Care is provided by a palliative healthcare team comprised of members who have expertise in communication, pharmacologic principles of pain management, and identification of associated psychosocial and spiritual needs. Palliative care eases the burden of suffering experienced by patients approaching life's end and provides for grief counseling and bereavement services for a family adjusting to loss. Physicians and other healthcare professionals should strive to enhance their knowledge of key strategies to achieve high-quality palliative care, as detailed in this course.
1. National Hospice and Palliative Care Organization.NHPCO Facts and Figures: Hospice Care in America, 2024 Edition. Alexandria, VA: The National Alliance for Care at Home; 2024. Available at https://www.nhpco.org/wp-content/uploads/NHPCO-Facts-Figures-2024.pdf. Last accessed October 10, 2024.
2. Field MJ, Cassel CK (eds). Approaching Death: Improving Care at the End of Life. Washington, DC: National Academies Press, 1997.
3. Mount BM. The Royal Victoria Hospital Palliative Care Service: a Canadian experience. In: Saunders C, Kastenbaum R (eds). Hospice Care on the International Scene. New York, NY: Springer; 1997: 73-85.
4. World Health Organization. Cancer Pain Relief and Palliative Care. Technical Report Series 804. Geneva: World Health Organization; 1990.
5. Payne S, Lynch T. International progress in creating palliative medicine as a specialized discipline and the development of palliative care. In: Cherny N, Fallon M, Kaasa S, Portenoy RK, Currow DC (eds). Oxford Textbook of Palliative Medicine. 5th ed. Oxford: Oxford University Press; 2017: 3.
6. National Consensus Project for Quality Palliative Care. Clinical Practice Guidelines for Quality Palliative Care. 4th ed. Richmond, VA: National Coalition for Hospice and Palliative Care; 2018.
7. World Health Organization. WHO Definition of Palliative Care. Geneva: World Health Organization; 2007.
8. Ferris F, Bruera E, Cherny N, et al. ASCO Special Article. Palliative cancer care a decade later: accomplishments, the need, next steps—from the American Society of Clinical Oncology. J Clin Oncol. 2009;27(18):3052-3058.
9. Lynn J, Adamson DM. Living Well at the End of Life: Adapting Health Care to Serious Chronic Illness in Old Age. Santa Monica, CA: Rand; 2003.
10. Pastrana T, Junger S, Ostgathe C, Elsner F, Radbruch L. A matter of definition—key elements identified in a discourse analysis of definitions of palliative care. Palliat Med. 2008;22(3):222-232.
11. National Institutes of Health. State-of-the Science Conference Statement on Improving End-of-Life Care. Available at https://consensus.nih.gov/2004/2004EndOfLifeCareSOS024html.htm. Last accessed October 9, 2024.
12. The SUPPORT Investigators. A controlled trial to improve care for seriously ill hospitalized patients in the Study to Understand Prognoses and Preferences for Outcomes and Risk of Treatments. JAMA. 1995;274:1591-1598.
13. Freeborne N, Lynn J, Desbiens NA. Insights about dying from the SUPPORT project. The Study to Understand Prognoses and Preferences for Outcomes and Risks of Treatments. J Am Geriatr Soc. 2000;48(5 Suppl):S199-S205.
14. Field MJ, Behrman RE (eds). When Children Die: Improving Palliative and End-of-Life Care for Children and Their Families. Report of the Institute of Medicine. Washington, DC: National Academies Press; 2003.
15. National Quality Forum. A National Framework and Preferred Practices for Palliative and Hospice Care Quality. A Consensus Report. Available at https://www.qualityforum.org/Publications/2006/12/A_National_Framework_and_Preferred_Practices_for_Palliative_and_Hospice_Care_Quality.aspx. Last accessed October 9, 2024.
16. Singer PA, Martin DK, Kelner M. Quality end-of-life care: patients' perspectives. JAMA. 1999;281:163-168.
17. Steinhauser K, Clipp EC, McNeilly M, et al. In search of a good death: observations of patients, families, and providers. Ann Intern Med. 2000;132:825-832.
18. Center to Advance Palliative Care. Specialty Palliative Care Certification. Available at https://www.capc.org/jobs/palliative-care-certification. Last accessed October 9, 2024.
19. National Rural Health Association. Providing Hospice and Palliative Care in Rural and Frontier Areas. Kansas City, MO: National Rural Health Association; 2005.
20. Linder JF, Meyers FJ. Palliative care for prison inmates: "Don't let me die in prison." JAMA. 2007;298(8):894-901.
21. Center to Advance Palliative Care. Designing a Long-Term Care Palliative Care Program. Available at https://www.capc.org/toolkits/starting-the-program/designing-a-long-term-care-palliative-care-program. Last accessed October 9, 2024.
22. National Hospice and Palliative Care Organization. NHPCO's Facts and Figures: Pediatric Palliative and Hospice Care in America. Alexandria, VA: National Hospice and Palliative Care Organization; 2015.
23. Mosenthal AC, Weissman DE, Curtis JR, et al. Integrating palliative care in the surgical and trauma intensive care unit: a report from the Improving Palliative Care in the Intensive Care Unit (IPAL-ICU) Project Advisory Board and the Center to Advance Palliative Care. Crit Care Med. 2012;40(4):1199-1206.
24. Villarreal D, Restrepo MI, Healy J, et al. A model of increasing palliative care in the intensive care unit: enhancing interprofessional consultation rates and communication. J Pain Symptom Manage. 2011;42(5):676-679.
25. American Society of Health-System Pharmacists. ASHP statement on the pharmacist's role in hospice and palliative care. Am J Health Syst Pharm. 2002;59:1770-1773.
26. Fine PG. The evolving and important role of anesthesiology in palliative care. Anesth Analg. 2005;100:183-188.
27. Elkington H, White P, Addington-Hall J, Higgs R, Pettinari C. The last year of life of COPD: a qualitative study of symptoms and services. Respir Med. 2004;98(5):439-445.
28. Higginson IJ, Evans CJ. What is the evidence that palliative care teams improve outcomes for cancer patients and their families? Cancer J. 2010;16(5):423-435.
29. Zimmermann C, Riechelmann R, Krzyzanowska M, Rodin G, Tannock I. Effectiveness of specialized palliative care: a systematic review. JAMA. 2008;299(14):1698-1709.
30. Ternel JS, Greer JA, Muzikansky A, et al. Early palliative care for patients with non-small-cell lung cancer. N Engl J Med. 2010;363(8):733-742.
31. Caffrey C, Sengupta M, Moss A, Harris-Kojetin L, Valverde R. Home health care and discharged hospice care patients: United States, 2000 and 2007. Natl Health Stat Report. 2011;(38):1-27.
32. Lynn J. Serving patients who may die soon and their families: the role of hospice and other services. JAMA. 2001;285(7):925-932.
33. Weckmann M. The role of the family physician in the referral and management of hospice patients. Am Fam Physician. 2008;77(6):807-812, 817-818.
34. Centers for Medicare and Medicaid Services. Medicare Hospice Benefits. CMS Pub No. 02154. Baltimore, MD: U.S. Department of Health and Human Services; 2020.
35. Epstein R, Street RL Jr. Patient-Centered Communication in Cancer Care: Promoting Healing and Reducing Suffering. NIH Publication No. 07-6225. Bethesda, MD: National Cancer Institute; 2007.
36. Tattersall M, Butow PN, Clayton JM. Insights from cancer patient communication research. Hematol Oncol Clin North Am. 2002;16:731-743.
37. de Haes H, Teunissen S. Communication in palliative care: a review of recent literature. Curr Opin Oncol. 2005;17:345-350.
38. Connor S, Elwert F, Spence C, Christakis NA. Racial disparity in hospice use in the United States in 2002. Palliat Med. 2008;22(3):205-213.
39. Cohen LL. Racial/ethnic disparities in hospice care: a systematic review. J Palliat Med. 2008;11(5):763-768.
40. Ngo-Metzger Q, Phillips RS, McCarthy EP. Ethnic disparities in hospice use among Asian-American and Pacific Islander patients dying with cancer. J Am Geriatr Soc. 2008;56(1):139-144.
41. Lepore MJ, Miller SC, Gozalo P. Hospice use among urban Black and White U.S. nursing home decedents in 2006. Gerontologist. 2011;51(2): 251-260.
42. Washington KT, Bickel-Swenson D, Stephens N. Barriers to hospice use among African Americans: a systematic review. Health Soc Work. 2008;33(4):267-274.
43. Mitchell BL, Mitchell LC. Review of the literature on cultural competence and end-of-life treatment decisions: the role of the hospitalist. J Natl Med Assoc. 2009;101(9):920-926.
44. Colon M. Hospice and Latinos: a review of the literature. J Soc Work End Life Palliat Care. 2005;1(2):27-43.
45. El-Jawahri A, Greer JA, Temel JS. Does palliative care improve outcomes for patients with incurable illness? A review of the evidence. J Support Oncol. 2011;9(3):87-94.
46. Brumley R, Enquidanos S, Jamison P, et al. Increased satisfaction with care and lower costs: results of a randomized trial of in-home palliative care. J Am Geriatr Soc. 2007;55(7):993-1000.
47. Qaseem A, Snow V, Shekelle P, et al. Evidence-based interventions to improve the palliative care of pain, dyspnea, and depression at the end of life: a clinical practice guideline from the American College of Physicians. Ann Intern Med. 2008;148(2):141-146.
48. Casarett D, Pickard A, Bailey FA, et al. A nationwide VA palliative care quality measure: the family assessment of treatment at the end of life. J Palliat Med. 2008;11(1):68-75.
49. Gelfman LP, Meier DE, Morrison RS. Does palliative care improve quality? A survey of bereaved family members. J Pain Symptom Manage. 2008;36(1):22-28.
50. Abernethy AP, Currow DC, Fazekas BS, Luszcz MA, Wheeler JL, Kuchibhatla M. Specialized palliative care services are associated with improved short- and long-term caregiver outcomes. Support Care Cancer. 2008;16(6):585-597.
51. Connor S, Pyenson B, Fitch K, Spence C, Iwasaki K. Comparing hospice and nonhospice patient survival among patients who die within a three-year window. J Pain Symptom Manage. 2007;33(3):238-246.
52. Saito AM, Landrum MB, Neville BA, Ayanian JZ, Weeks JC, Earle CC. Hospice care and survival among elderly patients with lung cancer. J Palliat Med. 2011;14(8):929-939.
53. Smith TJ, Temin S, Alesi ER, et al. American Society of Clinical Oncology provisional clinical opinion: the integration of palliative care into standard oncology care. J Clin Oncol. 2012;30(8):880-887.
54. Ford DW, Koch KA, Ray DE, Selecky PA. Palliative and end-of-life care in lung cancer: diagnosis and management of lung cancer, 3rd ed. American College of Chest Physicians evidence-based clinical practice guidelines. Chest. 2013;143(5_Suppl):e498S-e512S.
55. Goodman DC, Esty AR, Fisher ES, Chang C-H. Trends and Variation in End-of-Life Care for Medicare Beneficiaries with Severe Chronic Illness: A Report of the Dartmouth Atlas Project. Available at https://data.dartmouthatlas.org/downloads/reports/EOL_Trend_Report_0411.pdf. Last accessed October 9, 2024.
56. Zhang B, Wright AA, Huskamp HA, et al. Health care costs in the last week of life. Arch Intern Med. 2009;169(5):480-488.
58. Emanuel E, Ash A, Yu W, et al. Managed care, hospice use, site of death, and medical expenditures in the last year of life. Arch Intern Med. 2002;162(15):1722-1728.
59. Taylor D, Ostermann J, Van Houtven CH, Tulsky JA, Steinhauser K. What length of hospice use maximizes reduction in medical expenditures near death in the US Medicare program? Soc Sci Med. 2007;65:1466-1478.
60. Morrison RS, Dietrich J, Ladwig S, et al. Palliative care consultation teams cut hospital costs for Medicaid beneficiaries. Health Aff. 2011;30(3):454-463.
61. Bekelman DB, Havranek EP. Palliative care for patients with acute decompensated heart failure: an underused service? Nat Clin Pract Cardiovasc Med. 2008;5(5):250-251.
62. Curtis JR. Palliative and end-of-life care for patients with severe COPD. Eur Respir J. 2008;32(3):796-803.
63. Roberts C, Seiger A, Buckingham R, Stone R. Clinician perceived good practice in end-of-life care for patients with COPD. Palliat Med. 2008;22(7):855-858.
64. Berzoff J, Swantkowski J, Cohen LM. Developing a renal supportive care team from the voices of patients, families, and palliative care staff. Palliat Support Care. 2008;6(2):133-139.
65. Jablonski A. Palliative care: misconceptions that limit access for patients with chronic renal disease. Semin Dial. 2008;21(3):206-209.
66. Hinds PS, Oakes LL, Hicks J, Anghelescu DL. End-of-life care for children and adolescents. Semin Oncol Nurs. 2005;21(1):53-62.
67. Berger AM, O'Neill JF (eds). Principles & Practice of Palliative Care & Supportive Oncology. 5th ed. Philadelphia, PA: Lippincott Williams & Wilkins; 2022.
68. Ross DD, Shpritz D, Hull MM, Goloubeva O. Long-term evaluation of required coursework in palliative and end-of-life care for medical students. J Palliat Med. 2005;8:962-974.
69. Scharfenberger J, Furman CD, Rotella J, Pfeifer M. Meeting American Council of Graduate Medical Education guidelines for a palliative medicine fellowship through diverse community partnerships. J Palliat Med. 2008;11(3):428-430.
70. American Medical Association. FREIDA. Available at https://freida.ama-assn.org/. Last accessed October 9, 2024.
71. American Academy of Hospice and Palliative Medicine. Certification for Hospice and Palliative Medicine Specialists: History of Certification. Available at http://aahpm.org/career/certification. Last accessed October 9, 2024.
72. Quigley L, Salsberg E, Lupu D, American Academy of Hospice and Palliative Medicine. Profile of Active Hospice and Palliative Medicine Physicians, 2016. Available at http://aahpm.org/uploads/Profile_of_Active_HPM_Physicians_September_2017.pdf. Last accessed October 9, 2024.
73. American Board of Medical Specialties. ABMS Board Certification Report 2023–2024. Available at https://www.abms.org/wp-content/uploads/2024/09/2023_24_ABMSCertReport_REVISED-9-23-24.pdf. Last accessed October 1, 2024.
74. Wilkinson S, Perry R, Blanchard K, Linsell L. Effectiveness of a three-day communication skills course in changing nurses' communication skills with cancer/palliative care patients: a randomised controlled trial. Palliat Med. 2008;22(4):365-375.
75. National Board for Certification in Hospice and Palliative Care Nurses. August 2015 HPCC Certification Newsletter: Results of the June 2017 Exam. Available at https://myemail.constantcontact.com/Certification-Newsletter-from-HPCC---August-2017.html?soid=1109774303066&aid=eETO3RPGibQ. Last accessed October 9, 2024.
76. National Hospice Organization. Medical guidelines for determining prognosis in selected non-cancer diseases. Hosp J. 1996;11(2):47-63.
77. Lutz S, Spence C, Chow E, et al. Survey on use of palliative radiotherapy in hospice care. J Clin Oncol. 2004;22:3581-3586.
78. McCloskey S, Tao ML, Rose CM, Fink A, Amadeo AM. National survey of perspectives of palliative radiation therapy: role, barriers, and needs. Cancer J. 2007;13(2):130-137.
79. Jarosek SL, Virnig BA, Feldman R. Palliative radiotherapy in Medicare-certified freestanding hospices. J Pain Symptom Manage. 2009;37(5):780-787.
80. Wright A, Katz IT. Letting go of the rope—aggressive treatment, hospice care, and open access. N Engl J Med. 2007;357:324-327.
81. Finlay E, Casarett D. Making difficult decisions easier: using prognosis to facilitate transitions to hospice. Ca Cancer J Clin. 2009;59:250-263.
83. Salz T, Brewer NT. Offering chemotherapy and hospice jointly: one solution to hospice underuse. Med Decis Making. 2009;29(4):521-531.
85. Centers for Medicare and Medicaid. Medicare Care Choices Model, Fifth and Final Annual Evaluation Report (2016–2021). Available at https://www.cms.gov/priorities/innovation/data-and-reports/2023/mccm-fg-fifthannrpt. Last accessed October 10, 2024.
86. Medicare Learning Network. MLN Fact Sheet: Advance Care Planning. Available at https://www.cms.gov/outreach-and-education/medicare-learning-network-mln/mlnproducts/downloads/advancecareplanning.pdf. Last accessed October 9, 2024.
87. Belanger E, Loomer L, Teno JM. Early utilization patterns of the new Medicare procedure codes for advance care planning. JAMA Intern Med. 2019;179(6):829-830.
88. Brickner L, Scannell K, Marquet S, Ackerson L. Barriers to hospice care and referrals: survey of physicians' knowledge, attitudes, and perceptions in a health maintenance organization. J Palliat Med. 2004;7(3):411-418.
89. Hauptman P, Swindle J, Hussain Z, Biener L, Burroughs TE. Physician attitudes toward end-stage heart failure: a national survey. Am J Med. 2008;121:127-135.
90. Davies B, Sehring SA, Partridge JC, et al. Barriers to palliative care for children: perceptions of pediatric health care providers. Pediatrics. 2008;121(2):282-288.
91. Twomey F, O'Leary N, O'Brien T. Prediction of patient survival by healthcare professionals in a specialist palliative care inpatient unit: a prospective study. Am J Hosp Palliat Care. 2008;25(2):139-145.
92. Glare PA, Sinclair CT. Palliative medicine review: prognostication. J Palliat Med. 2008;11:84-103.
93. Christakis NA, Lamont EB. Extent and determinants of error in doctors' prognoses in terminally ill patients: prospective cohort study. BMJ. 2000;320:469-472.
94. Joshi K, Guthmann R, Kishman C. How do we decide when a patient with nonmalignant disease is eligible for hospice care? Family Pract. 2006;55(6).
95. Boyd K, Murray SA. Recognising and managing key transitions in end of life care. BMJ. 2010;341:c4863.
96. Glare P, Virik K, Jones M, et al. A systematic review of physicians' survival predictions in terminally ill cancer patients. BMJ. 2003;327(7408):195-198.
97. Alexander M, Christakis NA. Bias and asymmetric loss in expert forecasts: a study of physician prognostic behavior with respect to patient survival. J Health Econ. 2008;27:1095-1108.
98. Casarett DJ, Quill TE. "I'm not ready for hospice:" strategies for timely and effective hospice discussions. Ann Intern Med. 2007;146(6):443-449.
99. Coventry PA, Grande GE, Richards DA, Todd CJ. Prediction of appropriate timing of palliative care for older adults with non-malignant life-threatening disease: a systematic review. Age Aging. 2005;34:218-227.
100. Lunney JR, Lynn J, Hogan C. Profiles of older Medicare decedents. J Am Geriatr Soc. 2002;50(6):1108-1112.
101. Spence A, Hasson F, Waldron M, et al. Professionals delivering palliative care to people with COPD: qualitative study. Palliat Med. 2009;23(2):126-131.
102. McClung J. End-of-life care in the treatment of heart failure in the elderly. Clin Geriatr Med. 2007;23:235-248.
103. Birch D, Draper J. A critical literature review exploring the challenges of delivering effective palliative care to older people with dementia. J Clin Nurs. 2008;17(9):1144-1163.
104. Kapo J, Morrison LJ, Liao S. Palliative care for the older adult. J Palliat Med. 2007;10(1):185-209.
105. Knaus WA, Harrerll FE, Lynn J et al. The SUPPORT prognostic model. Objective estimates of survival for seriously ill hospitalised adults. Ann Intern Med. 1995;122:191-203.
106. Pirovano M, Maltoni M, Nanni O, et al. A new palliative prognostic score: a first step for the staging of terminally ill cancer patients. J Pain Symptom Manage. 1999;17(4):231-239.
107. Morita T, Tsunoda J, Inoue S, et al. The Palliative Prognostic Index: a scoring system for survival prediction of terminally ill cancer patients. Support Care Cancer. 1999;7(3):128-133.
108. Adler ED, Goldfinger JZ, Park ME, Meier DE. Palliative care in the treatment of advanced heart failure. Circulation. 2009;120: 2597-2606.
109. Levy W, Mozaffarian D, Linker DT, et al. The Seattle Heart Failure model: prediction of survival in heart failure. Circulation. 2006;113:1424-1433.
110. Feliu J, Jimenez-Gordo AM, Madero R, et al. Development and validation of a prognostic nomogram for terminally ill cancer patients. J Natl Cancer Inst. 2011;103(21):1613-1620.
111. Mitchell SL, Miller SC, Teno JM, Kiely DK, Davis RB, Shaffer ML. Prediction of 6-month survival of nursing home residents with advanced dementia using ADEPT vs hospice eligibility guidelines. JAMA. 2010;304(17):1929-1935.
112. Han PK, Lee M, Reeve BB, et al. Development of a prognostic model for six-month mortality in older adults with declining health. J Pain Symptom Manage. 2012;43(3):527-539.
113. Institute for Clinical Systems Improvement. Palliative Care for Adults, 6th ed. Available at https://www.icsi.org/guideline/palliative-care/. Last accessed October 9, 2024.
114. Bergman J, Saigal CS, Lorenz KA, et al. Hospice use and high-intensity care in men dying of prostate cancer. Arch Intern Med. 2011;171(3):204-210.
115. Haupt BJ. Characteristics of hospice care discharges and their length of service: United States, 2000. Vital Health Stat. 2003;(154): 1-36.
116. Teno JM, Shu JE, Casarett D, Spence C, Rhodes R, Connor S. Timing of referral to hospice and quality of care: length of stay and bereaved family members' perceptions of the timing of hospice referral. J Pain Symptom Manage. 2007;34(2):120-125.
117. Clayton JM, Hancock KM, Butow PN, et al. Clinical practice guidelines for communicating prognosis and end-of-life issues with adults in the advanced stages of a life-limiting illness, and their caregivers. Med J Aust. 2007;188(12 Suppl):S77, S79, S83-S108.
118. Weissman DE, Meier DE. Identifying patients in need of a palliative care assessment in the hospital setting: a consensus report from the Center to Advance Palliative Care. J Palliat Med. 2011;14(1):17-23.
119. Swetz KM, Freeman MR, AbouEzzeddine OF, et al. Palliative medicine consultation for preparedness planning in patients receiving left ventricular assist devices as destination therapy. Mayo Clin Proc. 2011;86(6):493-500.
120. Swetz KM, Ottenberg AL, Freeman MR, Mueller PS. Palliative care and end-of-life issues in patients treated with left ventricular assist devices as destination therapy. Curr Heart Fail Rep. 2011;8(3):212-218.
121. Renal Physicians Association. Shared Decision-Making in the Appropriate Initiation and Withdrawal from Dialysis. Clinical Practice Guideline. 2nd ed. Rockville, MD: Renal Physicians Association; 2010.
122. Lanken PN, Terry PB, Delisser HM, et al. An official American Thoracic Society clinical policy statement: palliative care for patients with respiratory diseases and critical illnesses. Am J Respir Crit Care Med. 2008;177(8):912-927.
123. Larson AM, Curtis JR. Integrating palliative care for liver transplant candidates: "too well for transplant, too sick for life." JAMA. 2006;295(108):2168-2176.
124. Center to Advance Palliative Care. 2011 Public Opinion Research on Palliative Care: A Report Based on Research by Public Opinion Strategies. New York, NY: Center to Advance Palliative Care; 2011.
125. Cambia Health Foundation. National Poll – "Conversation Stopper: What's Preventing Physicians from Talking with Patients about End-Of-Life and Advance Care Planing?". Available at https://www.cambiahealthfoundation.org/posts/news/2016-04-14/national-poll---conversation-stopper--whats-preventin.html. Last accessed October 9, 2024.
126. Davison SN, Jhangri GS. Impact of pain and symptom burden on the health-related quality of life of hemodialysis patients. J Pain Symptom Manage. 2010;39(3):477-485.
127. Naierman N, Turner J. Debunking the Myths of Hospice. Available at https://americanhospice.org/learning-about-hospice/debunking-the-myths-of-hospice. Last accessed October 9, 2024.
128. McGorty E, Bornstein BH. Barriers to physicians' decisions to discuss hospice: insights gained from the United States hospice model. J Eval Clin Pract. 2003;9:363-372.
129. Balaban RB. A physician's guide to talking about end-of-life care. J Gen Intern Med. 2000;15:195-200.
130. Ngo-Metzger Q, August KJ, Srinivasan M, Liao S, Meyskens FL Jr. End-of-life care: guidelines for patient-centered communication. Am Fam Physician. 2008;77(2):167-174.
131. Larochelle MR, Rodriguez KL, Arnold RM, Barnato AE. Hospital staff attributions of the causes of physician variation in end-of-life treatment intensity. Palliat Med. 2009;23(5):460-470.
132. Office of Minority Health. Cultural and Linguistic Competency. Available at https://minorityhealth.hhs.gov/omh/browse.aspx?lvl=1&lvlid=6. Last accessed October 9, 2024.
133. Paez K, Allen JK, Beach MC, Carson KA, Cooper LA. Physician cultural competence and patient ratings of the patient-physician relationship. J Gen Intern Med. 2009;24(4):495-498.
134. Powers BJ, Trinh JV, Bosworth HB. Can this patient read and understand written health information? JAMA. 2010;304(1):76-84.
135. U.S. Census Bureau. Selected Social Characteristics in the United States: 2019. Available at https://data.census.gov/cedsci/table?q=selected%20social%20charasteristics&tid=ACSDP1Y2019.DP02. Last accessed October 9, 2024.
136. Karliner L, Napoles-Springer AM, Schillinger D, Bibbins-Domingo K, Pérez-Stable EJ. Identification of limited English proficient patients in clinical care. J Gen Intern Med. 2008;23(10):1555-1560.
137. Flores G. The impact of medical interpreter services on the quality of health care: a systematic review. Med Care Res Rev. 2005;62(3):255-299.
138. Karliner L, Jacobs EA, Chen AH, Mutha S. Do professional interpreters improve clinical care for patients with limited English proficiency? A systematic review of the literature. Health Serv Res. 2007;42(2):727-754.
139. Ngo-Metzger Q, Massagli MP, Clarridge BR, et al. Linguistic and cultural barriers to care: perspectives of Chinese and Vietnamese immigrants. J Gen Intern Med. 2003;18(1):44-52.
140. Norris WM, Wenrich MD, Nielsen EL, Treece PD, Jackson JC, Curtis JR. Communication about end-of-life care between language-discordant patients and clinicians: insights from medical interpreters. J Palliat Med. 2005;8(5):1016-1024.
141. Committee on Health Literacy, Board on Neuroscience and Behavioral Health. Health Literacy: A Prescription to End Confusion. Washington, DC: The National Academies Press; 2004.
142. Paasche-Orlow MK, Parker RM, Gazmararian JA, Nielsen-Bohlman LT, Rudd RR. The prevalence of limited health literacy. J Gen Intern Med. 2005;20(2):175-184.
143. Kutner M, Greenberg E, Jin,Y, Paulsen C, White S. The Health Literacy of America's Adults: Results from the 2003 National Assessment of Adult Literacy. Washington, DC: National Center for Education Statistics; 2006.
144. Shah LC, West P, Bremmeyr K, Savoy-Moore RT. Health literacy instrument in family medicine: the "newest vital sign" ease of use and correlates. J Am Board Fam Med. 2010;23(2):195-203.
145. Weiss B, Mays MZ, Martz W, et al. Quick assessment of literacy in primary care: the newest vital sign. Ann Fam Med. 2005;3:514-522.
146. Crawley LM, Marshall PA, Lo B, Koenig BA, for the End-of-Life Care Consensus Panel. Strategies for culturally effective end-of-life care. Ann Intern Med. 2002;136(9):673-679.
147. Shanawani H, Wenrich MD, Tonelli MR, Curtis JR. Meeting physicians' responsibilities in providing end-of-life care. Chest. 2008;133(3):775-786.
148. Quill TE. Initiating end-of-life discussions with seriously ill patients: addressing the "elephant in the room." JAMA. 2000;284(19):2502-2507.
149. Parker SM, Clayton JM, Hancock K, et al. A systematic review of prognostic/end-of-life communication with adults in the advanced stages of a life-limiting illness: patient/caregiver preferences for the content, style, and timing of information. J Pain Symptom Manage. 2007;34(1):81-93.
150. Werb R. Palliative care in the treatment of end-stage renal failure. Prim Care Clin Office Pract. 2011;38:299-309.
151. Mack JW, Weeks JC, Wright AA, Block SD, Prigerson HG. End-of-life discussions, goal attainment, and distress at the end of life: predictors and outcomes of receipt of care consistent with preferences. J Clin Oncol. 2010;28(7):1203-1208.
152. Wright AA, Zhang B, Ray A, et al. Associations between end-of-life discussions, patient mental health, medical care near death, and caregiver bereavement adjustment. JAMA. 2008;300(14):1665-1673.
153. Huskamp HA, Keating NL, Malin JL, et al. Discussions with physicians about hospice among patients with metastatic lung cancer. Arch Intern Med. 2009;169(10):954-962.
154. Curtis J, Engelberg RA, Nielsen EL, et al. Patient-physician communication about end-of-life care for patients with severe COPD. Eur Respir J. 2004;24(2):200-205.
155. Reinke LF, Slatore CG, Uman J, et al. Patient-clinician communication about end-of-life care topics: is anyone talking to patients with chronic obstructive pulmonary disease? J Palliat Med. 2011;14(8):923-928.
156. Halliwell J, Mulcahy P, Buetow S, Bray Y, Coster G, Osman LM. GP discussion of prognosis with patients with severe chronic obstructive pulmonary disease: a qualitative study. Br J Gen Pract. 2004;54(509):904-908.
157. Keating NL, Landrum MB, Rogers SO Jr, et al. Physician factors associated with discussions about end-of-life care. Cancer. 2010;116(4):998-1006.
158. Jessup M, Abraham WT, Casey DE, et al. 2009 focused update: ACCF/AHA guidelines for the diagnosis and management of heart failure in adults. Circulation. 2009;119:1977-2016.
159. Yancy CW, Jessup M, Bozkurt B, et al. 2013 ACCF/AHA guideline for the management of heart failure: a report of the American College of Cardiology Foundation/American Heart Association Task Force on practice guidelines. Circulation. 2013;128(16):e240-e327.
160. Hancock K, Clayton JM, Parker SM, et al. Truth-telling in discussing prognosis in advanced life-limiting illnesses: a systematic review. Palliat Med. 2007;21(6):507-517.
161. Wailing A, Lorenz KA, Dy SM, et al. Evidence-based recommendations for information and care planning in cancer care. J Clin Oncol. 2008;26(23):3896-3902.
163. Baile WF, Buckman R, Lenzi R, Glober G, Beale EA, Kudelka AP. SPIKES—A six-step protocol for delivering bad news: application to the patient with cancer. Oncologist. 2000;5:302-311.
164. Buckman R. Communication skills in palliative care: a practical guide. Neurol Clin. 2001;19(4):989-1004.
165. Back AL, Arnold RM, Baile WF, Tulsky JA, Fryer-Edwards K. Approaching difficult communication tasks in oncology. CA Cancer J Clin. 2005;55:164-177.
166. Hancock K, Clayton JM, Parker SM, et al. Discrepant perceptions about end-of-life communication: a systematic review. J Pain Symptom Manage. 2007;34(2):190-200.
167. Moore PM, Mercado SR, Artigues MG, Lawrie TA. Communication skills training for healthcare professionals working with people who have cancer. Cochrane Database Syst Rev. 2013;(3):CD003751.
168. Back AL, Arnold RM, Baile WF, et al. Efficacy of communication skills training for giving bad news and discussing transitions to palliative care. Arch Intern Med. 2007;167(5):453-460.
169. Clayton JM, Butow PN, Tattersall MNH, et al. Randomized controlled trial of a prompt list to help advanced cancer patients and their caregivers to ask questions about prognosis and end-of-life care. J Clin Oncol. 2007;25(6):715-723.
170. Au DH, Udris EM, Engelberg RA, et al. A randomized trial to improve communication about end-of-life care among patients with COPD. Chest. 2012;141(3):726-735.
171. Brink P, Smith TF, Kitson M. Determinants of do-not-resuscitate orders in palliative home care. J Palliat Med. 2008;11(2):226-232.
172. Swetz KM, Ottenberg AL, Freeman MR, Mueller PS. Palliative care and end-of-life issues in patients treated with left ventricular assist devices as destination therapy. Curr Heart Fail Rep. 2011;8(3):212-218.
173. Swetz KM, Freeman MR, AbouEzzeddine OF, et al. Palliative medicine consultation for preparedness planning in patients receiving left ventricular assist devices as destination therapy. Mayo Clin Proc. 2011;86(6):493-500.
174. O'Connor NR, Kumar P. Conservative management of end-stage renal disease without dialysis: a systematic review. J Palliat Med. 2012;15(2):228-235.
175. Stapleton R, Curtis JR. End-of-life considerations in older patients who have lung disease. Clin Chest Med. 2007;28:801-811.
176. Audrey S, Abel J, Blazeby JM, Falk S, Campbell R. What oncologists tell patients about survival benefits of palliative chemotherapy and implications for informed consent: qualitative study. BMJ. 2008;337:a752.
177. Goldstein N, Lampert R, Bradley E, et al. Management of implantable cardioverter defibrillators in end-of-life care. Ann Intern Med. 2004;141:835-838.
178. Smith TJ, Hillner BE. Bending the cost curve in cancer care. N Engl J Med. 2011;364(21):2060-2065.
179. Weeks JC, Cook EF, O'Day SJ, et al. Relationship between cancer patients' predictions of prognosis and their treatment preferences. JAMA. 1998;279(21):1709-1714.
180. Sheffield KM, Boyd CA, Benarroch-Gampel J, Kuo YF, Cooksley CD, Riall TS. End-of-life care in Medicare beneficiaries dying with pancreatic cancer. Cancer. 2011;117(21):5003-5012.
181. Unroe KT, Greiner MA, Hernandez AF, et al. Resource use in the last 6 months of life among Medicare beneficiaries with heart failure, 2000–2007. Arch Intern Med. 2011;171(3):196-203.
182. Earle C, Neville BA, Landrum MB, et al. Trends in the aggressiveness of cancer care near the end of life. J Clin Oncol. 2004;22:315-321.
183. Kao S, Shafiq J, Vardy J, Adams D. Use of chemotherapy at end of life in oncology patients. Ann Oncol. 2009;20(9):1555-1559.
184. Saito AM, Landrum MB, Neville BA, Zyanian JZ, Earle CC. The effect on survival of continuing chemotherapy to near death. BMC Palliat Care. 2011;10:14.
185. Curtis JR, Engelberg RA. What is the "right" intensity of care at the end of life and how do we get there? [editorial]. Ann Intern Med. 2011;154(4):283-284.
186. Smith L. Guidelines for delivering quality palliative care. Am Fam Physician. 2006;73(6):1105-1111.
187. National Comprehensive Cancer Network. NCCN Guidelines Version 2.2024 Adult Cancer Pain. Available at https://www.nccn.org/professionals/physician_gls/pdf/pain.pdf. Last accessed October 4, 2024.
188. McCabe M, Storm C. When doctors and patients disagree about medical futility. J Oncol Pract. 2008;4(4):207-209.
189. Smith CB, Bunch O'Neill L. Do not resuscitate does not mean do not treat: how palliative care and other modalities can help facilitate communication about goals of care in advanced illness. Mt Sinai J Med. 2008;75(5):460-465.
190. Lee D, Austin PC, Stukel TA, et al. "Dose-dependent" impact of recurrent cardiac events on mortality in patients with heart failure. Am J Med. 2009;122(2):162-169.
191. Holley J. Palliative care in end-stage renal disease: illness trajectories, communication, and hospice use. Adv Chronic Kidney Dis. 2007;14(4):402-408.
192. Peppercorn JM, Smith TJ, Helft PR, et al. American Society of Clinical Oncology statement: toward individualized care for patients with advanced cancer. J Clin Oncol. 2011;29(6):755-760.
193. Torke AM, Siegler M, Abalos A, Moloney RM, Alexander GC. Physicians' experience with surrogate decision making for hospitalized adults. J Gen Intern Med. 2009;24(9):1023-1028.
194. Silveira MJ, Kim SY, Langa KM. Advance directives and outcomes of surrogate decision making before death. N Engl J Med. 2010;362(13):1211-1218.
195. Nicholas LN, Langa KM, Iwashyna TJ, Weir DR. Regional variation in the association between advance directives and end-of-life Medicare expenditures. JAMA. 2011;306(13):1447-1453.
196. Teno JM, Licks S, Lynn J, et al. Do advance directives provide instructions that direct care? SUPPORT Investigators. Study to Understand Prognoses and Preferences for Outcomes and Risks of Treatment. J Am Geriatr Soc. 1997;45(4):508-512.
197. Olick RS. Defining features of advance directives in law and clinical practice. Chest. 2012;14(1):232-238.
199. Reynolds K, Hanson LC, Henderson M, Steinhauser KE. End-of-life care in nursing home settings: do race or age matter? Palliat Support Care. 2008;6(1):21-27.
200. Kwak J, Haley WE. Current research findings on end-of-life decision making among racially or ethnically diverse groups. Gerontologist. 2005;45(5):634-641.
201. Sanchez W, Walwalkar JA. Palliative care for patients with end-stage liver disease ineligible for liver transplantation. Gastroenterol Clin North Am. 2006;35(1):201-219.
202. Stein G, Bonuck KA. Attitudes on end-of-life care and advance care planning in the lesbian and gay community. J Palliat Med. 2001;4(2):173-190.
203. Center for Ethics in Health Care, Oregon Health and Science University. Oregon POLST Program. Available at https://www.ohsu.edu/center-for-ethics/oregon-polst-program. Last accessed October 9, 2024.
204. Hickman SE, Nelson CA, Moss AH, et al. Use of the Physicians Orders for Life-Sustaining Treatment (POLST) paradigm program in the hospice setting. J Palliat Med. 2009;12(2):133-141.
205. Fromme EK, Zive D, Schmidt TA, Olszewski E, Tolle SW. POLST registry do-not-resuscitate orders and other patient treatment preferences [research letter]. JAMA. 2012;307(1):34-35.
206. Doyle D, Woodruff R. The IAHPC Manual of Palliative Care. 3rd ed. Houston, TX: International Association for Hospice and Palliative Care Press; 2013.
207. Blinderman CD, Homel P, Billings JA, Portenoy RK, Tennstedt SL. Symptom distress and quality of life in patients with advanced congestive heart failure. J Pain Symptom Manage. 2008;35(6):594-603.
208. Bekelman DB, Rumsfeld JS, Havranek EP, et al. Symptom burden, depression, and spiritual well-being: a comparison of heart failure and advanced cancer patients. J Gen Intern Med. 2009;24(5):592-598.
209. Blinderman CD, Homel P, Billings JA, Tennstedt S, Portenoy RK. Symptom distress and quality of life in patients with advanced chronic obstructive pulmonary disease. J Pain Symptom Manage. 2009;38(1):115-123.
210. Murtagh F, Addington-Hall JM, Higginson IJ. The prevalence of symptoms in end-stage renal disease: a systematic review. Adv Chronic Kidney Dis. 2007;14(1):82-99.
211. Solano J, Gomes B, Higginson IJ. A comparison of symptom prevalence in far advanced cancer, AIDS, heart disease, chronic obstructive pulmonary disease and renal disease. J Pain Symptom Manage. 2006;31:58-69.
212. Lorenz KA, Lynn J, Dy SM, et al. Evidence for improving palliative care at the end of life: a systematic review. Ann Intern Med. 2008;148(2):147-159.
213. Mahler DA, Selecky PA, Harrod CG, et al. American College of Chest Physicians consensus statement on the management of dyspnea in patients with advanced lung or heart disease. Chest. 2010;137(3):674-691.
214. Douglas C, Murtagh FE, Chambers EJ, Howse M, Ellershaw J. Symptom management for the adult patient dying with advanced chronic kidney disease: a review of the literature and development of evidence-based guidelines by a United Kingdom Expert Consensus Group. Palliat Med. 2009;23(2):103-110.
215. Hui D, Mori M, Parsons HA, et al. The lack of standard definitions in the supportive and palliative oncology literature. J Pain Symptom Manage. 2012;43(3):582-592.
216. Shah M, Quill T, Norton S, Sada Y, Buckley M, Fridd C. "What bothers you the most?" Initial responses from patients receiving palliative care consultation. Am J Hosp Palliat Care. 2008;25(2):88-92.
217. Esther Kim J-E, Dodd MJ, Aouizerat BE, Jahan T, Miaskowski C. A review of the prevalence and impact of multiple symptoms in oncology patients. J Pain Symptom Manage. 2009;37(4):715-736.
218. Teno J. Toolkit of Instruments to Measure End-of-Life Care (TIME). Available at www.chcr.brown.edu/pcoc/resourceguide/resourceguide.pdf. Last accessed October 9, 2024.
219. Mularski RA, Dy SM, Shugarman LR, et al. A systematic review of measures of end-of-life care and its outcomes. Health Serv Res. 2007;42(5):1848-1870.
220. Hoekstra J, Vernooij-Dassen MJ, de Vos R, Bindels PJ. The added value of assessing the "most troublesome" symptom among patients with cancer in the palliative phase. Patient Educ Couns. 2007;65(2):223-229.
221. Homsi J, Walsh D, Rivera N, et al. Symptom evaluation in palliative medicine: patient report vs. systematic assessment. Support Care Cancer. 2006;14(5):444-453.
222. American Pain Foundation. Breakthrough cancer pain: mending the break in the continuum of care. J Pain and Palliat Care Pharmacother. 2011;25(3):252-264.
223. Dalal S, Bruera E. Assessment and management of pain in the terminally ill. Prim Care Clin Office Pract. 2011;38:195-223.
224. Gao W, Gulliford M, Higginson IJ. Prescription patterns of analgesics in the last 3 months of life: a retrospective analysis of 10,202 lung cancer patients. Br J Cancer. 2011;104(11):1704-1710.
225. Godfrey C, Harrison MB, Medves J, Tranmer JE. The symptom of pain with heart failure: a systematic review. J Card Fail. 2006;12(4):307-313.
226. Breuer B, Fleishman SB, Cruciani RA, Portenoy RK. Medical oncologists' attitudes and practice in cancer pain management: a national survey. J Clin Oncol. 2011;29(36):4769-4775.
227. Abrahm JL. A Physician's Guide to Pain and Symptom Management in Cancer Patients. 3rd ed. Baltimore, MD: Johns Hopkins University Press; 2014.
229. Zerzan J, Lee CA, Haverhals LM, Nowels CT. Exploring physician decisions about end-of-life opiate prescribing: a qualitative study. J Palliat Med. 2011;14(5):567-572.
230. Fineberg IC, Wenger NS, Brown-Saltzman K. Unrestricted opiate administration for pain and suffering at the end of life: knowledge and attitudes as barriers to care. J Palliat Med. 2006;9(4):873-883.
231. Mezei L, Murinson BB, Johns Hopkins Pain Curriculum Development Team. Pain education in North American medical schools. J Pain. 2011;12(12):1199-1208.
232. Schmidt C. Experts worry about chilling effect of federal regulations on treating pain. J Natl Cancer Inst. 2005;97(8):554-555.
233. American Medical Association. Ethics: Withholding or Withdrawing Life-Sustaining Treatment: Code of Medical Ethics Opinion 5.3. Available at https://www.ama-assn.org/delivering-care/ethics/withholding-or-withdrawing-life-sustaining-treatment. Last accessed October 9, 2024.
234. American Medical Association. Caring for Patients at the End of Life. Available at https://www.ama-assn.org/delivering-care/ethics/caring-patients-end-life. Last accessed October 9, 2024.
235. Bagdasarian N. A prescription for mental distress: the principles of psychosomatic medicine with the physical manifestation requirement in NIED cases. Am J Law Med. 2000;26:401-438.
236. Congress.Gov. S.3397 – Secure and Responsible Drug Disposal Act of 2010. Available at https://www.congress.gov/bill/111th-congress/senate-bill/3397. Last accessed October 9, 2024.
237. Office of Diversion Control. Drug Disposal Information. Available at https://www.deadiversion.usdoj.gov/drug_disposal/. Last accessed October 9, 2024.
238. Goudas LC, Bloch R, Gialeli-Goudas M, Lau J, Carr DB. The epidemiology of cancer pain. Cancer Invest. 2005;23:182-190.
239. Jensen MP, Karoly P. Self-report scales and procedures for assessing pain in adults. In: Turk DC, Melzack R (eds.). Handbook of Pain Assessment. New York, NY: The Guilford Press; 2011: 19-44.
241. Desbiens NA, Mueller-Rizner N. How well do surrogates assess the pain of seriously ill patients? Crit Care Med. 2000;28(5):1347-1352.
242. Portenoy RK, Hagen NA. Breakthrough pain: definition, prevalence and characteristics. Pain. 1990;41:273-281.
243. Hockenberry M, Wilson D. Wong's Essentials of Pediatric Nursing. 9th ed. St. Louis, MO: Mosby; 2013.
244. Fishman B, Pasteranak S, Wallenstien SL, Houde RW, Holland JC, Foley KM. The Memorial Pain Assessment Card: a valid instrument for the evaluation of cancer pain. Cancer. 1987;60:1151-1158.
245. 245. WHO Guidelines for the Pharmacological and Radiotherapeutic management of Cancer Pain in Adults and Adolescents. Geneva: World Health Organization; 2018.
246. Scottish Partnership for Palliative Care. Scottish Palliative Care Guidelines. Available at https://www.palliativecareguidelines.scot.nhs.uk. Last accessed October 9, 2024.
247. U.S. Food and Drug Administration. Drug Approvals and Databases. Available at https://www.fda.gov/drugs/development-approval-process-drugs/drug-approvals-and-databases. Last accessed October 9, 2024.
249. Argoff CE, Silvershein DI. A comparison of long- and short-acting opioids for the treatment of chronic noncancer pain: tailoring therapy to meet patient needs. Mayo Clin Proc. 2009;84(7):602-612.
250. Pergolizzi JV Jr, Mercadante S, Echaburu AV, et al. The role of transdermal buprenorphine in the treatment of cancer pain: an expert panel consensus. Curr Med Res Opin. 2009;25(6):1517-1528.
251. Lauretti GR, Oliveira GM, Pereira NL. Comparison of sustained-release morphine with sustained-release oxycodone in advanced cancer patients. Br J Cancer. 2003;89:2027-2030.
252. Lexicomp Online. Available at https://online.lexi.com. Last accessed October 9, 2024.
253. McCleane G, Smith HS. Opioids for persistent noncancer pain. Anesthesiol Clin. 2007;25:787-807.
254. Shaiova L, Berger A, Blinderman CD, et al. Consensus guideline on parenteral methadone use in pain and palliative care. Palliat Support Care. 2008;6(2):165-176.
255. Nicholson AB, Watson GR, Derry S, Wiffen PJ. Methadone for cancer pain. Cochrane Database Syst Rev. 2017;(2):CD003971.
256. Dart RC, Woody GE, Kleber HD. Prescribing methadone as an analgesic [letter]. Ann Intern Med. 2005;143:620.
257. Drugs.com FDA Approves Nucynta ER (Tapentadol) Extended-Release Oral Tablets for the Management of Neuropathic Pain Associated with Diabetic Peripheral Neuropathy. Available at https://www.drugs.com/newdrugs/fda-approves-nucynta-er-tapentadol-extended-release-oral-management-neuropathic-pain-associated-3461.html. Last accessed October 9, 2024.
258. Vadivelu N, Timchenko A, Huang Y, Sinatra R. Tapentadol extended-release for treatment of chronic pain: a review. J Pain Res. 2011;4:211-218.
259. Schikowski A, Krings D, Schwenke K. Tapentadol prolonged release for severe chronic cancer-related pain: effectiveness, tolerability, and influence on quality of life of the patients. J Pain Res. 2014;8:1-8.
260. Blick SK, Wagstaff AJ. Fentanyl buccal tablet: in breakthrough pain in opioid-tolerant patients with cancer. Drugs. 2006;66(18):2387-2395.
263. Fallon MT, Laird BJA. A systematic review of combination step III opioid therapy in cancer pain: an EPCRC opioid guideline project. Palliat Med. 2011;25(5):597-603.
264. Saarto T, Wiffen PJ. Antidepressants for neuropathic pain. Cochrane Database Syst Rev. 2007;(4):CD005454.
265. Dolinsky C, Metz JM. Palliative radiation therapy in oncology. Anesthesiol Clin North Am. 2006;24:113-128.
266. Fine PG. Palliative radiation therapy in end-of-life care: evidence-based utilization. Am J Hospice Palliat Med. 2002;19(3):166-170.
267. Berrang T, Samant R. Palliative radiotherapy knowledge among community family physicians and nurses. J Cancer Educ. 2008;23(3):156-160.
268. Tilden VP, Drach LL, Tolle SW. Complementary and alternative therapy use at end-of-life in community settings. J Altern Complement Med. 2004;10(5):811-817.
269. Demmer C. A survey of complementary therapy services provided by hospices. J Palliat Med. 2004;7(4):510-516.
270. Kozak LE, Kayes L, McCarty R, et al. Use of complementary and alternative medicine (CAM) by Washington State hospices. Am J Hosp Palliat Care. 2008;25(6):463-468.
271. Dain AS, Bradley EH, Hurzeler R, Aldridge MD. Massage, music, and art therapy in hospice: results of a national survey. J Pain Symptom Manage. 2015;49(6):1035-1041.
272. Olotu BS, Brown CM, Lawson KA, Barner JC. Complementary and alternative medicine utilization in Texas hospices: prevalence, importance, and challenges. Am J Hosp Palliat Care. 2014;31(3):254-259.
273. Polubinski JP, West L. Implementation of a massage therapy program in the home hospice setting. J Pain Symptom Manage. 2005;30:104-106.
274. Choi TY, Lee MS, Kim TH, Zaslawski C, Ernst E. Acupuncture for the treatment of cancer pain: a systematic review of randomised clinical trials. Support Care Cancer. 2012;20(6):1147-1158.
275. Raub JA. Psychophysiologic effects of hatha yoga on musculoskeletal and cardiopulmonary function: a literature review. J Altern Complement Med. 2002;8:797-812.
277. Reynolds MW, Nabors L, Quinlan A. The effectiveness of art therapy: does it work? J Am Art Ther Assoc. 2000;17:207-213.
278. National Comprehensive Cancer Network. Cancer-Related Fatigue. V 1.2021. Available at https://www.nccn.org/professionals/physician_gls/pdf/fatigue.pdf. Last accessed October 9, 2024.
279. Radbruch L, Strasser F, Elsner F, et al. Fatigue in palliative care patients: an EAPC approach. Palliat Med. 2008;22(1):13-32.
280. Passik SD, Kirsh KL, Donaghy K et al. Patient-related barriers to fatigue communication: initial validation of the fatigue management barriers questionnaire. J Pain Symptom Manage. 2002;24: 481-493.
281. Agency for Healthcare Research and Quality. Management of Cancer Symptoms: Pain, Depression, and Fatigue. Evidence Report/Technology Assessment No. 61. Rockville, MD: U.S. Department of Health and Human Services; 2002.
282. Fleishman SB. Treatment of symptom clusters: pain, depression, and fatigue. J Natl Cancer Inst Monogr. 2004;(32):119-23.
283. Barsevick A. The elusive concept of the symptom cluster. Oncol Nurse Forum. 2007;34(5):971-980.
284. Bower JE, Bak K, Berger A, et al. Screening, assessment, and management of fatigue in adult survivors of cancer: an American Society of Clinical oncology clinical practice guideline adaptation. J Clin Oncol. 2014;32(17):1840-1850.
285. Walsh D, Rybicki L. Symptom clustering in advanced cancer. Support Care Cancer. 2006;14(8):831-836.
286. Ross D, Alexander CS. Management of common symptoms in terminally ill patients: part I. Fatigue, anorexia, cachexia, nausea and vomiting. Am Fam Physician. 2001;64:807-814.
287. Harris J. Fatigue in chronically ill patients. Curr Opin Support Palliat Care. 2008;2(3):180-186.
288. Curt G, Breitbart W, Cella D, et al. Impact of cancer-related fatigue on the lives of patients: new findings from the Fatigue Coalition. Oncologist. 2000;5(5):353-360.
289. Mendoza T, Wang XS, Cleeland CS, et al. The rapid assessment of fatigue severity in cancer patients: use of the Brief Fatigue Inventory. Cancer. 1999;85:1186-1196.
290. Minton O, Stone P, Richardson A, Sharpe M, Hotopf M. Drug therapy for the management of cancer related fatigue. Cochrane Database Syst Rev. 2008;(1):CD006704.
291. Minton O, Richardson A, Sharpe M, Hotopf M, Stone P. Drug therapy for the management of cancer-related fatigue. Cochrane Database Syst Rev. 2010;(7):CD006704.
292. Mochamat MM, Cuhls H, Peuckmann-Post V, Minton O, Stone P, Radbruch L. Pharmacological treatments for fatigue associated with palliative care. Cochrane Database Syst Rev. 2015;(5):CD006788.
293. Cramp F, Daniel J. Exercise for the management of cancer-related fatigue in adults. Cochrane Database of Syst Rev. 2008;(2):CD006145.
294. Volberding PA, Levine AM, Dieterich D, et al. Anemia in HIV infection: clinical impact and evidence-based management strategies. Clin Infect Dis. 2004;38:1454-1463.
295. Schmidt RJ, Dalton CL. Treating anemia of chronic kidney disease in the primary care setting: cardiovascular outcomes and management recommendations. Osteopath Med Primary Care. 2007;1:14.
296. Ngo K, Kotecha D, Walters JA, et al. Erythropoiesis-stimulating agents for anaemia in chronic heart failure patients. Cochrane Database Syst Rev. 2010;(1):CD007613.
297. U.S. Food and Drug Administration. FDA Drug Safety Communication: Modified Dosing Recommendations to Improve the Safe Use of Erythropoiesis-Stimulating Agents (ESAs) in Chronic Kidney Disease. Available at https://www.fda.gov/drugs/drug-safety-and-availability/fda-drug-safety-communication-modified-dosing-recommendations-improve-safe-use-erythropoiesis. Last accessed October 9, 2024.
298. National Kidney Foundation, Kidney Disease Outcomes Quality Initiative. KDOQI clinical practice guideline and clinical practice recommendations for anemia in chronic kidney disease: 2007 update of hemoglobin target. Am J Kidney Dis. 2007;50(3):471-530.
299. Rizzo JD, Brouwers M, Hurley P, et al. American Society of Clinical Oncology/American Society of Hematology clinical practice guideline update on the use of epoetin and darbepoetin in adult patients with cancer. J Clin Oncol. 2010;28(33):4996-5010.
300. Cramp F, Byron-Daniel J. Exercise for the management of cancer-related fatigue in adults. Cochrane Database Syst Rev. 2012;(11):CD006145.
301. Porock K, Kristjanson LJ, Tinnelly K, et al. An exercise intervention for advanced cancer patients experiencing fatigue: a pilot study. J Palliat Care. 2000;16:30-36.
302. Segal R, Reid RD, Courneya KS, et al. Resistance exercise in men receiving androgen deprivation therapy for prostate cancer. J Clin Oncol. 2003;21:1653-1659.
303. Oldervoll L, Loge JH, Paltiel H, et al. The effect of a physical exercise program in palliative care: a phase II study. J Pain Symptom Manage. 2006;31:421-430.
304. Rabkin JG, McElihiney MC, Rabkin R, McGrath PJ. Modafinil treatment for fatigue in HIV/AIDS: a randomized placebo-controlled study. J Clin Psychiatry. 2010;71(6):707-715.
305. Stone PC. Methylphenidate in the management of cancer-related fatigue. Clin Oncol. 2013;31(19):2372-2373.
306. Bausewein C, Farquhar M, Booth S, Gysels M, Higginson IJ. Measurement of breathlessness in advanced disease: a systematic review. Respir Med. 2007;101(3):399-410.
307. Edmonds P, Karlsen S, Khan S, Addington-Hall J. A comparison of the palliative care needs of patients dying from chronic respiratory diseases and lung cancer. Palliat Med. 2001;15(4):287-295.
309. Marciniuk DD, Goodridge D, Hernandez P, et al. Managing dyspnea in patients with advanced chronic obstructive pulmonary disease: a Canadian Thoracic Society clinical practice guideline. Can Respir J. 2011;18(2):69-78.
310. National Comprehensive Cancer Network. NCCN Clinical Practice Guidelines in Oncology: Palliative Care. Version 1.2024. Available at https://www.nccn.org/professionals/physician_gls/pdf/palliative.pdf. Last accessed October 4, 2024.
311. Bausewein C, Booth S, Gysels M, Higginson I. Non-pharmacological interventions for breathlessness in advanced stages of malignant and non-malignant diseases. Cochrane Database Syst Rev. 2008;(2):CD005623.
312. Kidney International Supplements. KDIGO clinical practice guideline for anemia in chronic kidney disease. J Internat Soc Nephrol. 2012;2(4):1-64.
313. Galbraith S, Fagan P, Perkins P, Lynch A, Booth S. Does the use of a handheld fan improve chronic dyspnea? A randomized, controlled, crossover trial. J Pain Symptom Manage. 2010;39(5):831-838.
314. Bailey CD, Wagland R, Dabbour R, Caress A, Smith J, Molassiotis A. An integrative review of systematic reviews related to the management of breathlessness in respiratory illnesses. BMC Pulm Med. 2010;10:63.
315. Jennings AL, Davies AN, Higgins JP, et al. A systematic review of the use of opioids in the management of dyspnoea. Thorax. 2002;57:939-944.
316. Clemens KE, Klaschik E. Effect of hydromorphone on ventilation in palliative care patients with dyspnea. Support Care Cancer. 2008;16(1):93-99.
317. Simon ST, Higginson IJ, Booth S, H arding R, Bausewein C. Benzodiazepines for the relief of breathlessness in advanced malignant and non-malignant diseases in adults. Cochrane Database Syst Rev. 2010;(1):CD007354.
318. Bausewein C, Booth S, Gysels M, Higginson IJ. WITHDRAWN: Non-pharmacological interventions for breathlessness in advanced stages of malignant and non-malignant diseases. Cochrane Database Syst Rev. 2013;(11):CD005623.
319. Larkin PJ, Sykes NP, Centeno C, et al. The management of constipation in palliative care: clinical practice recommendations. Palliat Med. 2008;22(7):796-807.
320. Librach SL, Bouvette M, De Angelis C, et al. Consensus recommendations for the management of constipation in patients with advanced, progressive illness. J Pain Symptom Manage. 2010;40(5):761-773.
321. World Health Organization. Essential Medicines in Palliative Care. Available at https://www.who.int/selection_medicines/committees/expert/19/applications/PalliativeCare_8_A_R.pdf. Last accessed October 9, 2024.
322. Miles C, Fellowes, D, Goodman ML, Wilkinson S. Laxatives for the management of constipation in palliative care patients. Cochrane Database Syst Rev. 2006;(4):CD003448.
323. American College of Gastroenterology Chronic Constipation Task Force. An evidence-based approach to the management of chronic constipation in North America. Am J Gastroenterol. 2005;100:S1-S22.
324. Candy B, Jones L, Goodman ML, Drake R, Tookman A. Laxatives or methylnaltrexone for the management of constipation in palliative care patients. Cochrane Database System Rev. 2011;(1):CD003448.
325. Hawley PH, Byeon JJ. A comparison of sennosides-based bowel protocols with and without docusate in hospitalized patients with cancer. J Palliat Med. 2008;11(4):575-581.
326. U.S. Food and Drug Administration. Drugs@FDA: FDA-Approved Drugs. Available at https://www.accessdata.fda.gov/scripts/cder/daf/index.cfm. Last accessed October 9, 2024.
327. U.S. Food and Drug Administration. FDA Approves Movantik for Opioid-Induced Constipation. Available at https://wayback.archive-it.org/7993/20170112023822/http://www.fda.gov/NewsEvents/Newsroom/PressAnnouncements/ucm414620.htm. Last accessed October 9, 2024.
328. Wood GJ, Shega JW, Lynch B, Von Roenn JH. Management of intractable nausea and vomiting in patients at the end of life. JAMA. 2007;298(10):1196-1207.
329. Glare P, Miller J, Nikolova T, Tickoo R. Treating nausea and vomiting in palliative care: a review. Clin Intervent Aging. 2011;6:243-259.
330. Hesketh PJ, Kris MG, Basch E, et al. Antiemetics: ASCO guideline update. J Clin Oncol. 2020;38(24):2782-2797.
331. Wickham RJ. Nausea and vomiting not related to cancer therapy: intractable problem or clinical challenge? J Adv Pract Oncol. 2020;11(5):476-488.
332. Davis MP, Hallerberg G, Palliative Medicine Study Group of the Multinational Association of Supportive Care in Cancer. A systematic review of the treatment of nausea and/or vomiting in cancer unrelated to chemotherapy or radiation. J Pain Symptom Manage. 2010;39(4):756-767.
333. Glare P, Pereira G, Kristjanson LJ, Stockler M, Tattersall M. Systematic review of the efficacy of antiemetics in the treatment of nausea in patients with far-advanced cancer. Support Care Cancer. 2004;12(6):432-440.
334. Glare P, Dunwoodie D, Clark K, et al. Treatment of nausea and vomiting in terminally ill cancer patients. Drugs. 2008;68(18):2575-2590.
335. U.S. Food and Drug Administration. FDA Drug Safety Communication: Abnormal Heart Rhythms May be Associated with Use of Zofran (Ondansetron). Available at https://www.fda.gov/drugs/drug-safety-and-availability/fda-drug-safety-communication-abnormal-heart-rhythms-may-be-associated-use-zofran-ondansetron. Last accessed October 9, 2024.
336. U.S. Food and Drug Administration. FDA Drug Safety Communication: New Information Regarding QT Prolongation with Ondansetron (Zofran). Available at https://www.fda.gov/drugs/drug-safety-and-availability/fda-drug-safety-communication-new-information-regarding-qt-prolongation-ondansetron-zofran. Last accessed October 9, 2024.
338. Donohoe CL, Ryan AM, Reynolds JV. Cancer cachexia: mechanisms and clinical implications. Gastroenterol Res Pract. 2011:601434.
339. Evans WJ, Morley JE, Argiles J, et al. Cachexia: a new definition. Clin Nutr. 2008;27(6):793-799.
340. Mangili A, Murman DH, Zampini AM, Wanke CA, Mayer KH. Nutrition and HIV infection: review of weight loss and wasting in the era of highly active antiretroviral therapy from the Nutrition for Healthy Living Cohort. Clin Infect Dis. 2006;42(6):836-842.
341. von Haehling S, Anker SD. Cachexia as a major underestimated and unmet medical need: facts and numbers. J Cachexia Sarcopenia Muscle. 2010;1:1-5.
342. Fearon K, Strasser F, Anker SD, et al. Definition and classification of cancer cachexia: an international consensus. Lancet Oncol. 2011;12(5):489-495.
343. Springer J, Filippatos G, Akashi YJ, Anker SD. Prognosis and therapy approaches of cardiac cachexia. Curr Opin Cardiol. 2006;21(3):229-233.
344. Consensus Development Panel Meeting. Treatment Guidelines for HIV-Associated Wasting. New York, NY: 2000.
345. Lasheen W, Walsh D. The cancer anorexia-cachexia syndrome: myth or reality? Support Care Cancer. 2010;18(2):265-272.
346. Yavuzsen T, Walsh D, Davis MP, et al. Components of the anorexia-cachexia syndrome: gastrointestinal symptom correlates of cancer anorexia. Support Care Cancer. 2009;17(12):1531-1541.
347. Kalantar-Zadeh K, Anker SD, Horwich TB, Fonarow GC. Nutritional and anti-inflammatory interventions in chronic heart failure. Am J Cardiol. 2008;101(11A):89E-103E.
348. Polsky B, Kotler D, Steinhart C. Treatment guidelines for HIV-associated wasting. HIV Clin Trials. 2004;5(1):50-61.
349. Sarhill N, Mahmoud F. Hiccups and other gastrointestinal symptoms. In: Berger AM, Shuster JL, Von Roenn JH (eds). Principles and Practice of Palliative Care and Supportive Oncology. 4th ed. Philadelphia, PA: Lippincott Williams & Wilkins; 2013: 223-237.
350. Bosaeus I. Nutritional support in multimodal therapy for cancer cachexia. Support Care Cancer. 2008;16(5):447-451.
351. Garcia VR, Lopez-Briz E, Sanchis RC, Perales JLG, Bort-Marti S. Megestrol acetate for treatment of anorexia-cachexia syndrome. Cochrane Database Syst Rev. 2013;(3):CD004310.
352. Moyle GJ, Schoelles K, Fahrback K, et al. Efficacy of selected treatments of HIV wasting: a systematic review and meta-analysis. J Acquir Immune Defic Syndr. 2004;37(Suppl 5):S262-S276.
353. Gelato M, McNurlan M, Freedland E. Role of recombinant human growth hormone in HIV-associated wasting and cachexia: pathophysiology and rationale for treatment. Clin Ther. 2007;29(11):2269-2288.
354. Gullett NP, Hebbar G, Ziegler TR. Update on clinical trials of growth factors and anabolic steroids in cachexia and wasting. Am J Clin Nutr. 2010;91(4):1143S-1147S.
355. Grunfeld C, Kotler DP, Dobs A, Glesby M, Bhasin S. Oxandrolone in the treatment of HIV-associated weight loss in men: a randomized, double-blind, placebo-controlled study. J Acquir Immune Defic Syndr. 2006;41(3):304-314.
356. Yeh SS, DeGuzman B, Kramer T, M012 Study Group. Reversal of COPD-associated weight loss using the anabolic agent oxandrolone. Chest. 2002;122(2):421-428.
357. Orr R, Fiatarone Singh M. The anabolic androgenic steroid oxandrolone in the treatment of wasting and catabolic disorders: review of efficacy and safety. Drugs. 2004;64(7):725-750.
358. DeBoer MD. Emergence of ghrelin as a treatment for cachexia syndromes. Nutrition. 2008;24(9):806-814.
359. Khatib MN, Shankar AH, Kirubakaran, et al. Ghrelin for the management of cachexia associated with cancer. Cochrane Database Syst Rev. 2018;(2):CD012229.
360. Beckwith MC. Diarrhea in palliative care patients. In: Lipman AG, Jackson KC II, Tyler LS (eds). Evidence-Based Symptom Control in Palliative Care: Systematic Reviews and Validated Clinical Practice Guidelines for 15 Common Problems in Patients with Life-Limiting Disease. Binghamton, NY: Haworth Press; 2000: 99-101.
361. Alderman J. Fast Facts and Concepts #96: Diarrhea in Palliative Care, 2nd edition. Available at https://www.mypcnow.org/fast-fact/diarrhea-in-palliative-care/. Last accessed October 9, 2024.
362. American Gastroenterological Association. American Gastroenterological Association medical position statement: guidelines for the evaluation and management of chronic diarrhea. Gastroenterology. 1999;116:1461-1463.
363. Allen SJ, Martinez EG, Gregorio GV, Dans LF. Probiotics for treating acute infectious diarrhea. Cochrane Database Syst Rev. 2010;(11):CD003048.
364. Collinson S, Deans A, Padua-Zamora, et al. Probiotics for treating acute infectious diarrhoea. Cochrane Database Syst Rev. 2020;(12):CD003048.
365. Schutte-Rodin S, Broch L, Buysse D, Dorsey C, Sateia M. Clinical guideline for the evaluation and management of chronic insomnia in adults. J Clin Sleep Med. 2008;4(5):487-504.
367. Hugel H, Ellershaw JE, Cook L, Skinner J, Irvine C. The prevalence, key causes and management of insomnia in palliative care patients. J Pain Symptom Manage. 2004;27(4):316-321.
368. Shayamsunder AK, Patel SS, Jain V, Peterson RA, Kimmel PL. Sleepiness, sleeplessness, and pain in end-stage renal disease: distressing symptoms for patients. Semin Dial. 2005;18:109-118.
370. Savard J, Marin CM. Insomnia in the context of cancer: a review of a neglected problem. J Clin Oncol. 2001;19:895-908.
371. Johns MW. A new method for measuring daytime sleepiness: the Epworth sleepiness scale. Sleep. 1991;14:54-545.
372. Edinger JD, Arnedt JT, Bertisch SM, et al. Behavioral and psychological treatments for chronic insomnia disorder in adults: an American Academy of Sleep Medicine clinical practice guideline. J Clin Sleep Med. 2021;17(2):255-262.
374. Matsuo N, Morita T. Efficacy, safety, and cost effectiveness of intravenous midazolam and flunitrazepam for primary insomnia in terminally ill patients with cancer: a retrospective multicenter audit study. J Palliat Med. 2007;10:1054-1062.
375. Bennett T, Bray D, Neville MW. Suvorexant, a dual orexin receptor antagonist for the management of insomnia. P T. 2014;39(4):264-266.
376. Scholz H, Trenkwalder C, Kohnen R, Riemann D, Kriston L, Hornyak M. Dopamine agonists for restless legs syndrome. Cochrane Database Syst Rev. 2011;(3):CD006009.
377. Barton DL, Atherton PJ, Bauer BA, et al. The use of Valeriana officinalis (valerian) in improving sleep in patients who are undergoing treatment for cancer: a phase III randomized, placebo-controlled, double-blind study (NCCTG Trial, N01C5). J Support Oncol. 2011;9(1):24-31.
378. American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders. 5th ed. Text revision. Washington, DC: American Psychiatric Association; 2022.
379. Friedlander M, Brayman Y, Breitbart WS. Delirium in palliative care. Oncology (Williston Park). 2004;18(12):1541-1550.
381. Rudolph JL, Marcantonio ER. Diagnosis and prevention of delirium. Geriat Aging. 2003;6(10):14-19.
382. Grassi L, Caraceni A, Mitchell AJ, et al. Management of delirium in palliative care: a review. Curr Psychiatry Rep. 2015;17(3):550.
384. Casarett D, Inouye S. Diagnosis and management of delirium near the end of life. Ann Intern Med. 2001;135:32-40.
385. Leonard M, Agar M, Mason C, Lawlor P. Delirium issues in palliative care settings. J Psychosom Res. 2008;65(3):289-298.
386. Cobb JL, Glantz MJ, Martin WE, et al. Delirium in patients with cancer at the end of life. Cancer Pract. 2000;8:172-177.
387. Lawlor PG, Fainsinger RL, Bruera ED. Delirium at the end of life: critical issues in clinical practice and research. JAMA. 2000;284:2427-2429.
388. Jackson KC, Lipman AG. Drug therapy for delirium in terminally ill adult patients. Cochrane Database System Rev. 2004;(2):CD004770.
389. Boettger S, Breitbart W. Atypical antipsychotics in the management of delirium: a review of the empirical literature. Palliat Support Care. 2005;3(3):227-237.
390. Lonergan E, Britton AM, Luxenberg J, Wyller T. Antipsychotics for delirium. Cochrane Database Syst Rev. 2007;(2):CD005594.
391. Finucane AM, Jones L, Leurent B, et al. Drug therapy for delirium in terminally ill adults. Cochrane Database Syst Rev. 2020;(1):CD004770.
392. Straker DA, Shapiro PA, Muskin PR. Aripiprazole in the treatment of delirium. Psychosomatics. 2006;47(5):385-391.
393. Boettger S, Breitbart W. An open trial of aripiprazole for the treatment of delirium in hospitalized cancer patients. Palliat Support Care. 2011;9(4):351-357.
394. Noorani NH, Montagnini M. Recognizing depression in palliative care patients. J Palliat Med. 2007;10(2):458-464.
395. von Roenn JH, Paice JA. Control of common, non-pain cancer symptoms. Semin Oncol. 2005;32:200-210.
396. National Comprehensive Cancer Network. NCCN Clinical Practice Guidelines in Oncology: Distress Management. Available at https://www.nccn.org/professionals/physician_gls/pdf/distress.pdf. Last accessed October 9, 2024.
397. Chochinov HM, Hack T, Hassard T, Kristjanson LJ, McClement S, Harlos M. Understanding the will to live in patients nearing death. Psychosomatics. 2005;46:7-10.
398. Breitbart W, Rosenbeld B, Pessin H, et al. Depression, hopelessness, and desire for hastened death in terminally ill patients with cancer. JAMA. 2000;284:2907-2911.
399. Emanuel EJ, Fairclough DL, Emanuel LL. Attitudes and desires related to euthanasia and physician-assisted suicide among terminally ill patients and their caregivers. JAMA. 2000;284:2460-2468.
400. Mystakidou K, Rosenfeld B, Parpa E, et al. Desire for death near the end of life: the role of depression, anxiety and pain. Gen Hosp Psychiatry. 2005;27(4):258-262.
401. Dees MK, Vernooij-Dassen MJ, Dekkers WJ, et al. "Unbearable suffering:" a qualitative study on the perspectives of patients who request assistance in dying. J Med Ethics. 2011;37:727-723.
402. Hudson P, Kristianson L, Ashby M, et al. Desire for hastened death in patients with advanced disease and the evidence base of clinical guidelines: a systematic review. Palliat Med. 2006;20(7):693-701.
403. Suarez-Almazor M, Newman C, Hanson J, et al. Attitudes of terminally ill cancer patients about euthanasia and assisted suicide: predominance of psychosocial determinants and beliefs over symptom distress and subsequent survival. J Clin Oncol. 2002;20(8):2134-2141.
404. Lee D, Schroeder JR, Karschner EL, et al. Cannabis withdrawal in chronic, frequent cannabis smokers during sustained abstinence within a closed residential environment. Am J Addict. 2014;23(3):234-242.
406. Stoklosa J, Patterson K, Rosielle D, Arnold RM. Anxiety in palliative care: causes and diagnosis. J Palliat Med. 2011;14(10):1173-1174.
407. Roth A, Massie M. Anxiety in palliative care. In: Chochinov M, Breitbart W (eds). Handbook of Psychiatry in Palliative Medicine. 2nd ed. New York, NY: Oxford University Press; 2009: 69-80.
408. Gibson C, Lichtenthal W, Berg A, Breitbart W. Psychologic issues in palliative care. Anesthesiol Clin North Am. 2006;24:61-80.
409. Longo L, Johnson B. Addiction: Part 1. Benzodiazepines: side effects, abuse risk and alternatives. Am Fam Physician. 2000;61(7):2121-2128.
410. National Cancer Institute. Depression (PDQ) – Health Professional Version. Available at https://www.cancer.gov/about-cancer/coping/feelings/depression-hp-pdq. Last accessed October 9, 2024.
411. McClain C, Rosenfeld B, Breitbart W. Effect of spiritual well-being on end-of-life despair in terminally ill cancer patients. Lancet. 2003;361(9369):1603-1607.
412. Bekelman DB, Hutt E, Masoudi FA, Kutner JS, Rumsfeld JS. Defining the role of palliative care in older adults with heart failure. Int J Cardiol. 2008;125(2):183-190.
413. Lang C, Mancini D. Non-cardiac comorbidities in chronic heart failure. Heart. 2007;93(6):665-671.
414. Lloyd-Williams M, Spiller J, Ward J. Which depression screening tools should be used in palliative care? Palliat Med. 2003;17(1): 40-43.
415. Chochinov HM, Wilson KG. "Are you depressed?" Screening for depression in the terminally ill. Am J Psychiatry. 1997;154:674-676.
416. Huffman J, Stern T. Using psychostimulants to treat depression in the medically ill. Prim Care Companion J Clin Psychiatry. 2004;6(1):44-46.
417. Daaleman T, Usher BM, Williams SW, Rawlings J, Hanson LC. An exploratory study of spiritual care at the end of life. Am Fam Med. 2008;6:406-411.
418. Sinclair S, Pereira J, Raffin S. A thematic review of the spirituality literature within palliative care. J Palliat Med. 2006;9(2):464-479.
419. Puchalski C, Ferrell B, Virani R, et al. Improving the quality of spiritual care as a dimension of palliative care: the report of the consensus conference. J Palliat Med. 2009;12(10):885-904.
420. Breitbart W, Gibson C, Poppito SR, Berg A. Psychotherapeutic interventions at the end of life: a focus on meaning and spirituality. Can J Psychiatry. 2004;49:366-372.
422. Johnson KS, Tulsky JA, Hays JC, et al. Which domains of spirituality are associated with anxiety and depression in patients with advanced illness? J Gen Intern Med. 2011;26(7):751-758.
423. Murray SA, Kendall M, Boyd K, Worth A, Benton TF. Exploring the spiritual needs of people dying of lung cancer or heart failure: a prospective qualitative interview study of patients and their carers. Palliat Med. 2004;18:39-45.
425. Smolinski K, Colon Y. Silent voices and invisible walls: exploring end of life care with lesbians and gay men. J Psychosoc Oncol. 2006;24(1):51-64.
427. Pennachio D. Cultural competence: caring for Chinese, Japanese, and Korean patients. Med Econ. 2004;81:54.
428. Dayer-Berenson, L. Native Americans: traditional health beliefs. In: Cultural Competencies for Nurses. Impact on Health and Illness. Sudbury, MA: Jones and Bartlett Publishers, LLC; 2011: 252-255.
429. Ackroyd R. Audit of referrals to a hospital palliative care team: role of the bilingual health-care worker. Int J Palliat Nurs. 2003;9(8):352-357.
430. National Cancer Institute. Last Days of Life – Health Professional Version. Available at https://www.cancer.gov/about-cancer/advanced-cancer/caregivers/planning/last-days-hp-pdq. Last accessed October 9, 2024.
431. Manfredonia J. Prescribing methadone for pain management in end-of-life care. JAOA. 2005;105(3 Suppl):18S-21S.
432. Lokker ME, van Zuylen L, van der Rijt CC, et al. Prevalence, impact, and treatment of death rattle: a systematic review. J Pain Symptom Manage. 2014;47(1):105-122.
433. Wee B, Hillier R. Interventions for noisy breathing in patients near to death. Cochrane Database Syst Rev. 2008;(1):CD005177.
434. Elsayem A, Curry E III, Boohene J, et al. Use of palliative sedation for intractable symptoms in the palliative care unit of a comprehensive cancer center. Support Care Cancer. 2009;17(1):53-59.
435. Rietjens JA, van Zuylen L, van Veluw H, van der Wijk L, van der Heide A, van der Rijt CC. Palliative sedation in a specialized unit for acute palliative care in a cancer hospital: comparing patients dying with and without palliative sedation. J Pain Symptom Manage. 2008;36(3):228-234.
437. Kirk T, Mahon M. National Hospice and Palliative Care Organization (NHPCO) position statement and commentary on the use of palliative sedation in imminently dying terminally ill patients. J Pain Symptom Manage. 2010;39(5):914-923.
438. American Medical Association. Ethics: Physician-Assisted Suicide. Available at https://www.ama-assn.org/delivering-care/ethics/physician-assisted-suicide. Last accessed October 9, 2024.
439. American Academy of Hospice and Palliative Medicine. Statement on Physician-Assisted Dying. Available at http://aahpm.org/positions/pad. Last accessed October 9, 2024.
440. National Hospice and Palliative Care Organization. Commentary and Resolution on Physician-Assisted Suicide. Available at www.nationalhospiceanalytics.com/library/documents/PAS_resources/NHPCO_PAS_Resolution_Commentary.pdf. Last accessed October 9, 2024.
441. Lampert R, Hayes DL, Annas GJ, et al. HRS expert consensus statement on the management of cardiovascular implantable electronic devices (CIEDs) in patients nearing end of life or requesting withdrawal of therapy. Heart Rhythm. 2010;7(7):1008-1026.
442. Stroebe MS, Hansson RO, Schut H, et al. (eds). Handbook of Bereavement Research and Practice: Advances in Theory and Intervention. Washington, DC: American Psychological Association; 2008.
444. Main J. Improving management of bereavement in general practice based on a survey of recently bereaved subjects in a single general practice. Br J Gen Pract. 2000;50:863-866.
445. Bedell S, Cadenhead K, Braboys T. The doctor's letter of condolence: national vital statistics reports final data 1998. N Engl J Med. 2001;344:1161-1162.
446. Casarett D, Karlawish J, Morales K, Crowley R, Mirsch T, Asch DA. Improving the use of hospice services in nursing homes: a randomized controlled trial. JAMA. 2005;294:211-217.
447. Miller SC, Lima J, Gozalo PL, MOR V. The growth of hospice care in U.S. nursing homes. J Am Geriatr Soc. 2010;581:1481-1488.
448. Powers BA, Watson NM. Meaning and practice of palliative care for nursing home residents with dementia at end of life. Am J Alzheimers Dis Other Demen. 2008;23(4):319-325.
449. Brazil K, Vohra JU. Identifying educational needs in end-of-life care for staff and families of residents in care facilities. Int J Palliat Nurs. 2005;11(9):475-480.
450. Jones KR, Fink R, Pepper G, et al. Improving nursing home staff knowledge and attitudes about pain. Gerontologist. 2004;44:469-478.
451. Kiely D, Prigerson H, Mitchell SL. Health care proxy grief symptoms before the death of nursing home residents with advanced dementia. Am J Geriatr Psychiatry. 2008;16(8):664-673.
452. Masoudi FA, Krumholz HM. Polypharmacy and comorbidity in heart failure. BMJ. 2003;327(7414):513-514.
453. Havranek E, Masoudi FA, Westfall KA, Wolfe P, Ordin DL, Krumholz HM. Spectrum of heart failure in older patients: results from the National Heart Failure project. Am Heart J. 2002;143(3):412-417.
454. Holmes HM, Sachs GA, Shega JW, Hougham GW, Cox Hayley D, Dale W. Integrating palliative medicine into the care of persons with advanced dementia: identifying appropriate medication use. J Am Geriatr Soc. 2008;56(7):1306-1311.
455. Stevenson J, Abernethy AP, Miller C, Currow DC. Managing comorbidities in patients at the end of life. BMJ. 2004;329(7471):909-912.
456. Helme RD, Gibson SJ. The epidemiology of pain in elderly people. Clin Geriatr Med. 2001;17:417-431.
457. Ferrell BA, Ferrell BR, Rivera L. Pain in cognitively impaired nursing home patients. J Pain Sympt Manage. 1995;10:591-598.
458. American Geriatrics Society Panel on Pharmacological Management of Persistent Pain in Older Persons. Pharmacological management of persistent pain in older persons. J Am Geriatr Soc. 2009;57:1331-1346.
459. Mitchell SL, Teno JM, Kiely DK, et al. The clinical course of advanced dementia. N Engl J Med. 2009;361:1529-1538.
460. Hanson LC, Eckert KJ, Dobbs D, et al. Symptom experience of dying long-term care residents. J Am Geriatr Soc. 2008;56:91-98.
461. Teno JM, Clarridge BR, Casey V, et al. Family perspectives on end-of-life care at the last place of care. JAMA. 2004;291:88-93.
463. Vandenberg EV, Tvrdik A, Keller BK. Use of the quality improvement process in assessing end-of-life care in the nursing home . J Am Med Dir Assoc. 2005;6(5):334-339.
464. Mahon MM, Sorrell JM. Palliative care for people with Alzheimer's disease. Nurs Philos. 2008;9(2):110-120.
465. Miller SC, Lima J, Gozalo PL, Mor V. The growth of hospice care in U.S. nursing homes. J Am Geriatr Soc. 2010;58(8):1481-1488.
466. Aminoff BZ. Dying dementia patients: too much suffering, too little palliation. Am J Hosp Palliat Care. 2005;22(5):344-348.
467. Herr K, Coyne PJ, Ely E, Gélinas C, Manworren R. ASPMN 2019 position statement: pain assessment in the patient unable to self-report. Pain Manag Nurs. 2019;(5):402-403.
468. Mitchell SL, Morris JN, Park PS, Fries BE. Terminal care for persons with advanced dementia in the nursing home and home care settings. J Palliat Med. 2004;7:808-816.
469. Sachs GA, Shega JW, Cox-Hayley D. Barriers to excellent end-of-life care for patients with dementia. J Gen Intern Med. 2004;19:1057-1063.
470. Sampson EL, Thune-Boyle I, Kukkastenvehmas R, et al. Palliative care in advanced dementia: a mixed methods approach for the development of a complex intervention. BMC Palliat Care. 2008;7:8.
471. Triplett P, Black BS, Phillips H, et al. Content of advance directives for individuals with advanced dementia. J Aging Health. 2008;20(5):583-596.
472. Center to Advance Palliative Care. Improving Palliative Care in Nursing Homes. Available at https://media.capc.org/filer_public/95/b8/95b84a49-7151-427d-be72-200b634eed5b/3123_1606_nursinghomereport-rev.pdf. Last accessed October 9, 2024.
474. Lindley LC, Lyon ME. A profile of children with complex chronic conditions at end of life among Medicaid beneficiaries: implications for health care reform. J Palliat Med. 2013;16(11):1388-1193.
475. Sheetz MJ, Bowman MA. Pediatric palliative care: an assessment of physicians' confidence in skills, desire for training, and willingness to refer for end-of-life care. Am J Hosp Palliat Care. 2008;25(2):100-105.
476. Fowler K, Poehling K, Billheimer D, et al. Hospice referral practices for children with cancer: a survey of pediatric oncologists. J Clin Oncol. 2006;24(7):1099-1104.
477. Thompson L, Knapp C, Madden V, et al. Pediatricians' perceptions of and preferred timing for pediatric palliative care. Pediatrics. 2009;123;e777.
478. Johnston DL, Nagel K, Friedman DL, Meza JL, Hurwitz CA, Friebert S. Availability and use of palliative care and end-of-life services for pediatric oncology patients. J Clin Oncol. 2008;26(28):4646-4650.
479. Tomlinson D, Bartels U, Gammon J, et al. Chemotherapy versus supportive care alone in pediatric palliative care for cancer: comparing the preferences of parents and health care professionals. CMAJ. 2011;183(17):E1252-E1258.
480. Crane K. Pediatric palliative care gains recognition. J Natl Cancer Inst. 2011;103(119):1432-1433.
481. Wolfe J, Grier HE, Klar N, et al. Symptoms and suffering at the end of life in children with cancer. N Engl J Med. 2000;342(5):326-333.
482. Kang T, Hoehn KS, Licht DJ, et al. Pediatric palliative, end-of-life, and bereavement care. Pediatr Clin North Am. 2005;52(4):1029-1046.
483. Himelstein B, Hilden JM, Boldt AM, Weissman D. Pediatric palliative care. N Engl J Med. 2004;350(17):1752-1762.
484. American Academy of Pediatrics. Committee on Bioethics and Committee on Hospital Care. Palliative care for children. Pediatrics. 2000;106:351-357.
486. Beale E, Baile WF, Aaron J. Silence is not golden: communicating with children dying from cancer. J Clin Oncol. 2005;23(15):3629-3631.
487. Donnelly JP, Huff SM, Lindsey ML, McMahon KA, Schumacher JD. The needs of children with life-limiting conditions: a healthcare-provider-based model. Am J Hosp Palliat Care. 2005;22:259-267.
488. Graham R, Levetown M, Comeau M. Decision making. In: Carter B, Levetown M, Freibert S (eds). Palliative Care for Infants, Children, and Adolescents: A Practical Handbook. 2nd ed. Baltimore, MD: The Johns Hopkins University Press; 2011.
489. Whitney S, Ethier AM, Fruge E, Berg S, McCullough LB, Hockenberry M. Decision making in pediatric oncology: who should take the lead? The decisional priority in pediatric oncology model. J Clin Oncol. 2006;24(1):160-165.
490. Goldman A, Hewitt M, Collins GS, Childs M, Hain R, United Kingdom Children's Cancer Study Group/Paediatric Oncology Nurses' Forum Palliative Care Working Group. Symptoms in children/young people with progressive malignant disease: United Kingdom Children's Cancer Study Group/Paediatric Oncology Nurses Forum Survey. Pediatrics. 2006;117(6):e1179-1186.
491. Jalmsell L, Kreicbergs U, Onelov E, Steineck G, Henter J-I. Symptoms affecting children with malignancies during the last month of life: a nationwide follow-up. Pediatrics. 2006;117(4):1314-1320.
492. Ullrich C, Mayer OH. Assessment and management of fatigue and dyspnea in pediatric palliative care. Pediatr Clin North Am. 2007;54:735-756.
493. Armendi A, Anghelescu DL. Pain management. In: Pui C (ed). Childhood Leukemias. 3rd ed. New York, NY: Cambridge University Press; 2012.
494. Savedra MC, Holzemer WL, Tesler MD, Wilkie DJ. Assessment of postoperation pain in children and adolescents using the adolescent pediatric pain tool. Nurs Res. 1993;42:5-9.
495. McGrath K, Rosmus C, Canfield C, Campbell MA, Hennigar A. Behaviours caregivers use to determine pain in nonverbal, cognitively impaired children. Develop Med Child Neurol. 1998;40:340-343.
496. Chambers C, Reid GJ, McGrath PJ, Finley GA. Development and preliminary validation of a postoperative pain measure for parents. Pain. 1996;68:307-313.
497. AboutKidsHealth. Tools For Measuring Pain. Available at https://www.aboutkidshealth.ca/Article?contentid=2994&language=English. Last accessed October 9, 2024.
498. Newman CJ, Lolekha R, Limkittikul K, Luangxay K, Chotpitayasunondh T, Chanthavanich P. A comparison of pain scales in Thai children. Arch Dis Child. 2005;90:269-270.
499. Luffy R, Grove SK. Examining the validity, reliability, and preference of three pediatric pain measurement tools in African-American children. Pediatr Nurs. 2003;29:54-59.
500. Garra G, Singer AJ, Taira BR, et al. Validation of the Wong-Baker FACES pain rating scale in pediatric emergency department patients. Acad Emerg Med. 2010;17:50-54.
501. Buccholz M, Karl HW, Pomietto M, Lynn A. Pain scores in infants: a modified infant pain scale vs. visual analog scale. Pain Symp Manag. 1998;15(2):117-124.
502. Monteiro Caran EM, Dias CG, Seber A, Petrilli AS. Clinical aspects and treatment of pain in children and adolescents with cancer. Pediatr Blood Cancer. 2005;45:925-932.
503. Zernikow B, Smale H, Michel E, Hasan C, Jorch N, Andler W. Paediatric cancer pain management using the WHO analgesic ladder: results of a prospective analysis from 2265 treatment days during a quality improvement study. Eur J Pain. 2006;10(7):587-595.
504. World Health Organization. WHO Guidelines for the Pharmacological and Radiotherapeutic Management of Cancer Pain in Adults and Adolescents. Geneva: World Health Organization; 2018.
505. Vargas-Schaffer G. Is the WHO analgesic ladder still valid? Twenty-four years of experience. Can Fam Physician. 2010;56(6):514-517.
507. Anghelescu D, Oakes L, Hinds PS. Palliative care and pediatrics. Anesthesiol Clin North Am. 2006;24(1):145-161.
508. American Academy of Pediatrics. Family pediatrics: report of the Task Force on the Family. Pediatrics. 2003;111(6):1541-1571.
509. Kazak A, Alderfer M, Rourke MT, Simms S, Streisand R, Grossman JR. Posttraumatic stress disorder (PTSD) and posttraumatic stress symptoms (PTSS) in families of adolescent childhood cancer survivors. J Pediatr Psychol. 2004;29(3):211-219.
510. Murray J. Attachment theory and adjustment difficulties in siblings of children with cancer. Issues Ment Health Nurs. 2000;21(2):149-169.
511. Sharpe D, Rossiter L. Siblings of children with a chronic illness: a meta-analysis. J Pediatr Psychol. 2002;27(8):699-710.
512. Grootenhuis M, Last BF. Children with cancer with different survival perspectives: defensiveness, control strategies, and psychological adjustment. Psycho-oncology. 2001;10(4):305-314.
513. Mularski R, Puntillo K, Varkey B, et al. Pain management within the palliative and end-of-life care experience in the ICU. Chest. 2009;135:1360-1369.
514. Truog R, Campbell ML, Curtis JR, et al. Recommendations for end-of-life care in the intensive care unit: a consensus statement by the American College of Critical Care Medicine. Crit Care Med. 2008;36(3):953-963.
515. O'Mahony S, McHenry J, Blank AE, et al. Preliminary report of the integration of a palliative care team into an intensive care unit. Palliat Med. 2010;24(2):154-165.
516. Nelson J. Identifying and overcoming the barriers to high-quality palliative care in the intensive care unit. Crit Care Med. 2006;34(Suppl):S324-S331.
517. Mosenthal A, Murphy PA. Interdisciplinary model for palliative care in the trauma and surgical intensive care unit: Robert Wood Johnson Foundation Demonstration Project for Improving Palliative Care in the Intensive Care Unit. Crit Care Med. 2006;34(Suppl):S399-S403.
518. Thompson BT, Cox PN, Antonelli M, et al. Challenges in end-of-life care in the ICU: statement of the 5th International Consensus Conference in Critical Care: Brussels, Belgium, April 2003: executive summary. Crit Care Med. 2004;32:1781-1784.
519. Mosenthal AC, Murphy PA. Trauma care and palliative care: time to integrate the two? J Am Coll Surg. 2003;197:509-516.
520. Norton S, Hogan LA, Holloway RG, et al. Proactive palliative care in the medical intensive care unit: effects on length of stay for selected high-risk patients. Crit Care Med. 2007;35:1530-1535.
521. Beckstrand RL, Kirchhoff KT. Providing end-of-life care to patients: critical care nurses' perceived obstacles and supportive behaviors. Am J Crit Care. 2005;14:395-403.
522. Sulmasy DP, Terry PB, Weisman CS, et al. The accuracy of substituted judgments in patients with terminal diagnoses. Ann Intern Med. 1998;128:621-629.
523. Covinsky KE, Fuller JD, Yaffe K, et al. Communication and decision-making in seriously ill patients: findings of the SUPPORT project. The Study to Understand Prognoses and Preferences for Outcomes and Risks of Treatments. J Am Geriatr Soc. 2000;48:S187-S193.
524. Campbell M. How to withdraw mechanical ventilation: a systematic review of the literature. AACN. 2007;18:397-403.
525. Davidson JE, Aslakson RA, Long AC, et al. Guidelines for family-centered care in the neonatal, pediatric, and adult ICU. Crit Care Med. 2017;45:103-128.
526. Sihra L, Harris M, O'Reardon C. Using the Improving Palliative Care in the Intensive Care Unit (IPAL-ICU) project to promote palliative care consultation. J Pain Symptom Manage. 2011;42(5):672-675.
528. Schoenborn NL, Janssen EM, Boyd C, et al. Older adults' preferences for discussing long-term life expectancy: results from a national survey. Ann Fam Med. 2018;16:530-537.
1. McCusker M, Jolkvosky M, Ruff R, et al. Palliative Care for Adults. 6th ed. Bloomington, MN: Institute for Clinical Systems Improvement; 2020. Available at https://www.icsi.org/wp-content/uploads/2021/11/PalliativeCare_6th-Ed_2020_v2.pdf. Last accessed October 14, 2024.
2. Medical Services Commission. Palliative Care for the Patient with Incurable Cancer or Advanced Disease. Part 3: Grief and Bereavement. Victoria: British Columbia Medical Services Commission; 2017. Available at https://www2.gov.bc.ca/assets/gov/health/practitioner-pro/bc-guidelines/palliative3.pdf. Last accessed October 14, 2024.
3. American Association of Neuroscience Nurses. Care of the Pediatric Patient with a Brain Tumor. Chicago, IL: American Association of Neuroscience Nurses; 2014. Available at https://bibliosjd.wordpress.com/wp-content/uploads/2015/02/aann13_pbt_e.pdf. Last accessed October 14, 2024.
Mention of commercial products does not indicate endorsement.